Introduction. A systematic bias against women, resulting from the use of creatinine as a measure of renal function, has been identified in Model for End-stage Liver Disease (MELD)-based liver allocation. Correction of this bias by calculation of female creatinine levels using the Modification of Diet in Renal Disease (MDRD) formula has been suggested.
Material and methods. A cohort of 639 cirrhotic candidates for first-time liver transplantation was studied. Creatinine levels were corrected for gender using the MDRD formula. The accuracy of MELD, with or without creatinine correction, to predict 3- and 6-month mortality after inclusion in a transplant waiting list was estimated.
Results. Women exhibited significantly lower creatinine levels, glomerular filtration rate, and MELD scores than men. After creatinine correction, female MELD scores had a mean increase of 1.1 points. Creatinine correction yielded an increase of 3 points in the MELD score in 15.2% of patients, 2 points in 22.4%, and 1 point in 17.6% of patients. The likelihood of death at 3 and 6 months after enrollment in the transplant waiting list was similar in males and females and the likelihood of receiving a transplant, as assessed by Kaplan-Meier survival curves, was also similar in males and females.
Conclusion. The survival or the likelihood of receiving a transplant while on the waiting list were similar in men and women in both pre- and post-MELD eras and creatinine correction did not increase the accuracy of the MELD score in estimating 3- and 6-month mortality in female candidates for liver transplantation.
The Model for End-stage Liver Disease (MELD)1,2 is a robust predictor of 3-month mortality in liver transplantation candidates.3,4 Three variables are used to calculate the MELD score, namely serum bilirubin, International Normalized Ratio (INR), and serum creatinine.2 These objective measures are easily obtained and updated to reflect disease progression. In Brazil, the MELD score was introduced for allocation purposes in 2006.5
Despite the many improvements in organ allocation following adoption of the MELD, some patients are still underserved.6,9 In the United States, Moylan, et al.10 have reported that even after adoption of the MELD, women continued to present a greater probability of dying or being too sick to undergo liver transplantation, and were also less likely to undergo liver transplantation within 3 years of being waitlisted as compared to men.10 As pointed out by Cholongitas, et al.11 this may in part result from a systematic bias inherent in the MELD-based organ allocation system. This bias concerns the assessment of renal function based on serum creatinine, as women have lower creatinine levels than men with similar renal function expressed as glomerular filtration rate (GFR). This difference is not taken into account by MELD, leading to the possibility of a woman with worse renal function, recognized as an adverse prognostic factor, having the same MELD score as a man. These authors therefore propose a correction of creatinine levels to “equalize” males and females before calculation of MELD scores. The present study aims:
- 1.
To evaluate whether the correction of creatinine as proposed by Cholongitas, et al.11 increases MELD score in women.
- 2.
To assess the accuracy of MELD score with and without creatinine correction in predicting 3-and 6-month mortality in male and female candidates for deceased-donor liver transplantation.
- 3.
To compare the performance of these scores for prediction of mortality 3 and 6 months after inclusion in a transplant candidate registry.
- 4.
To determine whether sex-based disparities exist in access to liver transplantation in southern Brazil after introduction of MELD scores for organ allocation.
Cirrhotic patients aged 18 years or older listed as candidates for first-time liver transplant from deceased donors at the Liver Transplantation Group at Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre between January 2001 and December 2008 were eligible for the study. The exclusion criteria were: being a candidate for combined liver-kidney transplant or liver retransplantation, a history of familial amyloid polyneuropathy or primary hyperoxaluria.
Patients with hepatocellular carcinoma were eligible if added to the registry before June 2006, when MELD-based allocation was adopted; hepatocellular carcinoma patients listed after June 2006 were not eligible because their MELD scores were upgraded. No United Network for Organ Sharing (UNOS)-based MELD exception rules were used. Patients with insufficient data or who received follow-up at a different hospital were also excluded. None of the patients was on dialysis. Of 698 eligible patients, 59 were excluded from analysis due to incomplete data, leaving a total sample size of 639.
The study was approved by the local Ethics Committee (Institutional Review Board-equivalent) and was conducted in accordance with the provisions of the Declaration of Helsinki.
Creatinine levels were measured with the Jaffé reaction (Cobas Integra 700 Roche). Serum bilirubin and INR were measured using the Evelin-Malloy reaction (Cobas Integra 700 Roche) and a viscometer (STA Compact Diagnostica STAGO), respectively.
To calculate the scores, we employed the results of tests performed as part of standard of care, at the date of inclusion in the registry or the closest tests to the date of inclusion. The following equation was used for calculation of MELD:12 3.8 logn serum bilirubin (mg/dL) + 11.2 logn INR + 9.6 logn serum creatinine (mg/dL) + 6.4. Serum bilirubin, INR and creatinine values lower than 1 were rounded to 1 to avoid negative scores. Scores were not capped at 40. Hepatocellular carcinoma patients did not have their score upgraded.
GFR was calculated using the Modification of Diet in Renal Disease (MDRD) formula:
- •
MDRD for males: GFR (mL/min/1.73 m2) = 186 × (creatinine/88.4)–1.154 × (age)–0.203 × (1.210 if black) (SI units)
- •
MDRD for females: GFR (mL/min/1.73 m2) = 0.742 × 186 × (creatinine/88.4)–1.154 x (age)–0.203 × (1.210 if black) (SI units)
Using the strategy proposed by Cholongitas, et al.11 in the present study the male MDRD formula was used to derive a corrected creatinine measure (CrC) for female participants. In other words, the MDRD was applied twice for each woman: once to calculate the GFR based on the actual serum creatinine level, and a second time to calculate CrC based on GFR. MELD was calculated separately, using both creatinine values, generating scores which were then compared.
The primary endpoints, death due to liver failure and liver transplantation, were recorded until 31 December 2008. Three- and 6-month mortality after inclusion in the registry was also determined.
Statistical analysisThe Statistical Package for the Social Sciences (v. 17 for Windows) was used for all analyses (SPSS Inc., Chicago, Illinois, USA). Quantitative variables were expressed as means ± standard deviation or medians (interquartile range). The chi-square or Fisher’s exact test (two-tailed) were used for categorical data. The Mann-Whitney or paired t test were used, as appropriate, for continuous variables. To evaluate the accuracy of the MELD and corrected-MELD in predicting mortality between males and females, c-statistics was used, with calculation of the area under a receiver operating characteristic (ROC) curve. The method of Hanley & McNeil13 was used to compare ROC curves. The outcomes were measured at 3 and 6 months. When evaluating the accuracy of the scores for mortality prediction, subjects transplanted before 3 and 6 months were removed from the calculation. We further analyzed whether after the introduction of MELD scores for organ allocation women were less likely to be transplanted or die on the waiting list. Kaplan-Meier curves were used to analyze survival and probability of receiving a transplant. Pearson’s coefficient was used to evaluate correlations between continuous variables. For all tests, p-values below 0.05 were considered to be statistically significant.
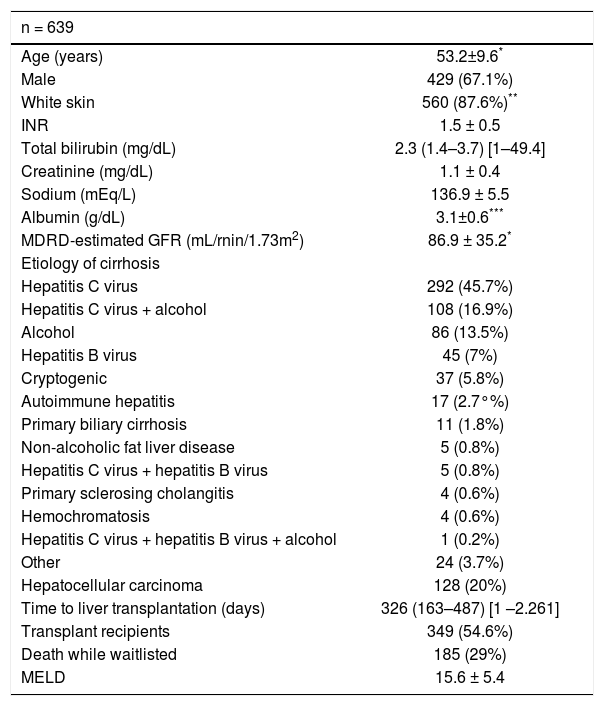
ResultsThe characteristics of patients are shown in table 1. Most patients were male (67.1%), had white skin (87.6%), and were HCV carriers (62.7%); 20.0% had hepatocellular carcinoma. At inclusion in the registry, mean MELD was 15.6 ± 5.4, while MDRD-estimated GFR was 86.9 ± 35.2. The overall mortality rate while waitlisted was 29%, and the median time until liver transplantation was 326 days, with no gender differences in time until transplantation.
Demographic characteristics of patients.
| n = 639 | |
|---|---|
| Age (years) | 53.2±9.6* |
| Male | 429 (67.1%) |
| White skin | 560 (87.6%)** |
| INR | 1.5 ± 0.5 |
| Total bilirubin (mg/dL) | 2.3 (1.4–3.7) [1–49.4] |
| Creatinine (mg/dL) | 1.1 ± 0.4 |
| Sodium (mEq/L) | 136.9 ± 5.5 |
| Albumin (g/dL) | 3.1±0.6*** |
| MDRD-estimated GFR (mL/rnin/1.73m2) | 86.9 ± 35.2* |
| Etiology of cirrhosis | |
| Hepatitis C virus | 292 (45.7%) |
| Hepatitis C virus + alcohol | 108 (16.9%) |
| Alcohol | 86 (13.5%) |
| Hepatitis B virus | 45 (7%) |
| Cryptogenic | 37 (5.8%) |
| Autoimmune hepatitis | 17 (2.7°%) |
| Primary biliary cirrhosis | 11 (1.8%) |
| Non-alcoholic fat liver disease | 5 (0.8%) |
| Hepatitis C virus + hepatitis B virus | 5 (0.8%) |
| Primary sclerosing cholangitis | 4 (0.6%) |
| Hemochromatosis | 4 (0.6%) |
| Hepatitis C virus + hepatitis B virus + alcohol | 1 (0.2%) |
| Other | 24 (3.7%) |
| Hepatocellular carcinoma | 128 (20%) |
| Time to liver transplantation (days) | 326 (163–487) [1 –2.261] |
| Transplant recipients | 349 (54.6%) |
| Death while waitlisted | 185 (29%) |
| MELD | 15.6 ± 5.4 |
INR: international normalized ratio. MDRD: Modification of Diet in Renal Disease. MELD: Model for End-Stage Liver Disease. Results are expressed as mean ± standard deviation, median (P25-P75) [min-max], or percentage (%).
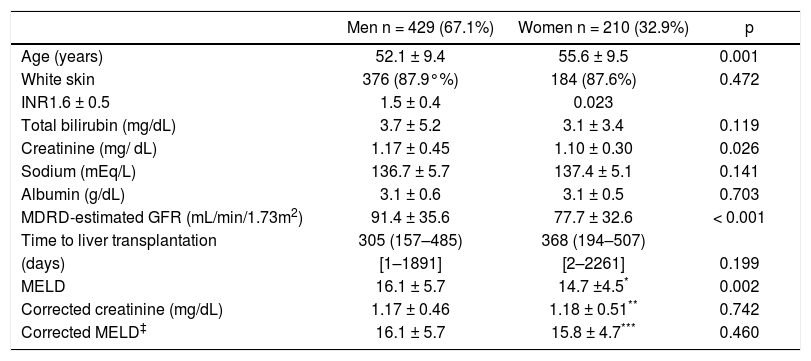
Table 2 shows that at the time of enrollment women were older than men (55.6 ± 9.5 vs. 52.1 ± 9.5; p = 0.001), had significantly lower creatinine levels (1.10 ± 0.30 vs. 1.17 ± 0.46; p = 0.026), and exhibited lower GFR as calculated by the MDRD formula (77.7 ± 32.6 vs. 91.4 ± 35.6; p < 0.001). Men had higher baseline INR (1.6 ± 0.5 vs. 1.5 ± 0.4; p = 0.023).
Demographic and clinical characteristics of male and female candidates for liver transplantation.
| Men n = 429 (67.1%) | Women n = 210 (32.9%) | p | |
|---|---|---|---|
| Age (years) | 52.1 ± 9.4 | 55.6 ± 9.5 | 0.001 |
| White skin | 376 (87.9°%) | 184 (87.6%) | 0.472 |
| INR1.6 ± 0.5 | 1.5 ± 0.4 | 0.023 | |
| Total bilirubin (mg/dL) | 3.7 ± 5.2 | 3.1 ± 3.4 | 0.119 |
| Creatinine (mg/ dL) | 1.17 ± 0.45 | 1.10 ± 0.30 | 0.026 |
| Sodium (mEq/L) | 136.7 ± 5.7 | 137.4 ± 5.1 | 0.141 |
| Albumin (g/dL) | 3.1 ± 0.6 | 3.1 ± 0.5 | 0.703 |
| MDRD-estimated GFR (mL/min/1.73m2) | 91.4 ± 35.6 | 77.7 ± 32.6 | < 0.001 |
| Time to liver transplantation | 305 (157–485) | 368 (194–507) | |
| (days) | [1–1891] | [2–2261] | 0.199 |
| MELD | 16.1 ± 5.7 | 14.7 ±4.5* | 0.002 |
| Corrected creatinine (mg/dL) | 1.17 ± 0.46 | 1.18 ± 0.51** | 0.742 |
| Corrected MELD‡ | 16.1 ± 5.7 | 15.8 ± 4.7*** | 0.460 |
INR: international normalized ratio. MDRD: Modification of Diet in Renal Disease. MELD: Model for End-Stage Liver Disease. Results are expressed as mean ± standard deviation, median (P25-P75) [min-max], or percentage (%).
Using the strategy proposed by Cholongitas, et al.11 a corrected creatinine value was obtained for each female patient to calculate GFR. After creatinine correction, the difference between men and women lost significance.
At enrollment in the waiting list, men had significantly higher MELD scores than women (16.1 ± 5.7 vs. 14.7 ± 4.5 vs. p = 0.002). However, this difference was abolished following creatinine correction.
Recalculating the MELD score with CrC in women led to a mean increase of 1.1 point. In 32 patients (15.2%), a 3-point difference was observed between the actual and corrected MELD; a 2-point difference was observed in 47 women (22.4%) and a 1-point difference in 37 patients (17.6%). The increase was noted for all MELD score categories.
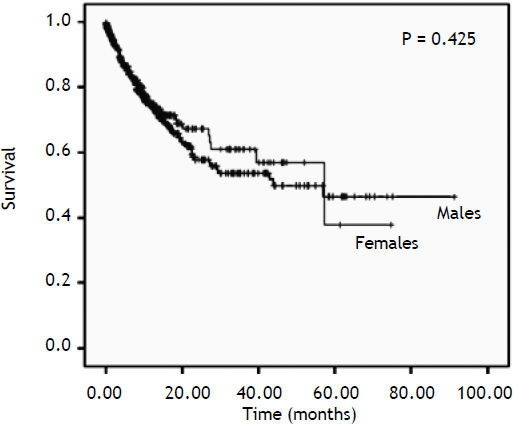
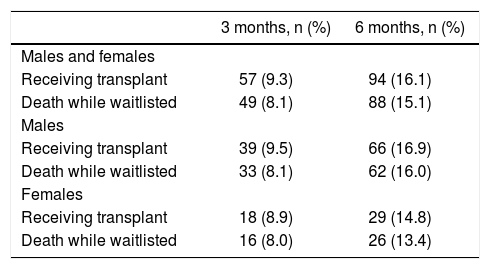
Nevertheless, Table 3 shows that the likelihood of death at 3 and 6 months after enrollment in the transplant waiting list (Kaplan-Meier) was similar in males and females. In addition, the likelihood of receiving a transplant, as assessed by Kaplan-Meier survival curves, was similar in males and females. Figure 1 shows the analysis of survival for both genders (p = 0.425).
Three- and 6-month mortality or transplantation (Kaplan-Meier).*
| 3 months, n (%) | 6 months, n (%) | |
|---|---|---|
| Males and females | ||
| Receiving transplant | 57 (9.3) | 94 (16.1) |
| Death while waitlisted | 49 (8.1) | 88 (15.1) |
| Males | ||
| Receiving transplant | 39 (9.5) | 66 (16.9) |
| Death while waitlisted | 33 (8.1) | 62 (16.0) |
| Females | ||
| Receiving transplant | 18 (8.9) | 29 (14.8) |
| Death while waitlisted | 16 (8.0) | 26 (13.4) |
Data expressed as absolute number and percentage (%).
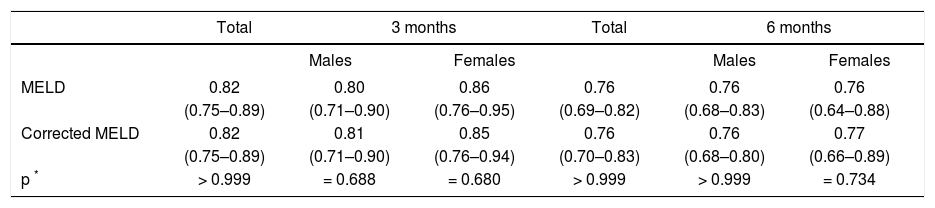
The ability to predict death after 3 and 6 months with MELD and CrC-MELD, according to ROC curve analysis, is shown in Table 4. There were no statistical differences in the accuracy of the different scores.
ROC analysis of 3- and 6-month mortality (95%CI) in males and females according to MELD and corrected MELD.
| Total | 3 months | Total | 6 months | |||
|---|---|---|---|---|---|---|
| Males | Females | Males | Females | |||
| MELD | 0.82 | 0.80 | 0.86 | 0.76 | 0.76 | 0.76 |
| (0.75–0.89) | (0.71–0.90) | (0.76–0.95) | (0.69–0.82) | (0.68–0.83) | (0.64–0.88) | |
| Corrected MELD | 0.82 | 0.81 | 0.85 | 0.76 | 0.76 | 0.77 |
| (0.75–0.89) | (0.71–0.90) | (0.76–0.94) | (0.70–0.83) | (0.68–0.80) | (0.66–0.89) | |
| p * | > 0.999 | = 0.688 | = 0.680 | > 0.999 | > 0.999 | = 0.734 |
ROC: Receiver operating characteristic. 95%CI: 95% confidence interval. MELD: Model for End-Stage Liver Disease.
When analyzing survival and probability of receiving a transplant after the introduction of MELD scores for organ allocation through Kaplan-Meier curves, no statistical difference was found between males and females in both the pre-MELD (January 1, 2001-June 28, 2006) and post-MELD (June 29, 2006-December 31, 2008) eras (data not shown).
DiscussionThe possibility that women are disadvantaged relative to men in terms of liver allocation using the MELD score has been studied internationally.7,8,14 However, this is the first study to evaluate the impact of serum creatinine on MELD score results in a population of Brazilian patients on the waiting list for a first-time liver transplant, investigating the existence of a systematic bias against women, as suggested by Cholongitas, et al.11
At the time of enrollment women were older than men, making it difficult to interpret some findings given that age influences creatinine and is an independent predictor of waitlist mortality. Women also had significantly lower creatinine levels than men, while exhibiting lower GFR as calculated by the MDRD formula, supporting that serum creatinine is not adequate for estimating renal function.15–17
Using the strategy proposed by Cholongitas, et al.,11 a corrected creatinine value was obtained for each female patient to calculate GFR. After creatinine correction, the difference between men and women lost significance.
Despite well-known limitations, MDRD formula is considered to be more accurate than other methods for estimation of GFR from creatinine in patients with cirrhosis.18 It estimates the rate of glomerular filtration for the mean adult body surface area (1.73 m2) rather than for body weight, which might be advantageous in cirrhotic patients with ascites. The MDRD has a correction factor of 0.742 for women, indicating that the GFR is lower in women than men of a similar age and skin color with similar serum creatinine levels.
At enrollment in the waiting list, men had significantly higher MELD scores than women, explained in part by their higher creatinine values. However, this difference was abolished following recalculation of MELD scores using CrC. Using CrC to calculate MELD scores would translate into a 3-point increase in 32 (15.2%) women, a 2-point increase in 47 (22.4%) women, and a 1-point increase in 37 (17.6%) women; these increases would be observed for all categories of the actual MELD score. These data partially agree with the findings reported by Cholongitas, et al.,11 who observed 3- or 2-point increases in 65% of female patients, with 3-point increase observed mainly in women with a MELD score below 19. These observations could be important in the context of an objective allocation system that attempts to prioritize the sickest patients, and in which a 1-point difference suffices to decide allocation.
The scores employed in the present analysis were those calculated at inclusion in the waiting list. Therefore, they do not necessarily reflect the scores at death or transplantation. Although MELD was developed to estimate the probability of death at 3 and 6 months, it may predict death over longer periods of time.4
Another potential bias in our analysis is that adjustments for potential confounders, such as coexisting cirrhosis-related complication markers of renal dysfunction in liver disease (e.g. ascites and hyponatremia), were not made. In addition, a problem, not often recognized by hepatologists, is that calculation of the scores may be influenced by laboratory test variability.19
ConclusionCorrected creatinine increased the MELD score in at least 1 point in 55.2% of women on the waiting list for liver transplantation. Although statistically significant, the differences between the modified MELD and MELD were not clinically significant. The survival or the likelihood of receiving a transplant while on the waiting list in our cohort was similar in men and women in both the pre- and post-MELD eras and the method proposed by Cholongitas, et al.11 did not increase the accuracy of the MELD score in estimating 3- and 6-month mortality in female candidates for liver transplantation in southern Brazil. We must consider that organ allocation may also be influenced by factors other than those evaluated in this study, such as organ size matching, and that in the MELD-based allocation system, MELD score is recalculated and all patients are prioritized according to the last, rather than the baseline, MELD score. Furthermore, the small number of patients studied may have contributed to these findings. Thus, it would be important to verify whether these findings can be repeated in other centers with a larger number of patients.
AcknowlegmentsThe authors would like to thank Dr. Mário B Wagner, for his assistance in statistical analyses; and the Liver Transplant Group: Eduardo Soares Schlindwein, Guillermo Kiss, Ian Leipnitz, Marcos Mucenic, Marcus Vinícius Osório da Silveira, Mário Henrique de Mattos Meine.
Abbreviations- •
CrC: Corrected creatinine measure.
- •
GFR: Glomerular filtration rate.
- •
HCV: Hepatitis C virus.
- •
INR: International normalized ratio.
- •
MELD: Model for End-stage Liver Disease.
- •
MDRD: Modification of Diet in Renal Disease.
- •
ROC: Receiver operating characteristic.
- •
SPSS: Statistical Package for the Social Sciences.
- •
UNOS: United Network for Organ Sharing.
The study did not receive financial support or grants.