Reconstruction of the oesophagus continues to be a difficult operation that requires the participation of an experienced surgical team. There are few options, and reconstruction has been traditionally done with the stomach or interposition of the colon. In recent years, as a consequence of advances in microsurgery techniques, interposition of the jejunum with the increased vascular flow offered by microsurgery (“supercharged”) has been used more and more often and can be considered a useful option.
The present case illustrates an oesophageal reconstruction in 2 phases, after failed colon interposition, using a radial forearm free flap (first step) and “supercharged” jejunal interposition (second step).
A 58-year-old woman was admitted to the Emergency Department at a third level university hospital after having voluntarily ingested a caustic liquid. After the patient was stabilised, gastroscopy showed grade 3 esophagitis (Zargar classification) and necrosis of the gastric mucosa, with no airway compromise. We performed oesophagogastrectomy, terminal cervical oesophagostomy and jejunostomy with a feeding tube. After 52 days in the Intensive Care Unit (ICU) with prolonged mechanical ventilation, tracheostomy and 21 days in the Hospitalisation Unit, the patient was discharged for transfer to a psychiatric hospital. Eighteen months later, interposition of the right colon was carried out through the retrosternal approach. On the fifth day, the patient presented dehiscence of the proximal anastomosis, mediastinitis and pneumonia, and she was treated in the ICU for 62 days. Once stabilised, the endoscopy showed complete proximal stenosis. Computed tomography showed the incorrect location of the interpositioned colon. Laryngoscopy demonstrated no alterations in vocal cord function. The patient was discharged with jejunostomy feeding and showed normal breathing and speaking.
The General Surgery team then consulted with the Plastic Surgery team for a second reconstruction surgery. In this phase, the patient's main problem was constant drooling and the risk of recurring aspiration pneumonia. She could not sleep more than 2h at a time because she began to drown in her own saliva and needed constant suction while awake. Before planning the surgical treatment, the patient started a multidisciplinary recovery programme, which included optimal nutrition, regular exercise and physiotherapy. The patient demonstrated great motivation throughout this 6 month period, and the surgery was scheduled.
The surgical exploration of the mediastinum to try to re-establish the colonic interposition showed an atrophic colon that was not considered apt for reconstruction, which was expected.
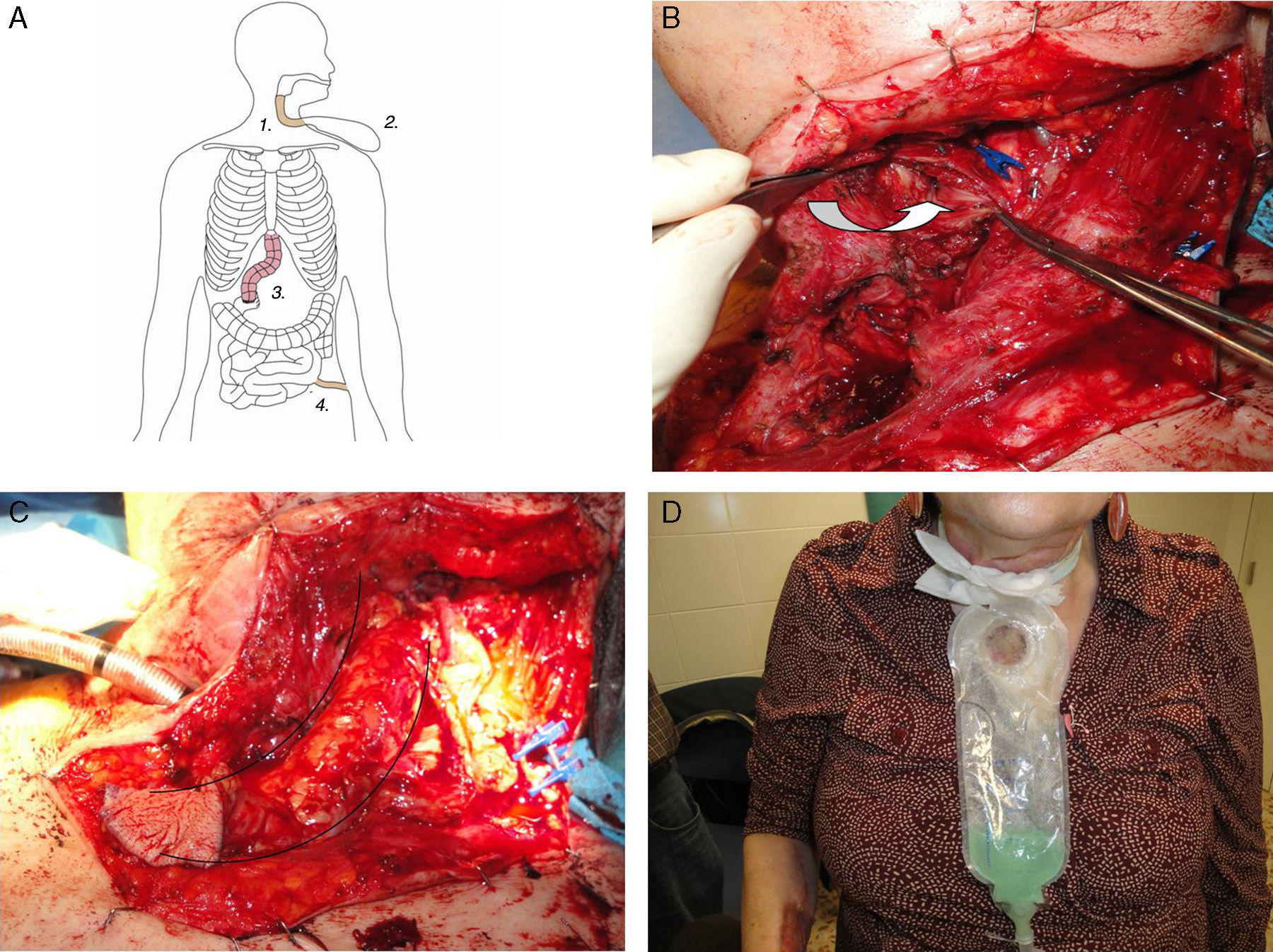
Thus, in an initial stage (Fig. 1), a forearm free flap was obtained and a tube was created to connect the pyriform sinus to the skin in the neck (Fig. 1B and C), in order to resolve the drooling problem by collecting the saliva in a bag (Fig. 1D). Partial resection of the manubrium provided wider access. Microsurgical vascular anastomoses were created to the lingual artery, lingual vein and external jugular vein.
(A) First stage of the intervention: forearm free flap (1), saliva collection bag (2), failed interposition of the colon (3) and jejunostomy (4); (B) Dissection of the neck and identification of the pyriform sinus (arrow); (C) Forearm free flap forming a tube used to connect the pyriform sinus with neck skin; (D) Patient with saliva connection bag.
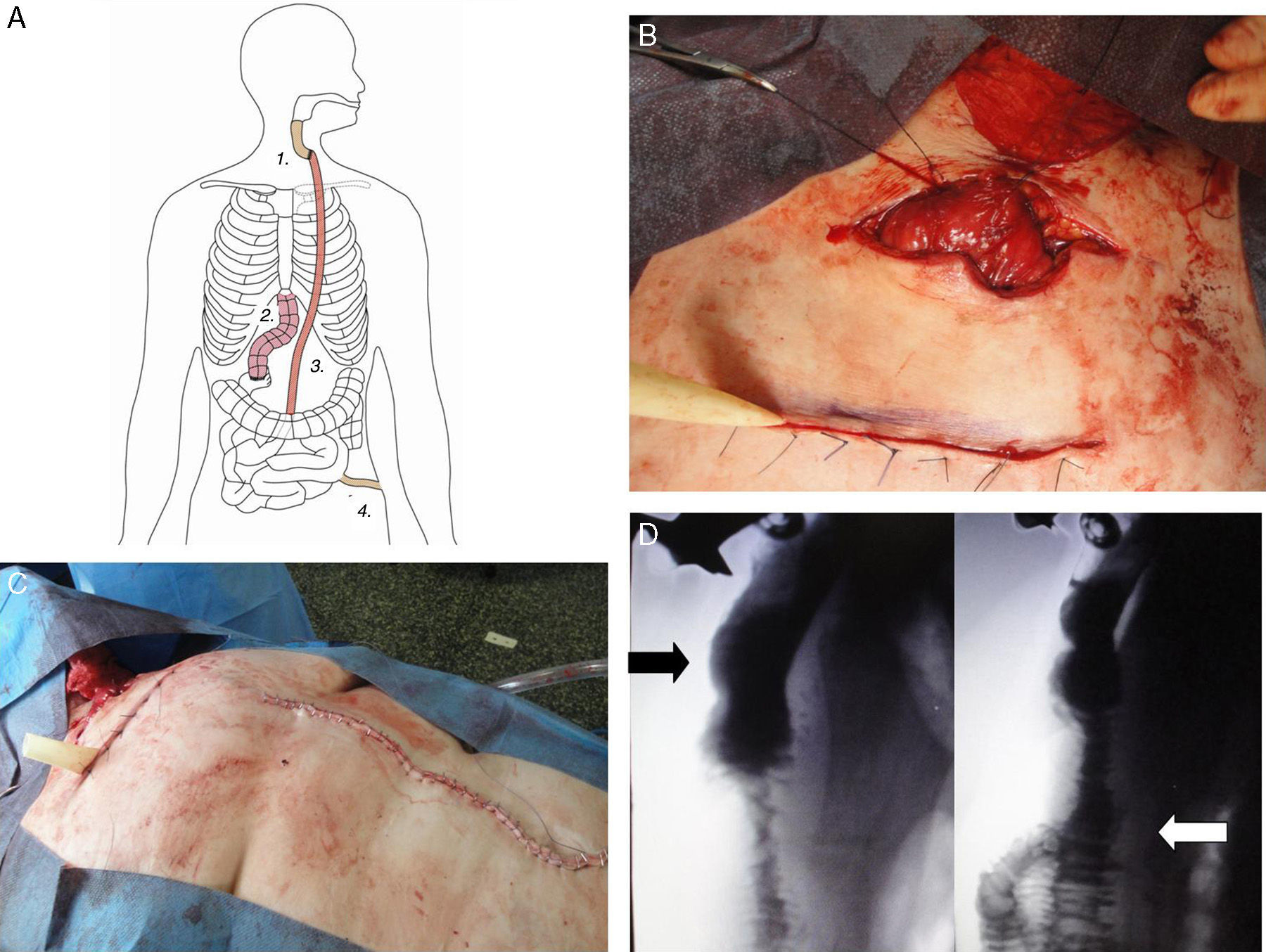
The second stage was completed with the collaboration of the Plastic Surgery Department 10 weeks later. It involved the interposition of a long jejunal section (supercharged), which was connected to the distal end of the radial forearm flap (Fig. 2A–C). A subcutaneous tunnel was created in the abdominal wall and in the thorax to pull the jejunum up to the neck. Microsurgery was used to create the anastomosis of the vascular pedicle of the jejunum to the internal thoracic vessels to increase blood flow. Finally, the jejunojejunal anastomosis was completed with a Roux-en-Y reconstruction to re-establish intestinal continuity, and a jejunal feeding tube was inserted.
(A) Second stage of the procedure: forearm free flap (1), failed interposition of the colon (2), “supercharged” pedunculated jejunal flap (3), jejunostomy (4); (B) “Supercharged” pedunculated jejunal flap connected to the distal end of the forearm radial flap; (C) Midline laparotomy; (D) Barium swallow study showing re-established continuity of the digestive tube, forearm radial flap (black arrow) as well as the “supercharged” pedunculated jejunal flap (white arrow).
One week later, a barium swallow test showed that the continuity of the digestive tube had been re-established (Fig. 2D) and the patient began to eat. One month after surgery, she presented mild dysphagia but did not need complementary nutrition, so the jejunal tube was withdrawn. Currently, 6 months after the operation, the patient is able to eat, presents no drooling, has had no pneumonia and her quality of life has improved greatly.
This is a special case in which a multidisciplinary team was able to perform a complex oesophageal reconstruction after having previously performed a total esophagogastrectomy with later failure of a colonic interposition. As far as we know, there are very few articles in the literature that describe similar cases. The surgical team evaluated several alternatives to approach this challenge. We contemplated the possibility of a single-stage reconstruction, with interposition of the jejunum and microsurgical anastomosis to the thoracic vessels, according to the “supercharged” method by Swisher et al.8 This, however, was ruled out because the patient had had 2 previous laparotomies and the possibility of multiple adhesions that could complicate mobilisation of the small bowel, while it was foreseen that the distal tension would be excessive to ensure the success of the operation. A 2-stage reconstruction seemed the best option. The forearm free flap was 8cm in length and allowed us to connect the hypopharynx with the lower part of the neck. After this stage, the patient's quality of life improved as the drooling problem had been resolved. After the forearm donor area had healed, the second stage was scheduled. The subcutaneous approach to pull the jejunum up to the neck is not the first option. In fact, the posterior mediastinal and retrosternal approaches are usually preferred, but neither of these was applicable due to the mediastinal fibrosis. We therefore opted to use the subcutaneous method. Partial resection of the manubrium was necessary to widen the access to the neck. Furthermore, this reduces postoperative oedema and provides access to internal thoracic vessels for microsurgery. Before the operation, it is essential for a nutritionist and physical therapist to work with the patient and optimise his/her condition. Caution should be used, because the loss of saliva can lead to hypokalaemia. The nutritionist indicated the use of a high-calorie diet with vitamin B12 supplements.
The method provides a safe way to re-establish the continuity of the digestive tract when all other options have been ruled out. It requires close collaboration among surgeons as well as careful patient selection and preparation.1–8
Please cite this article as: Dewever M, Gomes T, Madrazo Z, López A, Farrán L, Viñals JM. Fallo de la interposición de colon tras esofagogastrectomía: ¿cuál es el siguiente paso? Cir Esp. 2016;94:54–57.