Considered as a healthcare quality indicator, hospital readmissions in decompensated cirrhosis predispose the patients and the society to physical, social and economic distresses. Few studies involving North American cohorts have identified different predictors. The aim of this study was to determine and validate the predictors of 1-month and 3-months readmission in an Asian cohort.
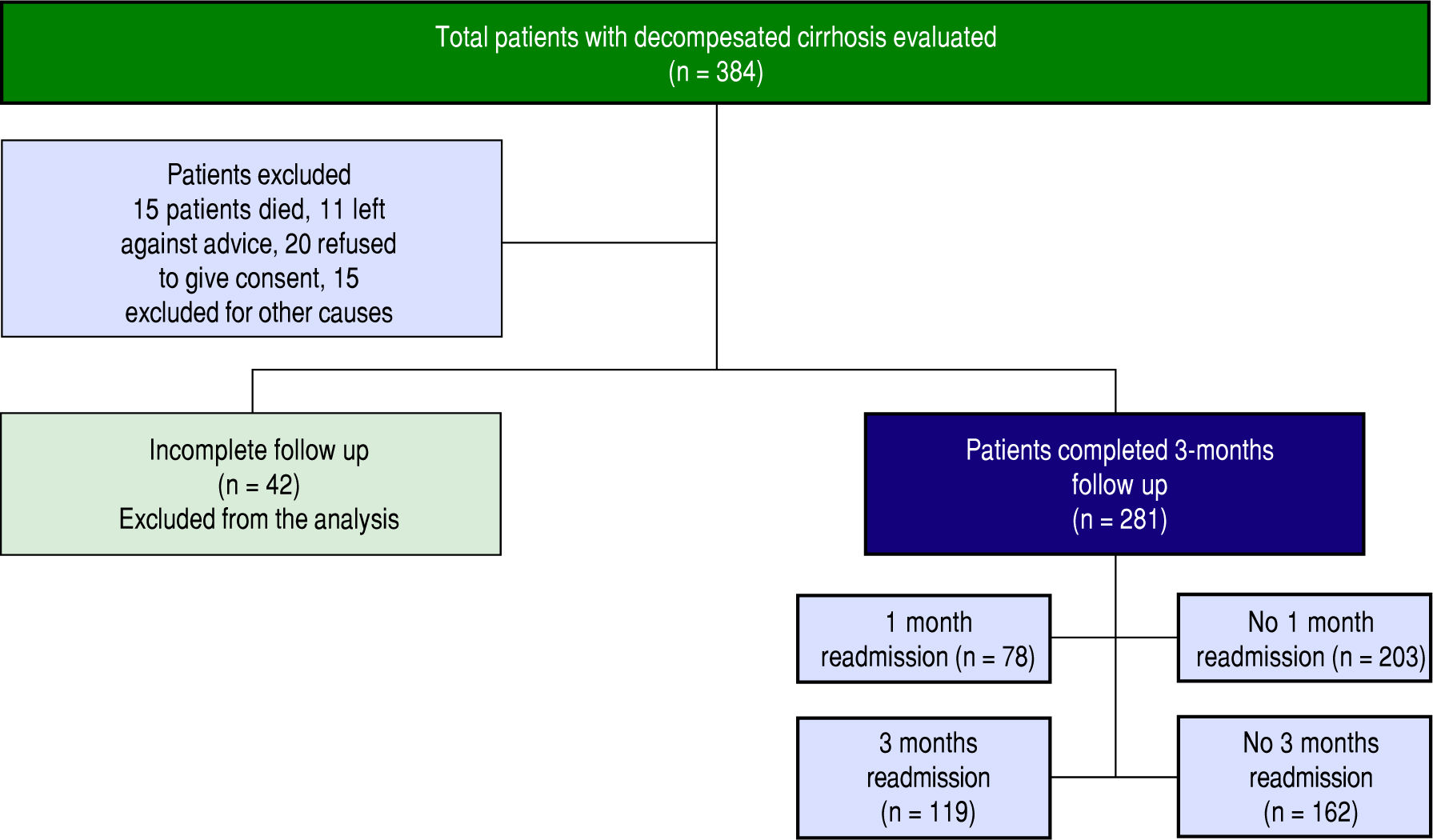
Material and methods.We prospectively studied 281 hospitalised patients with decompensated cirrhosis at a large tertiary care public hospital in India between August 2014 and August 2016 and followed them for 3 months. Data regarding demographic, laboratory and disease related risk factors were compiled. We used multivariate logistic regression to determine predictors of readmission at 1-month and 3-months and receiver operating curves (ROC) for significant predictors to obtain the best cut-offs.
Results1-month and 3-months readmission rates in our study were 27.8% and 42.3%, respectively. Model for End stage Liver Disease (MELD) score at discharge (OR:1.24, p < 0.001) and serum sodium (OR:0.94, p-0.039) independently predicted 1-month and MELD score (OR:1.11, p-0.003), serum sodium (OR:0.94, p-0.027) and male gender (OR:2.19, p-0.008) independently predicted 3-months readmissions. Neither aetiology nor complications of cirrhosis emerged as risk factors. MELD score >14 at discharge and serum sodium < 133 mEq/L best predicted readmissions; MELD score being a better predictor than serum sodium (p - 0.0001).
ConclusionsHigh rates of early and late readmissions were found in our study. Further, this study validated readmission predictors in Asian patients. Structured interventions targeting this risk factors may diminish readmissions in decompensated cirrhosis.
Early hospital readmission has been considered as a surrogate marker of quality of any healthcare delivery system.1 Hospital readmissions not only put financial burden on patients and their families but employ significant amount of healthcare resources, physician consultations and economic as well as social burden on the society.2 Readmissions usually result from relapsing nature of the underlying disease, complications during previous hospitalisation, miscommunication between discharging hospital and physicians giving outpatient care and patient noncompliance. Therefore evaluation of the causes and thereby their prevention are of utmost importance. Sufficient amount of data have been produced delineating pre-dictors of readmissions in chronic heart failure and chronic obstructive lung disease and their implementation in patient care have reduced the number of readmissions enormously.3,4
Cirrhosis of liver is a chronic progressive disorder and an end result for various chronic liver diseases. Decompensated chronic liver disease has been reported to be the third most common cause of death in USA in patients aged 45 to 64 years5 and carries 10-fold higher risk of death as compared to general population.6 Apart from death, it is also one of the leading causes of morbidity requiring frequent hospitalizations and readmissions.7 Studies have shown readmission rates of 20-37% within 1-month and upto 53% at 3-months.8-10
A handful of studies have come up in the last five years evaluating predictors of early readmissions in cirrhosis.8-12 However, all of them have been conducted in the North America with majority of population being Caucasian and most of them are single center studies showing divergent results. Severity of cirrhosis, presence of diabetes and nosocomial infections predicted early readmissions in one study,10 whereas other brought Model for End stage Liver Disease (MELD) score, serum sodium and number of medications to be associated with frequent readmissions.9 Also there is little uniformity in the time duration upto which readmissions have been considered as early. Few have taken 30 days as the cut-off,8,9,11 while some have measured 3-months readmission rates producing inconsistent results.10
Our study is a prospective study to evaluate whether the severity of liver disease, aetiology of cirrhosis and complications during initial hospitalisation for decompensated cirrhosis predict early (1-month) or late (3-month) readmissions. It will also highlight the subtle differences, if any, in risk factors profile between these two time periods. In addition, this will be the first study to validate the predictors of readmission in decompensated cirrhosis in any Asian population.
Material and MethodsStudy designThis was a single center prospective study conducted at a large tertiary level public hospital in the Western India between August 2014 and August 2016. Study protocol was approved by the institutional ethics committee of Lok-manya Tilak Municipal Medical College and complies with the ethical guidelines of 1975 declaration of Helsinki. Informed written consent was obtained from all the study participants.
Inclusion criteria and exclusion criteriaStudy cohort included all the patients with age > 18 years with cirrhosis of liver hospitalized due to any of the hepatic decompensations. Patients who refused to give consent, discharged against medical advice, underwent liver transplantation or died during index hospitalisation or with inconclusive diagnosis of cirrhosis were excluded from the study. Similarly, patients admitted for elective reasons (i.e. cirrhosis patient with hepatocellular carcinoma admitted for TACE, cirrhosis patients admitted for conditions unrelated to liver cirrhosis) were not included in the study population.
PatientsCirrhosis was diagnosed by combination of clinical symptoms, laboratory evaluation (e.g. low platelet count, detailed liver profile), radiological parameters (coarse nodular liver, splenomegaly and features of portal hypertension) and endoscopic detection of oesophageal or gastric varices or portal hypertensive gastropathy (PHG). Liver biopsy was performed only in cases of doubtful chronic liver disease where diagnosis was uncertain.
Hepatic decompensation during the index hospitalisation included the following: Volume overload (ascites, lower limb edema, anasarca), renal failure, hepatic encephalopathy (HE), portal hypertensive bleeding and spontaneous bacterial peritonitis (SBP). They were defined as under.
- •
Volume overload. Ascites or anasarca or pedal edema requiring hospitalisation or paracentesis in patients with cirrhosis.
- •
Hepatic encephalopathy. Altered mental status or neuropsychiatric abnormalities in the presence of liver cirrhosis, after exclusion of other causes.
- •
Spontaneous bacterial peritonitis. More than 250 polymorphonuclear leukocytes per high power field and/or positive culture in the ascitic fluid.
- •
Portal hypertensive bleeding. Patients with gastrointestinal (GI) bleed with varices seen on endoscopy or significant bleed in a diagnosed case of cirrhosis.
- •
Renal failure. Serum creatinine > 1.5 mg/dL or rise in serum creatinine > 0.3 mg/dL from the baseline in patients with ascites.
In presence of more than one complications in one patient, principal cause of hospitalisation was defined as per the following: Patients with renal failure in presence of ascites were considered in renal failure group. Likewise, admissions with HE in presence of precipitating factors like GI bleed, SBP or renal failure were attributed to the respective precipitating factor. SBP in presence of GI bleed or renal failure were taken as SBP.
Study protocolPatients were enrolled in the study when they were hospitalized with decompensated cirrhosis. During index hospitalisation, data were collected and compiled regarding demographic profile, history, clinical features, presence of other comorbidities, aetiology of cirrhosis, type of decompensation and number of complications, blood laboratory parameters on discharge (complete haemogram, bilirubin, transaminases, albumin, prothrombin time with international normalised ratio (INR), renal function tests and electrolytes), Child Turcotte Pugh (CTP) score at discharge, Model for End-Stage Liver Disease (MELD) score at discharge and length of stay during hospitalisation. Patients were followed for 3 month to look for any event of readmission using liver clinic records, institutional medical records or telephonic conversations. Readmissions details that occurred in other hospitals were compiled either from the discharge cards or via telephonic talks. Similarly, patients electively readmitted for planned procedures, surgery or therapy for hepatocellular carcinoma or admitted for reasons unrelated to liver disease were not considered in the evaluation. Patients with incomplete follow up were not included in the final analysis. The study protocol has been outlined in Figure 1.
Statistical analysisIncidence of readmission at 1-month and 3-months were calculated as percentage of total eligible readmissions. Patients who were readmitted within 1-month of index hospitalisation were compared with those without readmission for demographic, laboratory and disease variables during index hospitalisation. Univariate analysis was done using Student’s t-test for parametric continuous variables and Mann-Whitney U test for nonparametric data. Categorical variables were evaluated using %2 test. Variables with P value < 0.05 were further analysed by multivariate logistic regression analysis by forward stepwise selection model. P value < 0.05 was considered as statistically significant. Similar protocol was used to determine the predictors of readmission at 3-months. Receiver operating characteristics (ROC) curves were obtained to get the cut-off values of variables that best predict hospital readmissions. Differences between predictors at 1 and 3-months readmissions were also noted. All statistical analyses were done using SPSS software version 16 (SPSS Inc., Chicago, USA).
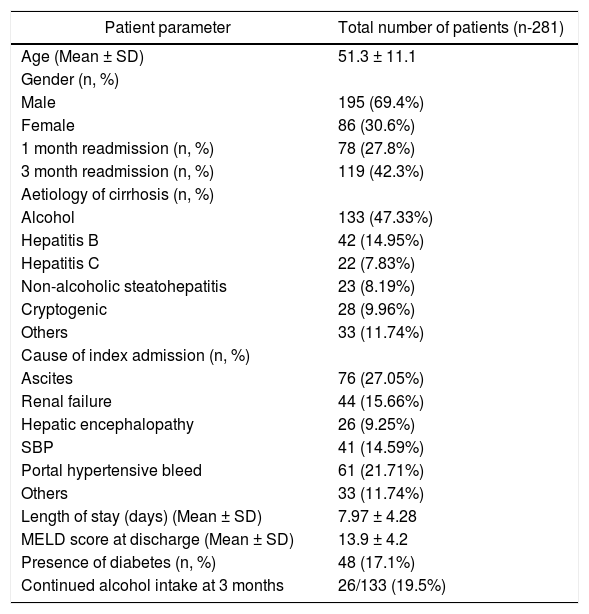
ResultsIndex hospitalisationTotal 281 patients hospitalized with decompensated chronic liver disease and completed desired follow-up were included in the study analysis. Mean age of the study population was 51.3 ± 11.1 years. Majority of the patients were male (195/281, 69.4%). Demographic, biochemical and aetiological characteristics of the study population are outlined in Table 1. Predominant aetiology of chronic liver disease was alcohol found in 47.33% patients (133/281), followed by hepatitis B (14.95%), cryptogenic cirrhosis (9.96%) and non-alcoholic steatohepatitis (NASH) (8.19%). While, the most common decompensation event responsible for index hospitalisation was volume over-load/ascites (27.05%) followed by upper GI bleed, renal failure, spontaneous bacterial peritonitis and hepatic en-cephalopathy. Average length of stay was 7.97 ± 4.28 days and average MELD score at discharge was 13.9 ± 4.2.
Demographic profile and aetiological characteristics of the study cohort during index hospitalisation.
| Patient parameter | Total number of patients (n-281) |
|---|---|
| Age (Mean ± SD) | 51.3 ± 11.1 |
| Gender (n, %) | |
| Male | 195 (69.4%) |
| Female | 86 (30.6%) |
| 1 month readmission (n, %) | 78 (27.8%) |
| 3 month readmission (n, %) | 119 (42.3%) |
| Aetiology of cirrhosis (n, %) | |
| Alcohol | 133 (47.33%) |
| Hepatitis B | 42 (14.95%) |
| Hepatitis C | 22 (7.83%) |
| Non-alcoholic steatohepatitis | 23 (8.19%) |
| Cryptogenic | 28 (9.96%) |
| Others | 33 (11.74%) |
| Cause of index admission (n, %) | |
| Ascites | 76 (27.05%) |
| Renal failure | 44 (15.66%) |
| Hepatic encephalopathy | 26 (9.25%) |
| SBP | 41 (14.59%) |
| Portal hypertensive bleed | 61 (21.71%) |
| Others | 33 (11.74%) |
| Length of stay (days) (Mean ± SD) | 7.97 ± 4.28 |
| MELD score at discharge (Mean ± SD) | 13.9 ± 4.2 |
| Presence of diabetes (n, %) | 48 (17.1%) |
| Continued alcohol intake at 3 months | 26/133 (19.5%) |
Seventy eight patients (27.8%) were readmitted within 1-month of index hospitalisation. Median time to readmission was 18 days. Volume overload related complications (ascites in 26.9% and renal failure in 21.8%) were the most common causes of readmission, while incidence was highest in patients with HE during index stay (46.2%) and alcoholic cirrhosis (35.3%).
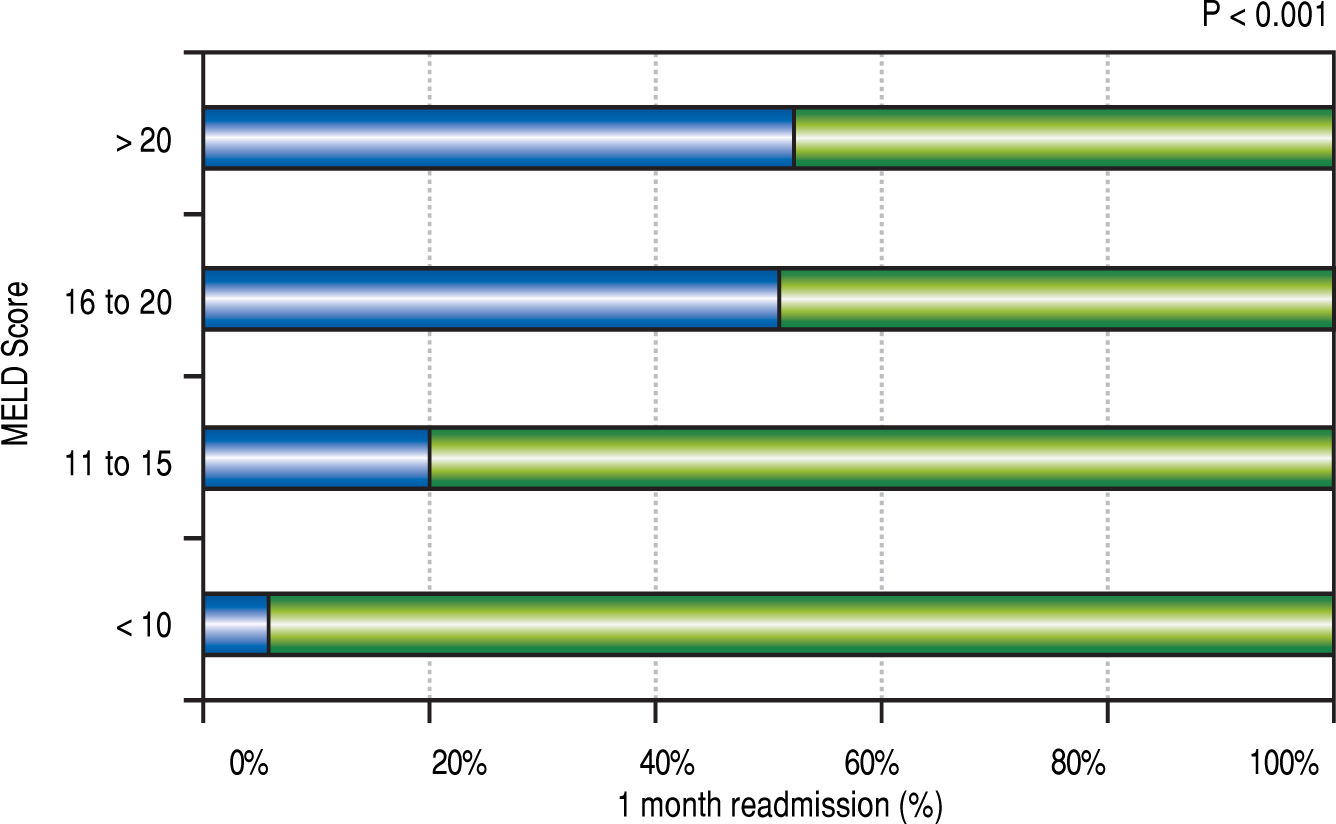
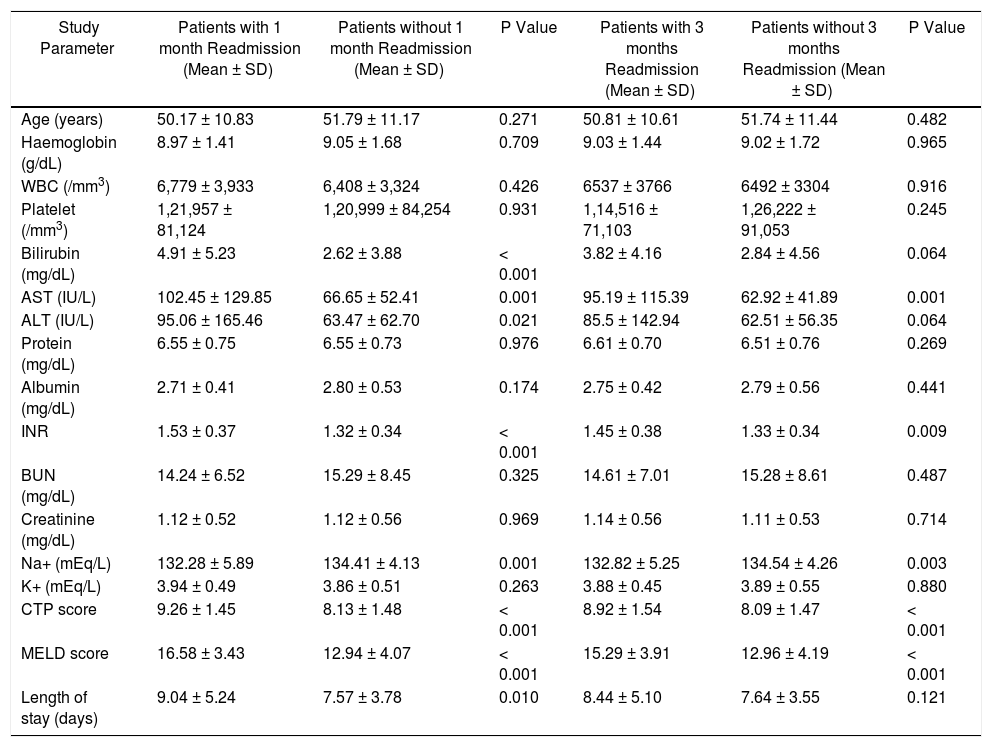
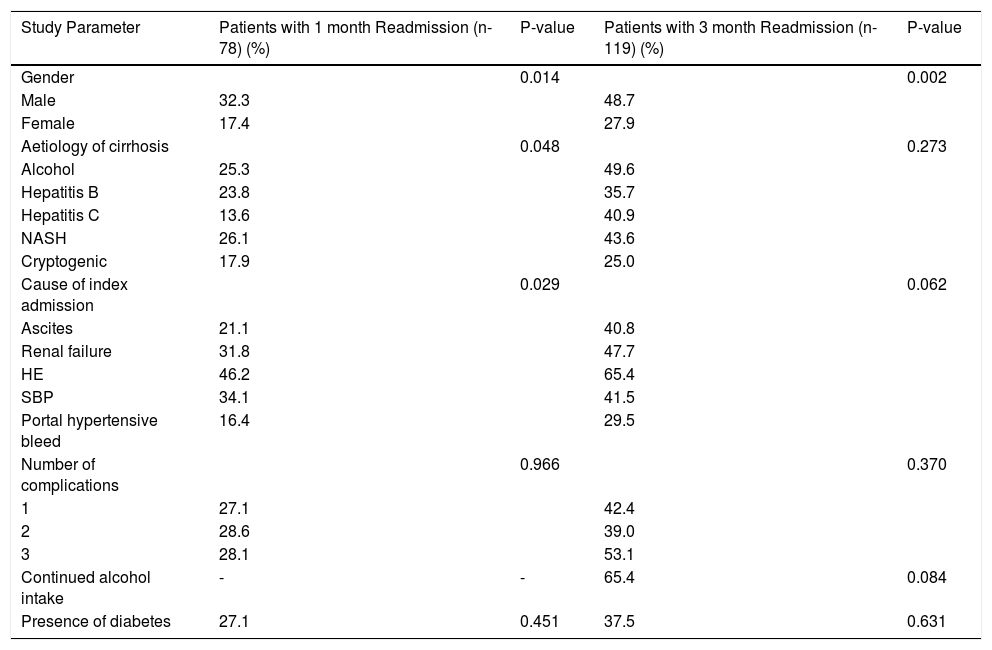
Univariate analysisSeveral continuous and categorical parameters during index hospitalisation were compared between patients who were readmitted within 1-month and those who were not (Tables 2Table 3). Readmission rate was higher in males than in females (32.3% vs. 17.4%, p-0.014). Among laboratory parameters, serum bilirubin (p < 0.001), alanine aminotransferase (p-0.001), aspartate aminotransferase (p-0.021), INR (p < 0.001) and serum sodium (p-0.001) were significantly associated with 1-month readmission. Severity of liver disease as calculated by Model for End stage Liver Disease (MELD) score (16.6 vs. 12.9, p < 0.001) and Child Pugh (CTP) score (9.26 vs. 8.1, P < 0.001) were also correlated significantly with early readmissions at 1-month. Figure 2 illustrates a bar diagram showing 1-month readmission rates in different MELD groups. Patients with readmissions had longer index hospital stay (9.04 ± 5.27 vs 7.57 ± 3.78, p-0.01). Among categorical variables, aetiology of liver disease (p-0.048) and cause of decompensation during index hospitalisation (p-0.029) were significantly associated with 1-month readmission, whereas number of complications during index admission was statistically similar in both the groups (p-0.966).
Univariate analysis of continuous variables between patients who readmitted at 1 month or 3 months and those who did not require readmission within same time durations.
| Study Parameter | Patients with 1 month Readmission (Mean ± SD) | Patients without 1 month Readmission (Mean ± SD) | P Value | Patients with 3 months Readmission (Mean ± SD) | Patients without 3 months Readmission (Mean ± SD) | P Value |
|---|---|---|---|---|---|---|
| Age (years) | 50.17 ± 10.83 | 51.79 ± 11.17 | 0.271 | 50.81 ± 10.61 | 51.74 ± 11.44 | 0.482 |
| Haemoglobin (g/dL) | 8.97 ± 1.41 | 9.05 ± 1.68 | 0.709 | 9.03 ± 1.44 | 9.02 ± 1.72 | 0.965 |
| WBC (/mm3) | 6,779 ± 3,933 | 6,408 ± 3,324 | 0.426 | 6537 ± 3766 | 6492 ± 3304 | 0.916 |
| Platelet (/mm3) | 1,21,957 ± 81,124 | 1,20,999 ± 84,254 | 0.931 | 1,14,516 ± 71,103 | 1,26,222 ± 91,053 | 0.245 |
| Bilirubin (mg/dL) | 4.91 ± 5.23 | 2.62 ± 3.88 | < 0.001 | 3.82 ± 4.16 | 2.84 ± 4.56 | 0.064 |
| AST (IU/L) | 102.45 ± 129.85 | 66.65 ± 52.41 | 0.001 | 95.19 ± 115.39 | 62.92 ± 41.89 | 0.001 |
| ALT (IU/L) | 95.06 ± 165.46 | 63.47 ± 62.70 | 0.021 | 85.5 ± 142.94 | 62.51 ± 56.35 | 0.064 |
| Protein (mg/dL) | 6.55 ± 0.75 | 6.55 ± 0.73 | 0.976 | 6.61 ± 0.70 | 6.51 ± 0.76 | 0.269 |
| Albumin (mg/dL) | 2.71 ± 0.41 | 2.80 ± 0.53 | 0.174 | 2.75 ± 0.42 | 2.79 ± 0.56 | 0.441 |
| INR | 1.53 ± 0.37 | 1.32 ± 0.34 | < 0.001 | 1.45 ± 0.38 | 1.33 ± 0.34 | 0.009 |
| BUN (mg/dL) | 14.24 ± 6.52 | 15.29 ± 8.45 | 0.325 | 14.61 ± 7.01 | 15.28 ± 8.61 | 0.487 |
| Creatinine (mg/dL) | 1.12 ± 0.52 | 1.12 ± 0.56 | 0.969 | 1.14 ± 0.56 | 1.11 ± 0.53 | 0.714 |
| Na+ (mEq/L) | 132.28 ± 5.89 | 134.41 ± 4.13 | 0.001 | 132.82 ± 5.25 | 134.54 ± 4.26 | 0.003 |
| K+ (mEq/L) | 3.94 ± 0.49 | 3.86 ± 0.51 | 0.263 | 3.88 ± 0.45 | 3.89 ± 0.55 | 0.880 |
| CTP score | 9.26 ± 1.45 | 8.13 ± 1.48 | < 0.001 | 8.92 ± 1.54 | 8.09 ± 1.47 | < 0.001 |
| MELD score | 16.58 ± 3.43 | 12.94 ± 4.07 | < 0.001 | 15.29 ± 3.91 | 12.96 ± 4.19 | < 0.001 |
| Length of stay (days) | 9.04 ± 5.24 | 7.57 ± 3.78 | 0.010 | 8.44 ± 5.10 | 7.64 ± 3.55 | 0.121 |
Univariate analysis of categorical variables between patients who readmitted at 1 month or 3 months and those who did not require readmissions.
| Study Parameter | Patients with 1 month Readmission (n-78) (%) | P-value | Patients with 3 month Readmission (n-119) (%) | P-value |
|---|---|---|---|---|
| Gender | 0.014 | 0.002 | ||
| Male | 32.3 | 48.7 | ||
| Female | 17.4 | 27.9 | ||
| Aetiology of cirrhosis | 0.048 | 0.273 | ||
| Alcohol | 25.3 | 49.6 | ||
| Hepatitis B | 23.8 | 35.7 | ||
| Hepatitis C | 13.6 | 40.9 | ||
| NASH | 26.1 | 43.6 | ||
| Cryptogenic | 17.9 | 25.0 | ||
| Cause of index admission | 0.029 | 0.062 | ||
| Ascites | 21.1 | 40.8 | ||
| Renal failure | 31.8 | 47.7 | ||
| HE | 46.2 | 65.4 | ||
| SBP | 34.1 | 41.5 | ||
| Portal hypertensive bleed | 16.4 | 29.5 | ||
| Number of complications | 0.966 | 0.370 | ||
| 1 | 27.1 | 42.4 | ||
| 2 | 28.6 | 39.0 | ||
| 3 | 28.1 | 53.1 | ||
| Continued alcohol intake | - | - | 65.4 | 0.084 |
| Presence of diabetes | 27.1 | 0.451 | 37.5 | 0.631 |
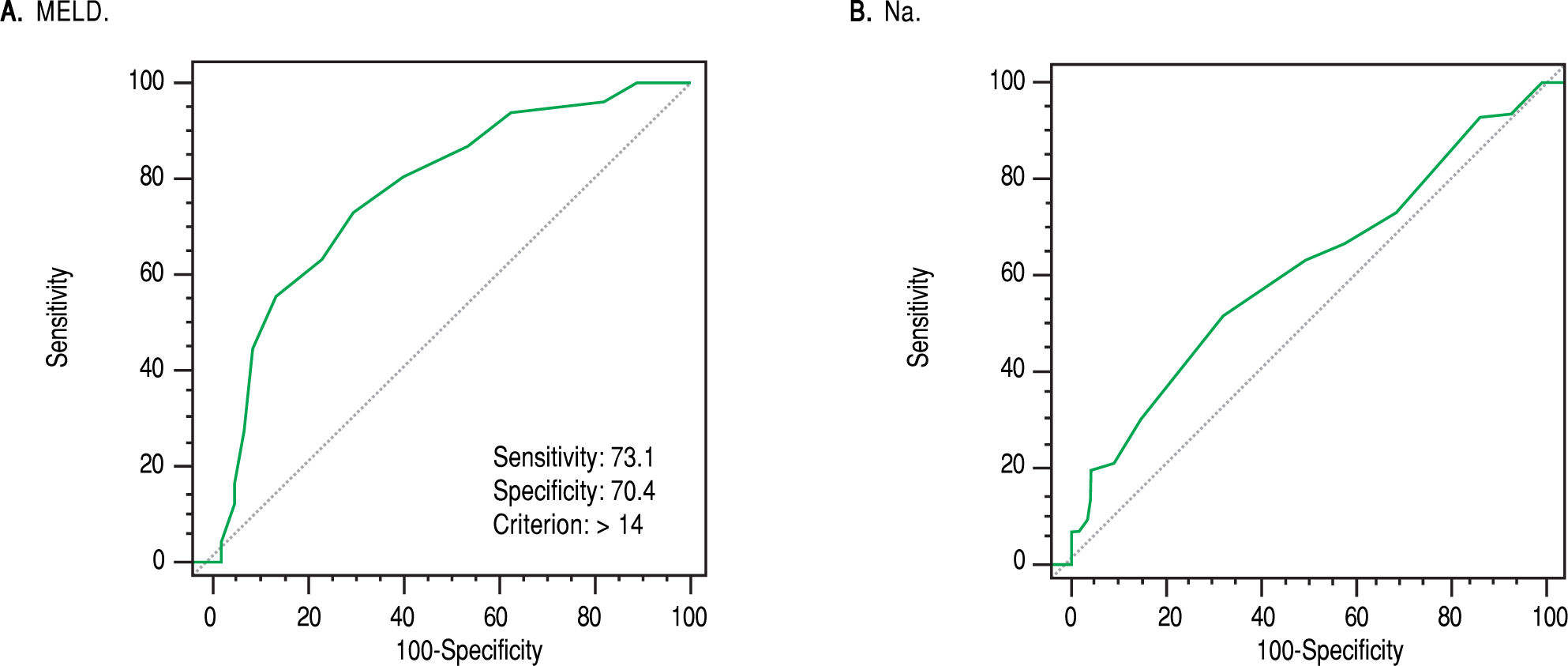
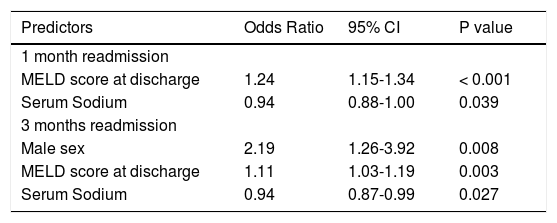
Variables with p value < 0.05 on univariate analysis were considered for building a forward stepwise model for multivariate binary logistic regression analysis. Out of eleven risk factors, only MELD score at discharge [Odds Ratio (OR): 1.24; 95% confidence interval (CI):1.15 - 1.34; p-< 0.001] and serum sodium during index stay [OR: 0.94; CI: 0.88 - 1.00: p: 0.039] turned out to be the independent predictors of hospital readmissions at 1-month. Interestingly, neither the aetiology of cirrhosis nor the type of decompensation during index hospitalisation were the risk factors for early readmissions. Figure 3A shows ROC curve for MELD score for prediction of 1-month readmission with area under the curve (AUC) of 0.778. MELD score more than 14 best predicted 1-month readmissions. Similarly, AUC for serum sodium was 0.599 with sodium level less than 133 as the best cut-off (Figure 3B).
A. Receiver operating characteristic curve of Model for End Stage Liver Disease (MELD) score that predicts 1-month readmission in decompensated cirrhosis (area under the curve-0.778). A MELD score more than 14 best predicts readmission at 1 month with sensitivity of 73.1% and specificity of 70.4%. B. Receiver operating characteristic curve of serum sodium that predicts 1-month readmission in decompensated cirrhosis (area under the curve - 0.599). Serum sodium level less than 133 meq/L best predicts readmission at 1-month with sensitivity of 52,6% and specificity of 65.8%.
Incidence of 3-months readmissions was 42.3% in our study with total 119 patients readmitted 1 or more times. Males had higher readmissions than females (48.7 vs. 27.9%, p-0.002), so as patients with alcoholic liver disease (49.6%). Continued alcohol intake post discharge was observed in 19.5% patients; out of them, readmissions were seen in 65.4% patients. Patients with HE had highest readmissions at 3-months (65.4%).
Univariate analysisWhen index hospitalisation variables were compared, patients with 3-months hospital readmission had more severe cirrhosis (MELD score [p < 0.001], CTP score [p < 0.001] and INR [p-0.009]) and low serum sodium (p0.003) (Table 2). Whereas, no significant difference was noted in proportion of patients rehospitalised depending on the aetiology of cirrhosis (p-0.273). Similarly, number of complications during index hospitalisation (p-0.370) and continued alcohol intake during follow up (p-0.084) did not differ significantly between two groups. (Table 3).
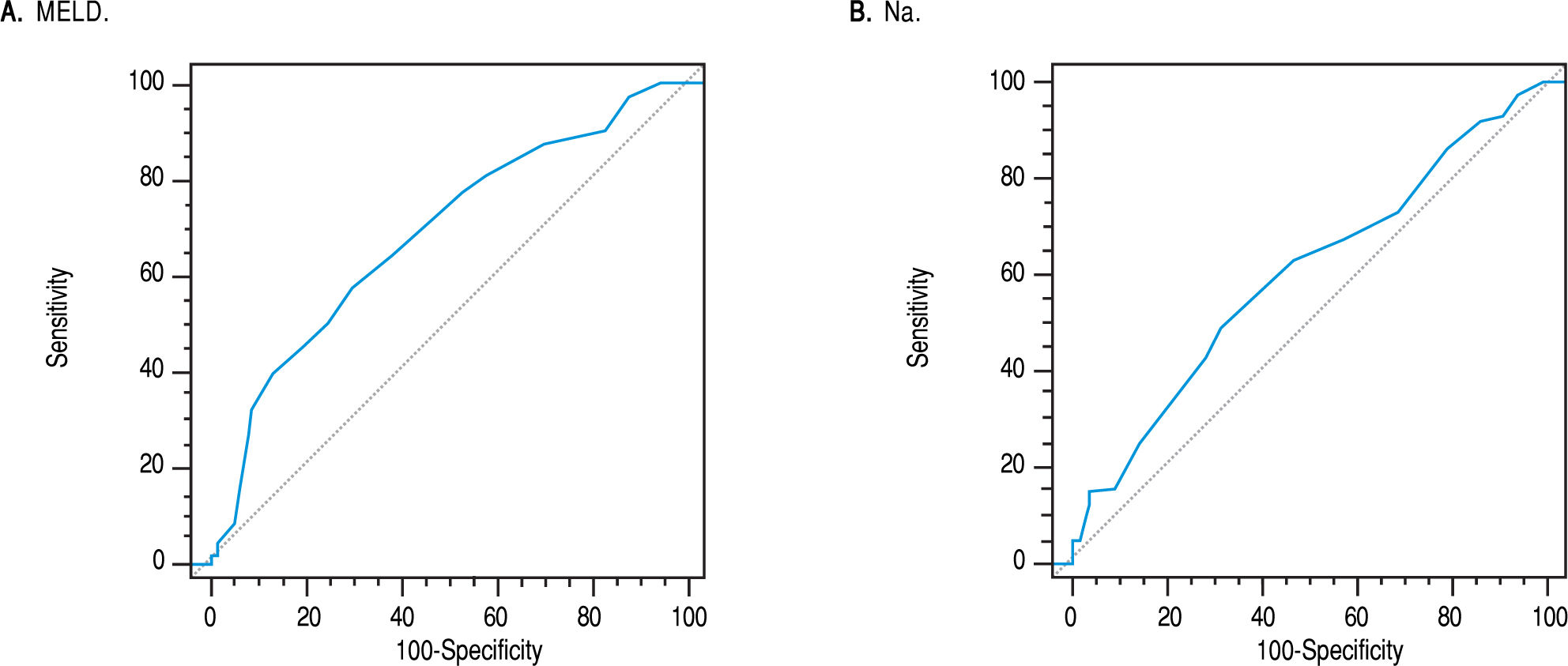
Multivariate analysisSimilar to 1-month readmission, MELD score at discharge [OR: 1.11; CI: 1.03-1.19; p: 0.003] and low serum sodium [OR: 0.94; CI: 0.87 - 0.99; p: 0.027] were also independent predictors of 3-month readmissions on binary logistic regression analysis. In addition, Male gender emerged as independent risk factor for 3-months readmissions [OR: 2.19; CI: 1.26 - 3.92; p: 0.008]. ROC curve of MELD score predicting 3-months readmission has been drafted in Figure 4A, which is showing AUC of 0.678. Most accurate cut-offs for the MELD score and serum sodium levels were 14 and 133 mEq/L respectively, beyond which the risk of readmission was highest (Figure 4B).
A. Receiver operating characteristic curve of Model for End Stage Liver Disease (MELD) score that predicts 3-months readmission in decompensated cirrhosis (area under the curve-0.678). A MELD score more than 14 best predicts readmission at 3 months with 57.1% sensitivity and 69.8% specificity. B. Receiver operating characteristic curve of serum sodium that predicts 3-months readmission in decompensated cirrhosis (area under the curve - 0.592). Serum sodium level less than 133 mEq/L best predicts readmission at 3-months with sensitivity of 49,2% and specificity of 67.9%.
Multivariate analysis of independent predictors associated with early hospital readmissions.
| Predictors | Odds Ratio | 95% CI | P value |
|---|---|---|---|
| 1 month readmission | |||
| MELD score at discharge | 1.24 | 1.15-1.34 | < 0.001 |
| Serum Sodium | 0.94 | 0.88-1.00 | 0.039 |
| 3 months readmission | |||
| Male sex | 2.19 | 1.26-3.92 | 0.008 |
| MELD score at discharge | 1.11 | 1.03-1.19 | 0.003 |
| Serum Sodium | 0.94 | 0.87-0.99 | 0.027 |
Patients with decompensated cirrhosis are most vulnerable to hospital readmissions early after discharge because of several reasons e.g. immediate effects and recurrent nature of complications prevalent during index admission, need for frequent titration of medications like diuretics and lactulose, need for laboratory tests and frequent follow up visits, side effects of medications and transfer of patients from indoor tertiary care to community level physicians. In addition to that, noncompliance to medications and diet, alcohol addiction and intake of complementary and alternative medications further predispose this already vulnerable population to increased risk of rehospitalisation.
The present study showed incidence of readmission of 27.8% at 1-month and 42.3% at 3-months in an Asian Indian cohort of decompensated chronic liver disease. These rates were lower than those found in the North American cohorts, which showed readmission rates of upto 37% at 1-month9 and 53% at 3 months.10 Only MELD score at discharge and serum sodium during hospital stay independently predicted both 1-month and 3-months readmissions, whereas male gender predicted only 3-months readmissions. MELD score was a better predictor than serum sodium for both the time periods (difference of AUC-0.179, p-0.0001 for 1-month readmission; difference of AUC-0.086, p-0.038 for 3-months readmission). Despite of being a single center study, the results were comparable to other larger multicentre studies.10
Severity of liver disease during index hospitalisation, as represented by MELD score at discharge, was independently associated with readmissions in our study. Initially developed to predict 3-months survival of patients undergoing transjugular intrahepatic portosystemic shunt (TIPS),13 MELD score has been validated for multiple outcomes in cirrhosis ranging from organ allocation in liver transplantation14 and acute liver failure15 to prediction of perioperative mortality in other surgical procedures,14 prognosis and treatment of acute on chronic liver failure (ACLF)16 and alcoholic hepatitis.17 This finding was analogous to the reports from the NACSELD group and other single center studies.8-12 Our study corroborates the previous studies8-12 and validates the MELD score to predict hospital readmissions upto 3-months in the Asian population. The odds of 1-month readmission increased by 24% and 3-months readmission increased by 11% for each one point increase in the MELD score at discharge in our study. Patients with MELD score more than 14 had the largest area under the ROC curve (AUC-0.778) with sensitivity of 73.4% and specificity of 70.4% in predicting 1-month readmissions; higher than predicting 3-months readmission (AUC-0.678). In our study, serum sodium independently predicted early hospital readmissions. With each 1 mEq/L decrease in serum sodium concentration, odds of readmission increased by 6% both at 1-month and 3-months. Serum sodium less than 133 mEq/L best predicted early readmissions with 52.6% sensitivity and 65.8% specificity (1-month readmission AUC-0.599, 3-months readmission AUC-0.592). Hyponatremia is common in advanced chronic liver disease and predicts mortality independent of the MELD score.18 Additionally, studies have also shown that combining hyponatremia with MELD score predicts mortality better than MELD score alone19,20 and thereby serum sodium has been recently included in the organ allocation criteria for liver transplantation.21 Our study described another predictive role of serum sodium in estimating 1-month and 3-months readmissions in decompensated cirrhosis.
Males were highly predisposed to readmissions with odds of readmission 119% higher than the females. Males constitute nearly 70% of our study population and 90% of the alcoholic cirrhosis cohort, which had the highest readmission rates among all the aetiologies (upto 49.6%). In India, alcohol still predominates as a cause of cirrhosis and males form the majority among patients with alcohol abuse.22 Anecdotally, we see high prevalence of certain psychosocial factors like noncompliance, substance addictions and avoidance of healthcare in males and that might explain the drastic difference of readmission between the genders; however these should be confirmed by evidence based studies.
Contradictory to many North American studies,8,10,12 presence of diabetes did not turn up as a risk factor for early or late hospital readmissions in advanced cirrhosis in this study. Few reasons could elucidate this finding. First, lesser prevalence of NASH in India as compared to the West might be the primary justification. In India, the prevalence of NASH has been estimated between 9-32% in epidemiological studies.23,24 NASH as a cause of cirrhosis was seen in only 8.2% of patients in our study. Alcohol and chronic viral hepatitis B and C are still the leading causes of cirrhosis in India than the west, where much sizeable proportion is formed by NASH related cirrhosis.25 Second, our center is a tertiary care public hospital where majority of the treated patients belong to lower or middle income groups. NASH is seen less commonly in these class of patients with higher proportions of country liquor abuse.
Clinical experience suggests that complications like renal failure or HE are more recurrent than others and elevate readmissions within days of discharge. We initially hypothesized that they could be the possible risk factors for 1-month readmissions. Despite of higher proportion of readmissions in patients with HE than others (46.2% vs. 27.8%; p-0.029), only MELD score and serum sodium turned to be the better predictors on logistic regression. Similarly, aetiology of cirrhosis did not predict readmissions, even though very high readmission rates were seen in certain aetiologies like alcoholic liver disease. In spite of being an index of cirrhosis severity, CTP score did not appear as a risk factor. Individually bilirubin and INR were associated with readmissions but other insignificant factors like albumin, ascites and mental status made all-inclusive CTP score insignificant.
Few recognised limitations of our study must be discussed. Being a single center study, it does not represent the entire region. However patients are referred to our hospital from a larger region of a country extending from the Northern states to the East and South India. Socioeconomic risk factors like patient education, social status, economic class and other influencing variables like use of complementary and alternative medications, presence and degree of noncompliance by the patient were not taken into consideration in the present study. They will need to be addressed in similar studies. Not exactly a limitation, but liver transplantation should be mentioned in brief. We have a common public hospital transplant program in our city. In spite of that none of our patients underwent liver transplantation during index hospitalisation or during follow-up. Extremely high costs, poor availability of organs and nonparticipation of public hospitals have made liver transplantation out of reach to even middle income groups in India; only < 2% transplantations occur in public hospitals.25 However its overall impact on incidence and prediction of readmissions remains negligible.
In conclusion, this study showed high early and late readmission rates in the Asian Indian cohort of decompensated chronic liver disease. MELD score, serum sodium and male gender turned up as independent risk factors for readmission. Our study will provide useful insight to design such targeted interventions in patients with advanced liver disease and help mitigate readmissions. Finally, our study was notable in such a way that it was the first to validate the above described risk factors as predictors of hospital readmission in advanced cirrhosis in an Asian population.
Abbreviations- •
ACLF: cute on chronic liver failure.
- •
AUC: area under the curve.
- •
CI: confidence interval.
- •
CTP: child turcotte pugh.
- •
GI: gastrointestinal.
- •
HE: hepatic encephalopathy.
- •
INR: International Normalised Ratio.
- •
MELD: Model for End stage Liver Disease.
- •
cNACSELD: The North American Consortium for End Stage Liver Disease.
- •
NASH: non-alcoholic steatohepatitis.
- •
OR: Odd’ ratio.
- •
PHG: portal hypertensive gastropathy.
- •
ROC urve: receiver operating characteristics curve.
- •
SBP: spontaneous bacterial peritonitis.
- •
TIPS: transjugular intrahepatic portosystemic shunt.
No financial assistance was taken for the execution of the study.
Conflicts of InterestThe authors declares that there is no conflict of interest regarding the publication of this article.