(OR = 2,44; IC del 95%, 1,93-3,09). Otros factores asociados son: considerar la citología necesaria, estatus socioeconómico alto/medio alto, cobertura sanitaria privada o mixta, edad de 40 a 50 años y municipio mayor de 100.000 habitantes. Conclusiones. La mitad de las mujeres españolas de 40 a 70 años se ha realizado la citología. El uso de la prueba se relaciona especialmente con la actitud de la mujer. Los profesionales deberían tomar conciencia de la importancia de su papel en la citología de cribado.
Introduction
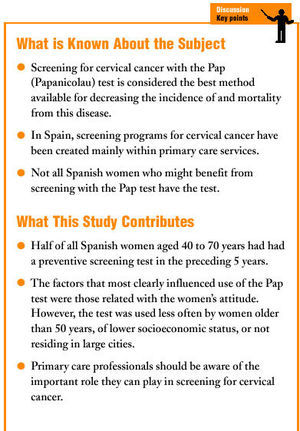
In developed countries the incidence and mortality rates from cervical cancer are very low, a fact attributed in large part to screening with the Papanicolau (Pap) test. If the quality of testing is appropriate, this test is considered the best method available for preventing the disease, although evidence of its efficacy has come from observational studies only.1,2
Periodic Pap tests are recommended for sexually active women, especially when risk factors such as human papilloma virus infection, sexual promiscuity or lower socioeconomic status are present.3 The age group comprising women between 35 and 65 years old benefits most from the test, which is considered unnecessary past the age of 65 if the women has been tested previously with normal results.4,5 The most widely recommended frequency is for repeat testing every 3 to 5 years after two consecutive normal results on annual tests. More frequent testing adds few benefits while notably increasing costs.4 The use of Pap testing has been related with sociodemographic, social and health factors, and with the woman's information about and attitude toward the test.6-8
In Spain, cervical cancer screening programs based on the Pap test have been developed mostly within primary care settings. Such programs are often opportunistic, and are used by women who actively seek health care.5,7 Population-based screening programs are not given high priority because of the low incidence and low mortality of the disease.9 Opportunistic screening, however, is related with low coverage and more frequent testing of younger women without risk factors, whereas it is older women of lower socioeconomic status who benefit most from Pap testing.1,10,11
The aim of this study was to determine the percentage of women aged 40 to 70 years who had had at least one Pap test in the preceding 5 years (use of the Pap test), and the factors associated with Pap testing.
Material and Methods
Study Population
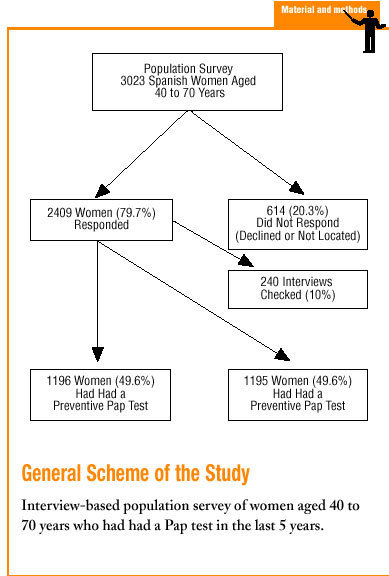
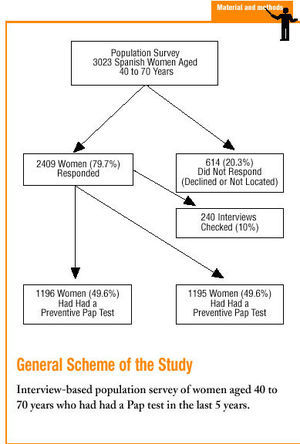
A population survey was done in women aged 40 to 70 years residing in Spain (excluding Ceuta and Melilla). The numbers of participants to be sampled were calculated on the basis of staged conglomerate sampling. In the first stage census sections were stratified into 9 categories by autonomous community and population of the town or city of residence, classified as fewer than 2000 inhabitants, 2001-5000, 5001-10 000, 10 001-30 000, 30 001-50 000, 50 001-100 000, 100 001-200 000, 200 001-500 000 and more than 500 000 inhabitants. The second stage considered households, and the third stage considered women aged 40 to 70 years living in each household. Census sections were chosen by simple random sampling, and strata were sampled proportionately according to the number of women aged 40 to 70 years in each stratum. Households were chosen by the random walk method, and all interviews took place in the participant's home. Sample size was calculated by assuming that 50% of the women had had a previous Pap test, with a 95% confidence interval and a sampling error of ±2, based on the estimate of the number of women aged 40 to 70 years in the year 2000 provided by the National Statistics Institute (Instituto Nacional de Estadística). The total sample consisted of 2409 interviews of 3023 women who were contacted, for a nonresponse rate (declined to participate or not located) of 20.3%.
Method
Information was collected during October 2000 with personal interviews and a standardized questionnaire. The questionnaire was pretested in 30 women from 3 different municipalities, and the final questionnaire incorporated modifications to improve the comprehension of some questions. Interviewing was done by a private firm specialized in survey studies, and all staff were trained appropriately in the use of the questionnaire. If the woman was not at home, 3 more visits were attempted at different times of day. The questionnaire included use of Pap testing as the dependent variable, and independent variables consisted of factors potentially related with use of the test. Performance of the Pap test was explained when the participant was unfamiliar with the procedure. The independent variables were: a) sociodemographic factors including socioeconomic status, recorded on the basis of level of education and employment status; b) social and health factors, and c) variables regarding information and attitudes. Reliability of the sampling procedure was checked in a random sample of 240 women by a private survey company different from the one responsible for interviewing the main sample. These participants were contacted by telephone and asked again whether they had had a Pap test, and their reasons for having the test. The correlations were significant at 0.65 and 0.54 (P<.01), respectively.
Statistical Analysis
We calculated the percentage of women who had had at least one Pap test in the 5 years preceding the interview, and the 95% confidence interval (CI). Univariate analysis of the association between each factor and the dependent variable was done with the chi-squared test for categorical variables and Mann-Whitney's U test for quantitative variables. The magnitude of association (odds ratio [OR] and CI) was calculated with reference to the category of the variable with the lowest percentage of women who had had a Pap test. Multivariate analysis with logistic regression was done to evaluate the weight of each factor separately. All analyses were done with SPSS v.10.0 software.
Results
About half (49.6%; 95% CI, 47.6%-51.6%) of the women had had at least one Pap test in the preceding 5 years. Univariate analysis (Table 1) showed the factors most strongly associated with use of the test to be intention to have a Pap test in the future (OR, 15.76; CI, 12.14-20.45), considering the test to be necessary even when the woman did not feel ill (OR, 10.83; CI, 8.25-14.22), upper (OR, 8.79; CI, 5.53-13.96) and middle-upper socioeconomic status (OR, 5.40; CI, 3.85-7.58), doctor´s advice (OR, 5.90; CI, 4.94-7.03), and fear of a diagnosis of cancer not being an obstacle to having the test (OR, 5.82; CI, 3.54-9.55). Use of the test was also associated with other factors such as marital status, size of the town or city of residence, highest level of education completed, employment status, number of children, number of pregnancies, type of health care, having a test more than 5 years ago, having a relative or friend with cervical cancer, perception of the test as safe, perception of cervical cancer as a disease that can be cured if detected early, and inconvenience not being an obstacle to having the test. No statistically significant associations were found between use of the test and visits to the general practitioner during the preceding 3 years, and perceived likelihood of cervical cancer compared to other women the same age. In the adjusted model (Table 2) the categories of factors were grouped by OR. Excluding the absence of a previous history of gynecological disease, the factors most strongly associated with greater use of the test were intention to have the test (OR, 4.76; CI, 3.40-6.65), fear of the diagnosis not being an obstacle to having the test (OR, 3.22; CI, 1.77-5.85), previous Pap tests (OR, 2.59; CI, 2.06-3.27), doctor's advice (OR, 2.44; CI, 1.93-3.09), and considering the test necessary even though the woman does not feel ill (OR, 2.42; CI, 1.67-3.50). Other factors associated with use of the test were upper or middle-upper socioeconomic status, private or combined medical care, age 40-50 years versus age 51-70 years, and residing in a city with a population of more than 100 000. The model correctly predicted 78.7% of the cases in the whole sample, and 81.6% of the cases among women who had had previous Pap tests.
Discussion
Screening of women with the Pap test is a common and widespread practice in developed countries.6,12 However, we found that half of the Spanish women aged 40 to 70 years surveyed in this study had not had a Pap test in the preceding 5 years.
Contact with health services determines, to a great extent, whether a woman has a Pap test.13 In the present study, however, use of the test was not associated with visits to the general practitioner despite the existence of screening programs for cervical cancer in primary care. This lack of association may be related with frequent Pap testing in the gynecologist´s office.14 We found that the doctor's advice was associated with use of the test; however, the test is not often recommended by health professionals.15 In our study the most relevant factors influencing use of the test were related with women´s attitudes. It has been shown that lack of knowledge about cervical cancer and the Pap test, fear of gynecological examinations and fear of a diagnosis of cancer were substantial obstacles to having the test.1,7 We believe it worthwhile to investigate in future studies the factors that influence women´s intention to have the test. Like other authors, we found that the Pap test is used more frequently by younger women (younger than 50 years in the present study), women of higher socioeconomic status, and women with access to private health care.6,8 Women with private medical insurance often make greater use of preventive services, and visits to the gynecologist are more frequent in certain strata of educational level and socioeconomic status.6 In the present study, univariate analysis showed a higher level of education to be associated with use of the Pap test, although the multivariate analysis failed to confirm the association--possibly because of some degree of association between age and level of education. As in earlier studies, we found that women who lived in larger cities had more Pap tests than women living in rural areas.16
The main limitations of this study are those inherent in any cross-sectional design and in any survey study in which the source of information is the participants themselves. However, the information provided by the women seems to be quite accurate.8 We believe that primary care professionals should be aware of the importance of their role in encouraging women to have screening tests for cervical cancer, and in providing access to testing for women who are most likely to benefit from testing but who receive such tests less frequently.