The authors summarize and update the most recent knowledge in the field of prevalence, natural history and incidence of Non Alcoholic Fatty Liver Disease (NAFLD) and Non Alcoholic Steatohepatitis (NASH). These novel diseases, firstly recognized at the beginning of the second millennium, arose suddenly to the attention of the clinicians, because they are the hepatic expression of the “so-called” metabolic syndrome. Due to the epidemic burden of obesity, diabetes, and metabolic diseases, NAFLD and NASH will become soon probably the most common hepatic disease worldwide, and they surely will keep busy our future young hepa-tologists.
The term NAFLD is used to describe a condition of fat accumulation in the liver in the absence of excessive alcohol consumption (less than 20 g per day) and any other specific causes of hepatic steatosis.1-5 In the majority of the cases NAFLD is of primary origin and its aetiology is not yet completely understood, even if it is strictly related to the presence of insulin resistance, and thus frequently occurs as the initial part of the metabolic syndrome (MS), and accompany obesity, type 2 diabetes and dyslipidaemia.6-11 Among the secondary causes of NAFLD there are relevant causes, such as nutritional (e.g. malnutrition, rapid weight loss), metabolic (e.g. abetali-poproteinemia, lipodystrophy) and drug-induced (e.g. glucocorticoids, methotrexate, chemotherapics, tamox-ifene, etc.), as well as other conditions (e.g. jejunal diver-ticulitis with bacterial overgrowth, inflammatory bowel disease, occupational exposure). In this review we are focusing our attention only to the epidemiology and natural history of primary NAFLD.
Prevalence of NAFLDNAFLD is now the most common liver disease in the United States and possibly worldwide. Furthermore, the number of affected patients is growing rapidly, and the disease has reached epidemic proportions. However, the true prevalence of NAFLD and Nonalcoholic-Steatohep-atitis (NASH), and their natural history remains incompletely deuned. Furthermore, there are no data on the change in prevalence of NAFLD within a population over time, and there are no data on incidence of NAFLD. The reported prevalence of NAFLD varies according to the population studied, and the diagnostic criteria used.12-14 Usually population-based studies provide better estimates of the prevalence of NAFLD in the general population compared with autopsy studies, hospital series or studies performed exclusively in obese populations, but few such studies have been reported to date.15-47 However, the diagnosis of NAFLD within the population studies are usually made by ultrasonography (US), that allows detecting moderate and severe steatosis with a fair sensitivity and specificity only when fat on liver biopsy exceeds 33%. More sensitive techniques, including MR imaging and spectroscopy, are hindered by expense and lack of feasibility in large populations. The American Association for the Study of Liver Diseases (AASLD) set the limit for the diagnosis of NAFLD at fat accumulation in the liver of at least 5 to 10% by weight. Therefore, liver biopsy is still considered as the gold standard, but is limited by sampling and interpretation error besides its cost and not applicability in population-based studies for both ethical and practical reasons.
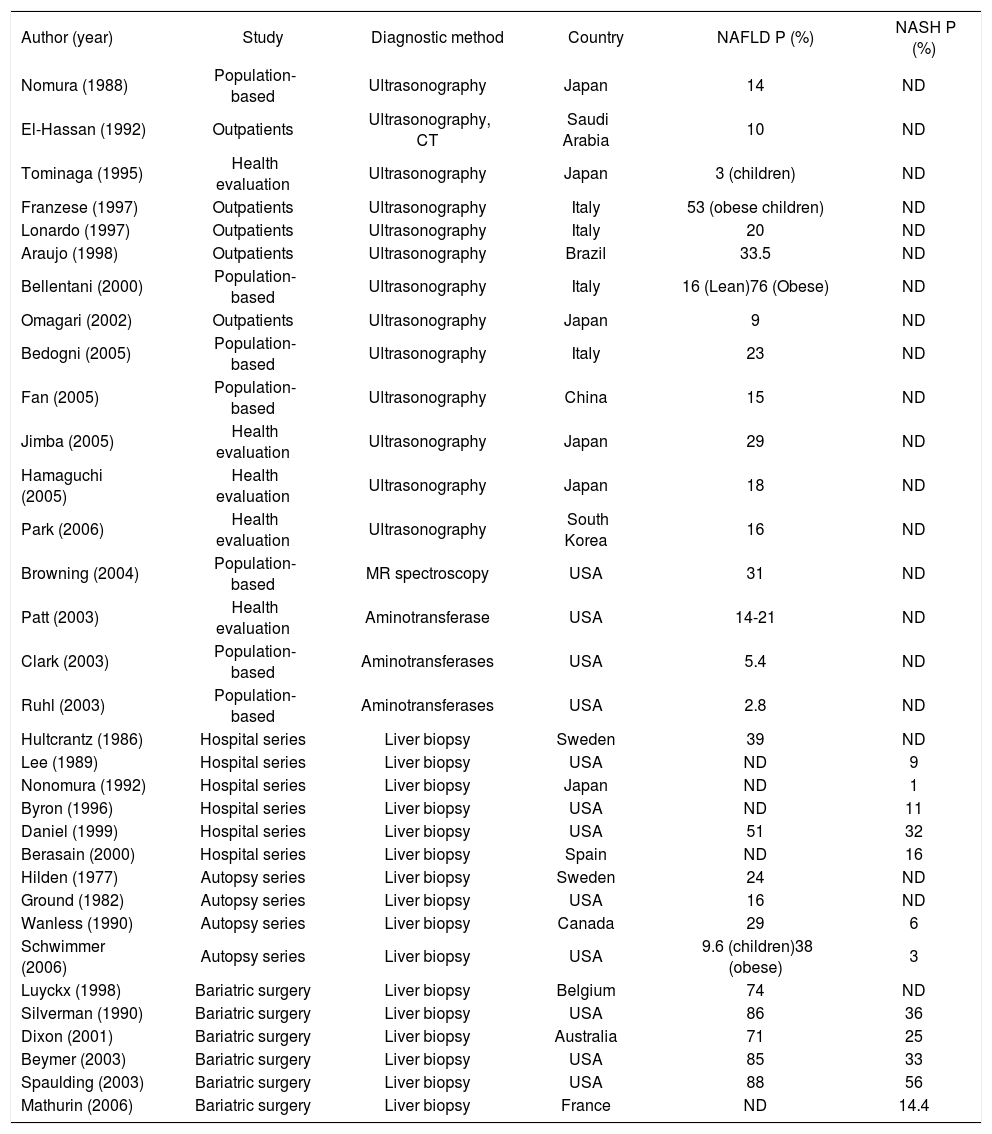
Table I summarizes the results of several studies on the prevalence of NAFLD/NAS H.12-44 Proton MR spectro-scopy and 1H-MRS are considered the most accurate non-invasive methods for measuring liver fat, but again unpractical and too expensive to be applied on a large scale. Recently both the Dallas Heart Study (a population-based cohort study performed in an ethnically diverse community in the USA) and our Dionysos study (a population-based cohort study performed in 2 community of Northern of Italy) reported that 30% of adult Americans and 25% of adult Italians have NAFLD. This indicates that over 70 million adult Americans and 15 million adult Italians suffer from NAFLD. In that studies 79 and 55% of patients with NAFLD had normal aminotransferase levels, suggesting that studies using liver enzymes as a surrogate for NAFLD highly underestimate the prevalence of NAFLD.
Prevalence (=P) of Nonalcoholic Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH) according to different type of studies. ND= not determined. See reference from 12 to 44.
| Author (year) | Study | Diagnostic method | Country | NAFLD P (%) | NASH P (%) |
|---|---|---|---|---|---|
| Nomura (1988) | Population-based | Ultrasonography | Japan | 14 | ND |
| El-Hassan (1992) | Outpatients | Ultrasonography, CT | Saudi Arabia | 10 | ND |
| Tominaga (1995) | Health evaluation | Ultrasonography | Japan | 3 (children) | ND |
| Franzese (1997) | Outpatients | Ultrasonography | Italy | 53 (obese children) | ND |
| Lonardo (1997) | Outpatients | Ultrasonography | Italy | 20 | ND |
| Araujo (1998) | Outpatients | Ultrasonography | Brazil | 33.5 | ND |
| Bellentani (2000) | Population-based | Ultrasonography | Italy | 16 (Lean)76 (Obese) | ND |
| Omagari (2002) | Outpatients | Ultrasonography | Japan | 9 | ND |
| Bedogni (2005) | Population-based | Ultrasonography | Italy | 23 | ND |
| Fan (2005) | Population-based | Ultrasonography | China | 15 | ND |
| Jimba (2005) | Health evaluation | Ultrasonography | Japan | 29 | ND |
| Hamaguchi (2005) | Health evaluation | Ultrasonography | Japan | 18 | ND |
| Park (2006) | Health evaluation | Ultrasonography | South Korea | 16 | ND |
| Browning (2004) | Population-based | MR spectroscopy | USA | 31 | ND |
| Patt (2003) | Health evaluation | Aminotransferase | USA | 14-21 | ND |
| Clark (2003) | Population-based | Aminotransferases | USA | 5.4 | ND |
| Ruhl (2003) | Population-based | Aminotransferases | USA | 2.8 | ND |
| Hultcrantz (1986) | Hospital series | Liver biopsy | Sweden | 39 | ND |
| Lee (1989) | Hospital series | Liver biopsy | USA | ND | 9 |
| Nonomura (1992) | Hospital series | Liver biopsy | Japan | ND | 1 |
| Byron (1996) | Hospital series | Liver biopsy | USA | ND | 11 |
| Daniel (1999) | Hospital series | Liver biopsy | USA | 51 | 32 |
| Berasain (2000) | Hospital series | Liver biopsy | Spain | ND | 16 |
| Hilden (1977) | Autopsy series | Liver biopsy | Sweden | 24 | ND |
| Ground (1982) | Autopsy series | Liver biopsy | USA | 16 | ND |
| Wanless (1990) | Autopsy series | Liver biopsy | Canada | 29 | 6 |
| Schwimmer (2006) | Autopsy series | Liver biopsy | USA | 9.6 (children)38 (obese) | 3 |
| Luyckx (1998) | Bariatric surgery | Liver biopsy | Belgium | 74 | ND |
| Silverman (1990) | Bariatric surgery | Liver biopsy | USA | 86 | 36 |
| Dixon (2001) | Bariatric surgery | Liver biopsy | Australia | 71 | 25 |
| Beymer (2003) | Bariatric surgery | Liver biopsy | USA | 85 | 33 |
| Spaulding (2003) | Bariatric surgery | Liver biopsy | USA | 88 | 56 |
| Mathurin (2006) | Bariatric surgery | Liver biopsy | France | ND | 14.4 |
NAFLD has also reached epidemic proportions among populations typically considered at ‘‘low risk’’ for this liver condition, with a prevalence in China and Japan of 15 and 14%, respectively, among adults. The clinical implications of this alarming prevalence of NAFLD are derived from the fact that this liver condition may progress to endstage liver disease and liver cancer. The prevalence of NAFLD among children is unknown, but some data indicate that 2.6-9.6% of children have NAFLD, increasing up to 38-53% among obese children (Table I).
NAFLD is more frequent among obese subjects (75%) compared to controls (16%), and among patients with type 2 diabetes (34-74%), whereas it is an almost universal finding in obese patients with type 2 diabetes. The prevalence of NAFLD is also more prevalent in Hispanics and Asian-Indians than in white Americans or Black, and it is normally increasing with age. Recent data indicate a doubling of the prevalence in children: from 2.6% a decade ago to 5% today in normal-weight, and 38% or 48% in obese and diabetic children respectively. All these prevalences makes NAFLD the most common chronic liver disease in the Western societies.
Natural history, mortality and incidence of NAFLDData on natural history and mortality of NAFLD/ NASH are contradictory and the study available in the literature are not conclusive.48-64 NAFLD progresses slowly to NASH and cirrhosis or HCC over many years or decades, therefore the natural history is difficult to measure in short-time interval. Patients with simple, bland steatosis seem to have a more benign prognosis. For instance, a Danish study by Dam-Larsen and co-workers65 of a cohort of 109 predominantly morbidly obese subjects, followed for nearly 17 years, found the incidence of cirrhosis to be less than 1%, and during the follow-up the mortality of people with fatty liver did not differ from the general population mortality. Conversely, patients with cryptogenic cirrhosis due to NASH have a worse prognosis, as demonstrated in some recent studies where 9-26% of patients died within 4-10 years of follow-up, with most causes of death related to end-stage liver disease.66-70 Using a community-based sample, Adams et al.66-67 demonstrated a lower survival among persons with NAFLD compared to the general population. In a different study, Ekstedt et al.68 showed that persons with NAFLD, in particular those with the subtype of NASH, had a reduced survival when compared with a matched reference population. Both these studies however may not necessarily reflect the general population. In the Dionysos cohort, after 8.5 years of follow up, we found that people with alcohol use or abuse remains still the main risk factor for progression of fatty liver to end-stage liver disease.23,69 The last study available, published by Ong et al.70 that used the NHANES III data-base, showed that persons with NAFLD have a higher likelihood of dying of a liver-related complication compared to those without NAFLD or liver disease. This risk was independent of obesity or the presence of diabetes mellitus, the latter being associated with higher rates of liver-related deaths. However, a great limitation of this study is the use of elevated serum aminotransferases as a marker of NAFLD, which underestimates the true prevalence of NAFLD of more than 50%, as already reported above.
Among the various causes of death in people with NAFLD, cardiovascular disease and malignancy seems to be the most important causes as found by Ong et al.,70 but also by others previously published cohort studies. For this reason, NAFLD is now believed to be the hepatic manifestation of the metabolic syndrome, and an independent predictor of cardiovascular morbidity and mortality.
Overall, a diagnosis of NAFLD is associated with a shorter survival than expected for the general population of the same age and gender, and the higher mortality is mainly due to cardiovascular disease (CVD). A strong association between elevated levels of serum liver enzymes and increased CVD risk has also been reported by numerous population-based studies, such as the Hoorn Study, the Framingham Heart Study and the Valpolicella Heart Diabetes Study,71-73 where mildly elevated levels of liver enzymes were independently associated with an increased CVD mortality rate in both sexes, independently of traditional risk factors and components of the metabolic syndrome.
Long-term data that clearly show that NAFLD progress to end-stage liver disease are lacking, even if some short-term data suggest that NAFLD underlies a substantial proportion of cases of cryptogenic cirrho-sis74,75 of patients with cryptogenic cirrhosis, 50-73% are obese or suffer from diabetes. Further, the presence of NAFLD increases disease severity and progression in oth-erliver diseases including chronic hepatitis C infection, alcoholic liver disease and hemochromatosis.
The incidence of NAFLD remains unknown because no prospective studies have been conducted. The only data available are the one referring to the incidence of fatty liver (FL) in the Dionysos cohort, where we found that FL regressed in nearly 1 of every 2 cases and had a substantially benign course, and ethanol intake was the most important risk factor for FL remission and inci-dence.23,76,77 The incidence and remission rates of FL after 8.5 years of follow up in the Dionysos cohort were 18.5 and 55.0 per 1,000 person-years; every increase of 20 g/ day of ethanol intake at baseline was associated with a 17% increase in the rate of incident FL.76
ConclusionsNAFLD has become a common diagnosis in clinical practice of several medical specialties, and its prevalence in the general population is increasing together with obesity, type 2 diabetes and the metabolic syndrome. Bland steatosis remains stable for a number of years and will probably never progress in many cases. On the contrary in those patients with NASH, whose disease progresses to advanced fibrosis and cirrhosis, most liver and hearth-related morbidity and mortality are observed. Prospective studies with long-term follow-up are necessary to better define the natural history of NAFLD and its incidence both in the general populations and in speciuc groups. Genetic studies are also necessary to determine to what extent the genetic background predisposes to NAFLD development and progression to advanced liver disease.