Nowadays the contraindication for transjugular intrahepatic portosystemic shunt (TIPS) in patients with portal vein thrombosis (PVT) had been modify. The experience and technology have reduce the complications for this procedure. We report a case of refractory ascites and portal vein thrombosis to emphasize the role of TIPS in the treatment for this condition.
PVT is one of the most common vascular disorders of the liver; its importance relies because of its significant morbidity and mortality. Large cohorts have reported a global PVT prevalence of 1%, but in some risk groups can be up to a 26%.1 The incidence of PVT in cirrhosis is less clearly defined, but reported as 16% by Amitrano, et al.2 in a group of patients with liver disease (LD) followed prospectively. TIPS is commonly performed for refractory ascites, refractory variceal bleeding, hepatic hydrothorax, and Budd-Chiari syndrome.
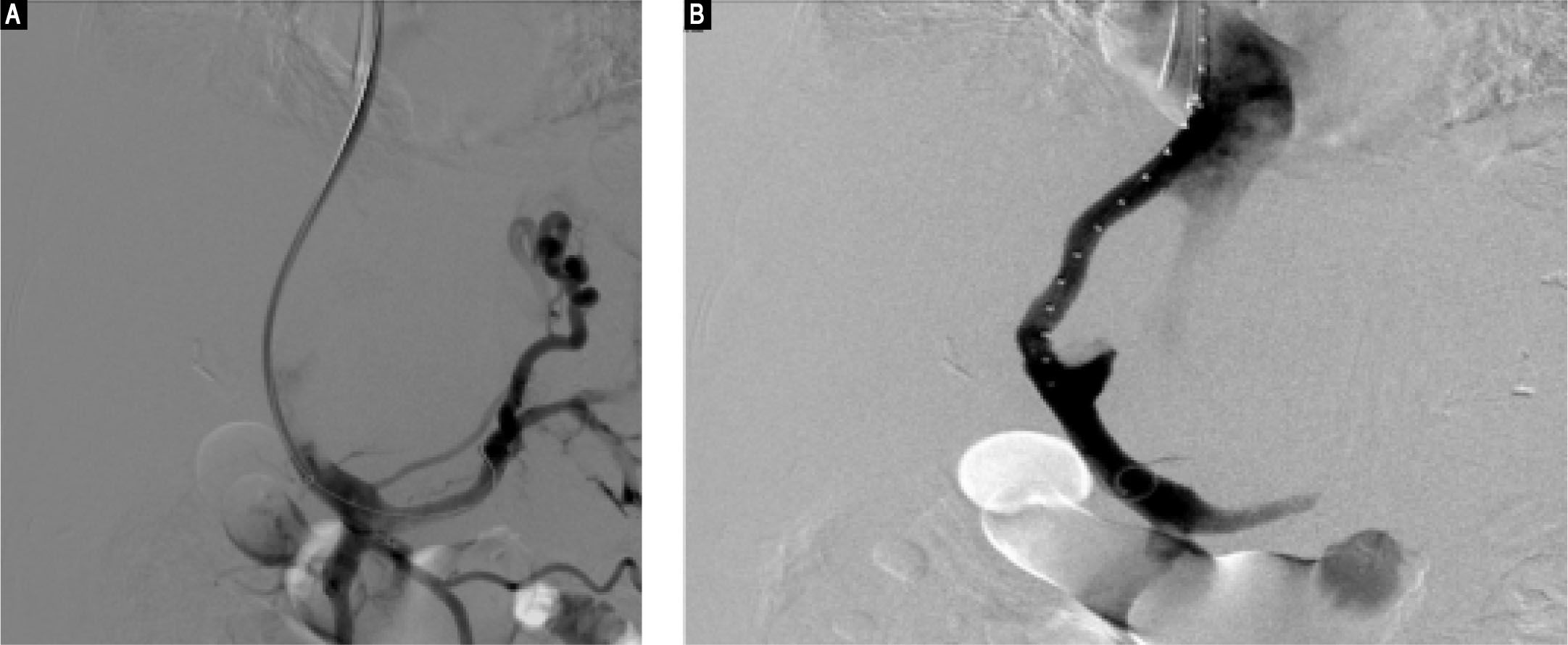
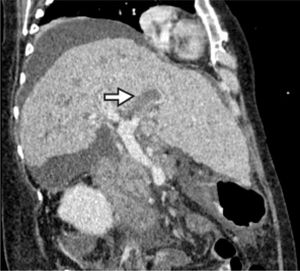
Case PresentationA 67-year-old female with hepatic cirrhosis associated to VHC genotype 2b/2c infection (CHILD PUGH: B (10 points) + MELD: 14 points + MELD Na: 19 points) diagnosed in 2007. She received treatment with interferon and rivabirin with no response. In 2015 she received treatment with sofosbuvir and ribavirin without response. She has present two episodes of variceal bleeding treated endoscopically succesfuly. In her last hospitalization because variceal bleeding she was diagnosed with a portal vein thrombosis and received anticoagulation with enoxaparin (Figure 1). Two weeks later she presented with refractory ascites for these we decided to treat her with TIPS (Figure 2).
The echocardiography previous the procedure reported an EF 64%, TAPSE 19, PSAP 42. During the procedure they reported a portal pressure of 30 mmHg, after the placement of a 10 mm, 8 cm x 2 cm prosthesis she had a portal pressure of 6 mmHg, no complications were reported during the procedure.
DiscussionPVT is a common disorder in patients with LD, we suggest that it is important to consider prophylactic therapy to prevent thrombotic disease in this patients who are at high risk of bleeding.3
The evidence and experience of other centers demonstrate that TIPS is not always contraindicated in PVT, and indeed may be an ‘indication’ in some cases.
Some authors asseverated that the increasing experience with the use of widely available imaging guidance has made it possible to manage the patient undergoing TIPS with complete PVT.4 Luca, et al. showed that TIPS is an effective treatment in PVT with cirrhosis. Their case series showed a 57% complete resolution of the thrombus. Moreover, a conservative attitude of placing the stent towards the portal side was considered.5
TIPS is not a contraindication to treatment PVT, the importance is the selection cases for this kind of treatment and clearly the expertise of the specialist who perform the intervention.