Non-steroidal-anti-inflammatory drugs (NSAIDs) make a heterogenous pharmaco-therapeutic class of drugs among the most used drugs worldwide with various indications, modes of administration and increasing automedication. NSAIDs can cause acute liver injury with variable severity. The recent identification of genetic markers might facilitate the diagnosis and the prediction of hepatotoxicity risk.
Non-steroidal-anti-inflammatory drugs (NSAIDs) are among the most used drugs worldwide. Their indications are multiple, mainly to treat various inflammatory diseases or to relief acute pain or fever in various acute or chronic situations.1,2 Consequently, their use is very variable regarding the administration route (orally, parenterally, percutaneously, suppository), the duration of administration (from single dose to long term treatment), the variable dosage according to the type of indication (low to high dose), as monotherapy or in combination with other drugs (for instance, paracetamol). This variability leads frequently to automedication beside the prescription by a care professional. NSAIDs make a heterogenous pharma-co-therapeutic class of drugs, with variable side-effects, gastro-duodenal, intestinal, cutaneous, renal et hepatic. They are responsible for about 10% of cases of drug-induced liver injury.1–3 Ninety-nine % of reported cases of hepatotoxicity are caused by seven NSAIDs.3 The estimated incidence of NSAID-induced hepatotoxicity is variable, ranging from 0.29 to 9 per 100,000 patients per year.1,6 However, considering the quantity of consummed NSAIDs, hepatotoxicity is a rare event.5
The specific clinical aspects of liver injuries and the involved mechanisms of each class of NSAIDS are presented below as well as the recent advances for the diagnosis and prediction of hepatotoxicity.
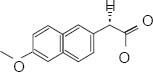
HEPATOTOTOXICITY OF THE DIFERENT CLASS OF NSAIDS1–11NSAIDs are classified into families according to their molecular structure: acetic acid derivatives, propionic acid derivatives, salicylates, enolic acid derivatives (Oxicams) and selective COX-2 inhibitors (Table 1).
| NSAID | NSAID Class | Molecular structure | Clinical Phenotype | Proposed mechanism | Frequency* LiverTox** (8) RUCAM Evaluation*** | Increase transaminases Symptomatic hepatitis (Transaminases > 3N) |
|---|---|---|---|---|---|---|
| Diclofenac | Acetic acid derivatives | Acute hepatitis Hepatocellular | Metabolic-Idiosyncratic Increased toxic metabolic formation Mitochondrial dysfunction | 34.1% > 50 cases | 15% 2-4% | |
| Ibuprofen | Propionic acid derivatives | Acute hepatitis Hepatocellular Cholestatic Vanishing bile duct syndrome | Metabolic-Idiosyncratic Mitochondrial dysfunction | 14.6% | Same as placebo at low dosages but > 16% for higher dosages | |
| Sulindac | Acetic acid derivatives | Acute hepatitis Cholestatic or mixed | Immunoallergic-Idiosyncratic | 12.4% > 50 cases | Severe rare hepatitis 0.1% of users (5/100,000) | |
| Acetylsalicylic acid | Salicylates | Acute hepatitis Hepatocellular Reye syndrome | Intrinsic toxicitydose dependent Mitochondrial dysfunction | 12% | ||
| Naproxen | Propionic acid derivatives | Acute hepatitis Hepatocellular Cholestatic | Metabolic and Immunoallergic Idiosyncratic | 11.1% | 4% of users 9-12 cases/ 100,000 | |
| Piroxicam | Enolic acid derivatives | Acute hepatitis Cholestatic hepatocellular | Immunoallergic-diosyncratic Increased toxic metabolic formation | 9.3% | 3-18% of users 1-5/100,000 | |
| Nimesulide | Sulfonanilides | Acute hepatitis hepatocellular Cholestatic | Metabolic-diosyncratic Mitochondrial dysfunction | 5.8% > 50 cases | 15% <1% |
The review regards cases reported with variable dates of publications and methods of causality assessment. The accuracy of causality assessment is obviously a key -point.12 The Roussel-Uclaf Causality Assessment Method Method (RUCAM) developed more than 20 years ago to assess rigorously causlity in suspected drug-induced liver injury has been recently refinied to help clinicians and health authorities.13 The RUCAM has been choosed as the reference method in recent international guidelines for DILI evaluation.14 Indeed, RUCAM is based on the importance of various types of suspected DILI.13 The limitations of RUCAM is that it has not been designed for suspected chronic DILI, which is mostly an unrecognized preexisting liver disease.13 Consequently, aiming to provide a fair presentation, we indicate the drugs, cases or series presented in this review which have been assessed with the RUCAM assessement.4,5,9,10
Propionic acid derivativesIn this class, the two most hepatotoxic compounds are ibuprofen and naproxen.1,3–8 Ketoprofen causes lower hepatotoxicity with an increase in transaminases over three times the upper limit of normal in less than 1% of patients and a single case of fulminant hepatitis indexed in LiverTox.8 They mostly cause acute hepatocellular or cholestatic hepatitis.1,3–8 Much less commonly, there are also cases of cholestasis with prolonged course and vanishing bile duct syndrome for ibuprofen.4,8,9 The mechanism of toxicity is primarily metabolic-idiosyncratic.1,3–9 NSAIDs of this class are also responsible for microvesicular steatosis due to an inhibitory effect of the carboxylic radical on mitochondria.9 In contrast with cyclins or cordarone, microvesicular steatosis remains benign and are is not accompanied by acute hepatic insufficiency.1,3–9 Crosshepatotoxicity may occur within NSAIDs of this class as reported between naproxen and fenoprofen.9
Acetic acid derivativesIn this class, there are two of the most hepatotoxic NSAIDs: diclofenac and sulindac. They cause acute hepatocellular or cholestatic hepatitis. The mechanism of toxicity is primarily idiosyncratic.1,3–9 Genetic factors have been demonstrated for diclofenac.10 It is mainly metabolized by CYP2C9, of which there are several polymorphisms but which do not seem to be associated with hepatotoxicity.10 In contrast, allelic variants for the genes encoding the enzymes involved in the metabolism of diclofenac UGT2B7, CYP2C8, and ABCC2 have been associated with increased risk of hepatotoxicity, particularly for patients with at least one UGT2B7 allele ⋆ 2 (OR 8.5).10 Similarly, allelic variants for cytokine receptors involved in the immune and inflammatory reaction (Interleukins 4 and 10) are associated with the hepatic toxicity of diclofenac.10 Some cases of cross-hepatotoxicity between indomethacin and sulindac have been reported.1,8,9
Salicylates1,3–8The only NSAID in this class is acetylsalicylic acid, one of the most widely used analgesic and antipyretic treatments in the world. It acts as an irreversible inhibitor of COX 1. Its mechanism of toxicity is dose-depending. While most cases are asymptomatic, cases of severe hepatitis for doses between 1800 and 3200 mg per day (blood level of 25 mg/dL).8,9 Reye’s syndrome is a particular form of toxicity of acetylsalicylic acid: in children, taking aspirin during a viral infection (chicken pox, influenza) can lead to severe hepatitis with severe microvesicular steatosis.9
Enolic acid derivatives (Oxicams)1,6–9Among the NSAIDs in the class, the most hepatotoxic is piroxicam. It is more frequently acute cholestatic than hepatocellular hepatitis. The mechanism of toxicity is unknown. An idiosyncratic immunoallergic toxicity and toxic metabolites are mentioned first.
Selective COX-2 inhibitors1,6–9Rare cases of idiosyncratic acute hepatitis secondary to celecoxib have been described. The mechanism is idiosyncratic and immunoallergic, especially in patients with a history of sulfonamide allergy. Lumiracoxib, another NSAID in this class, was withdrawn from the market in 2007 after more than 20 cases of severe acute hepatitis occurred in Europe and Australia.11 However, a genetic study revealed a strong association between HLA variant DRB1 ⋆ 1501-DQB1 ⋆ 0602-DRB5 ⋆ 0101-DQA1 ⋆ 0102 and hepatotoxicity (OR 7.5).11 Lumiracoxib is one of the best examples of the link between genetics and hepatotoxicity.
Sulfonanilides1,6–9The only NSAID in the class is nimesulide, a preferred inhibitor of COX 2.
This is mainly acute hepatocellular hepatitis. The mechanism of toxicity is metabolic-idiosyncratic.
SYNTHESIS OF NSAID HEPTATOTOXICITYIn total, NSAID- hepatotoxicity varies from one molecule to another with a variable level of evidence. The majority (99%) of reported cases of hepatotoxicity are attributed to seven NSAIDs (Table 1).3 For diclofenac, ibuprofen and nimesulide, the causality assessment has been made using the RUCAM;4,5,9,10 for sulindac, naproxen, piroxicam, the causality has been assessed individually without unspecific method of assessment which may lower the level of evidence. For acetylsalicylic acid, hepatotoxicity is described for long with many cases. The role of this drug in the onset of Reye syndrome is well-documented with a comprehensive mechanism. The clinical phenotype is mostly acute liver injury with variable severity from mild and transient increase of transaminases to fulminant hepatitis.1,3–9 Uncommonly, microvesicular steatosis may occur with proprionic acid derivatives with a fair level of evidence since the lesion is reproducible in animals.9 Most acute liver injuries associated with NSAIDs appear as idiosyncrasic reaction with or without immunoallergic reactions.1–13 Their mechnisms are only partially elucidated for most of them.1,3–9 The diagnosis of NSAID hepatotoxicity is frequently difficult because of the absence of specific clinical features.9,12 It relies mainly on the elimination of other causes and on chronological criteria.9,12 Apart few specific situations, liver biopsy is generally useless.15,16 This reinforce the interest of using specific causality assessment methods. There is no specific treatment of liver injury apart to stop the administration of the offending drug. In case of past liver injury caused by a NSAID, drugs of the same chemical family should be avoided to prevent cross-hepatotoxicity.8,9 In contrast, there is no contra-indication to use a NSAID of another chemical family.9
NEW BIOLOGICAL MARKERS OF DRUG-INDUCED LIVER INJURY17–20>There is an important need to get new markers for diferent steps of idiosyncratic DILI: a) the recognition of real liver injury and its type; the severity of liver injury; the causality of liver injury and the role of DILI and early diagnosis compared to current diagnositc rules (reviewed in reference 13). Recently, new biomarkers of hepatotoxicity have been developed to contribute to an early diagnosis of DILI and predict the severity of liver injury as compared to current diagnostic rules (reviewed in reference 17). The new biomarkers include GLDH (Glutamate dehydrogenase) and SDH (Sorbitol dehydrogenase) proposed as marker for hepatocyte necrosis;17–19 Cytokeratin 18: (caspase-cleaved CytoKeratin-18), a cytoskeletal protein that is very abundant at the hepatic but nonspecific level. Keratin may be a prognostic marker for liver injury because it is markedly higher in patients who have died or transplanted after paracetamol overdose compared to patients who have spontaneously recovered. It has been proposed as marker for apoptosis,17–19 HMGB1 (high mobility group box 1), a chromatin binding protein that is passively released by necrotic cells and participates in the activation of the immune system as is the case in some idiosyncratic hepatitis;17–19 (receptor-1) proposed as marker for immune activation.17 Other proposed biomarkers included M-30 (apoptosis), M-65 (apoptosis/necrosis), and microRNA-192 (unspecified liver damage),17–19 MCSFR1 (macrophage colony stimulating factor receptor 1): a highly increased marker in cases of idiosyncratic hepatotoxicity secondary to an analgesic, flupirtine;18,19 osteopontin: a protein associated with the case of severe drug hepatitis associated with a poor prognosis;17–19 bile acids: the increase of certain bile acids (glycochenodeoxycholic acid, taurochenodeoxycholic acid, taurocholic acid) has been demonstrated in some cases of hepatotoxicity (flupirtine) even in the absence of biological cholestasis.17–19 Despite potentially promising, these new biomarkers exhibit some limitations as recently stressed.17 Indeed, ideally, a biomarker of DILI should not only be the signature of a liver injury but also identify the offending drug or, at least, a class of chemical entities.
GENETIC FACTORS9,10,18,20Many links between drug and genetic hepatotoxicity have been established. In the NSAID category, the best example is lumiracoxib, currently withdrawn from the market, and its association between hepatic toxicity and HLADQA1*0102.10,18,20 The delay in obtaining the results and their cost did not make it possible to use the search for these genetic factors before the prescription of drugs. They are currently used retrospectively to improve understanding of the mechanisms of toxicity. In the coming years, the availability easy-to use genetic tests might facilitate the diagnosis and help to predict the risk of hepatotoxicity of drugs, including NSAIDs.18,20 However, the usefulness of genetict testing for the diagnosis and prediction of drug-induced liver injury is still a matter of discussion.
CONCLUSIONS- •
NSAIDs are one of the main causes of acute hepatitis especially hepatocellular type.
- •
The incidence of severe cases is low but it is one of the most prescribed pharmaco-therapeutic classes in the world.
- •
Most of NSAID induced acute liver injuries are associated with idiosycratic patterns and only partially understood mechanisms with the exception of aspirin.
- •
In case of hepatitis, the reintroduction of the incriminated NSAID or of the same class must be proscribed. Another class of NSAIDs can be used.
- •
New tools to help diagnosis and predict NSAID-related hepatotoxicity are forthcoming in a near future.