Laparoscopic cholecystectomy (LC) performed as day-case (DC) surgery has more unexpected admissions than most day-case procedures. We revised the literature about factors associated with unexpected admissions in LC as well as reconversion to open laparotomy and we investigate these factors in our series.
MethodsRetrospective cohort study, period 1999–2013 (511 cases). We study factors that in the literature have been associated with unpredicted admissions in DC or reconversion.
ResultsIn the period 1999–2013 511 patients were included (166 male/345 female), median age 53 years. Surgical indication was: Symptomatic cholelithiasis (386 cases), previous episode of cholecystitis (52 cases), biliary pancreatitis (47 cases) and ERCP for common duct stones (11cases). 70% were discharged on the same day, 13% overnight and 17% stayed longer than 24h. Reconversion rate was 3.3%, readmission rate 2.8% and reoperation rate 1.2%. Bivariant study showed significant statistical association with age 65 or, ASA classification II or higher, previous admission for acute cholecystitis and logistic regression showed them to be significantly associated with readmission (sensibility: 10.6%, specificity: 98.6%, R2 coefficient: 0.046–0.066).
ConclusionsThe model's predictive capacity is null. We think that factors other than indications are responsible for the high proportion of failure showed by LC in DC.
La colecistectomía laparoscópica (CL) como cirugía mayor ambulatoria (CMA) presenta un número de ingresos imprevistos mayor que otros procedimientos de CMA. Revisamos la bibliografía referente a factores asociados a ingresos imprevistos en CMA y a conversión a cirugía abierta e investigamos estos datos en nuestra serie.
MétodoEstudio de cohorte retrospectiva del periodo 1999 a 2013 (511 casos). Se estudian los factores que en algún estudio previo han mostrado una posible asociación de ingreso no previsto o conversión.
ResultadosEn el periodo 1999–2013 fueron incluidos 511 pacientes (166 hombres/345 mujeres) con mediana de edad de 53 años. La indicación quirúrgica fue: colelitiasis sintomática (386 casos), episodio previo de colecistitis (52 casos), pancreatitis biliar (47 casos) y CPRE por coledocolitiasis (11 casos). El 70% fueron dados de alta en el mismo día, ingresaron una noche el 13% y más de 24h, el 17%. La tasa de conversión fue del 3,3%, la de reingreso del 2,8% y la de reintervención del 1,2%. El estudio bivariante muestra asociación estadística significativa entre edad mayor de 65 años, clasificación ASA II o superior, ingreso previo por colecistitis y pared vesicular engrosada en ecografía. La regresión logística identifica 3 factores predictores independientes: edad mayor de 65 años, clasificación ASA II o superior, ingreso previo por colecistitis. (sensibilidad: 10,6%; especificidad: 98,6%; coeficiente R2: 0,046–0,066).
ConclusionesLa capacidad predictiva del modelo es nula. Pensamos que hay otros factores ajenos a las indicaciones que son responsables del elevado porcentaje de fallo de CMA que muestra la CL.
Laparoscopic cholecystectomy (LC) is at present not a new technique. Next year will be the 30th anniversary of the first LC by Mühe in 1985.1 In France Mouret started to use the technique in 1987, while in the USA McKerrnan and Saye first used it in 1988.1 although it was popularised by Reddick and Olsen, who published their first description of ambulatory cholecystectomy in 1990 (A-CC).2 LC was swiftly accepted in Spain, coinciding with the development and expansion of ambulatory surgery (AS).3 Nevertheless, it has not become general as AS in our country for reasons that are not very clear, perhaps due to the fear of serious postoperative complications after discharge4 or the difficulty of fitting it into the planned working schedule of major hospitals.5
On the other hand, the number of unplanned admissions following AS-CC is far higher than it is after other AS6 procedures. Attempts have been made to improve these results by studying the factors associated with unplanned admission after AS-CC with varying results.7–11
We have been performing AS-CC in Laredo Hospital since 1999.12 Our inclusion criteria for AS-CC are not very restrictive and in general do not differ from those used in other AS procedures, such as inguinal hernia. This is why we believe that our series may be of use in investigating the factors associated with the failure of AS in LC.
MethodStudy Design, Cases and Inclusion CriteriaWe carried out a retrospective cohort study by revising all of the cases included in the computerised surgical waiting list system for the procedure “laparoscopic cholecystectomy”) (CIE-9-mc 51.23) with “AS” as the admission mode from 1999 to 2013. The inclusion criteria for AS-LC were: indication of cholecystectomy due to symptomatic or complicated cholelithiasis (acute cholecystitis, acute pancreatitis, choledocholithiasis) and the absence of contraindications for AS due to medical reasons (ASA I and II and stable ASA III) or social reasons (patient able to comprehend self-care, living accompanied by responsible family members less than 45min transport time from the hospital and with appropriate facilities in their home). During this 14 year period there have been many changes in the staff of the Surgery Department so that, in a 6-surgeon unit, the cases included in this revision were indicated and operated on by 15 different surgeons.
Surgery and Postoperative PeriodPatients are admitted to hospital on the day of surgery at 07:30. The day before admission, in the evening, they are given a dose of low molecular weight heparin in their primary health care centre as prophylaxis against thromboembolic disease. They are operated on at the first hour of the surgical session, usually just one case of cholecystectomy but occasionally 2, so that the last case does not finish later than 12:00. Antibiotic prophylaxis with Cefazolin 2g is given in a single dose prior to the operation in patients with a history of cholecystitis, pancreatitis, choledocholithiasis or those who are older than 70 years old.
The anaesthesia technique has evolved over the period that includes the entire series. Systematic prophylaxis is given against postoperative nausea and vomiting. At the start of the series this consisted of Dihydrobenzoperidol, after which Ondansetron was used. Surgeons use the technique they are the most familiar with for the LC (87.3% “French” technique with 3 or 4 trocars; and 12.7% using “American” technique). Intraoperative cholangiography was only used in 1.2% of cases. Laparoscopic trocar wounds are systematically infiltrated with 0.5% Ropivacaine at the end of the operation. After the operation (SO) patients are taken to reanimation where they remain for about 2h and then to the day hospital where oral tolerance and walking commence, habitually at about 17:00. Discharge is given by Surgery and Anaesthesia (the on-duty surgeon and anaesthetist) between 20:00 and 21:00. This is why we do not count the postoperative stay (reanimation+day hospital time) in hours, as this usually lasts about 9–10h.
ComplicationsWe use the term “AS failure” for all admissions that have needed at least one night of hospitalisation, even though the discharge was issued before the first 24h. Demographic, clinical and surgical data are collected, paying special attention to the reasons for hospitalisation in cases of “AS failure”, as well as postoperative complications, repeat operations and admissions.
Data PreparationWe describe our series by using proportions, percentages and non-parametric statistics such as the median or interquartile range, given that the population did not have a normal distribution (age and surgical time) and make comparisons between qualitative data using the chi-squared test. We compare quantitative data using the Kruskall–Wallis test. Multivariate analysis is undertaken using logistic regression. Version 15.0 of the SPSS statistical programme was used.
ResultsIn the period from 1999 to 2013 511 patients were included in the surgical waiting list for ASLC (166 men and 345 women) with a median age of 53 years (interquartile range: 24 years). A total of 5 cases did not meet the basic criteria for AS and were excluded from the study. The following results refer to the remaining 506 cases.
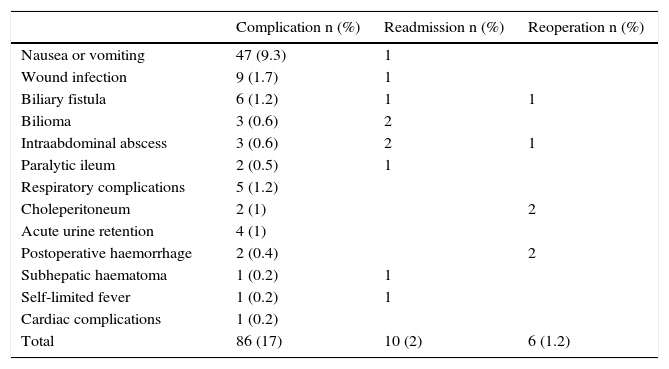
The surgical indication was: symptomatic cholelithiasis in 386 cases (76.3%), acute cholecystitis treated medically with previous admission in 52 cases (10.3%), biliary pancreatitis in 47 cases (9.3%) and choledocholithiasis treated using ERCP in 11 cases (2.2%). (There are also 7 other ERCP prior to the SO, 2 in cholecystitis and 5 in pancreatitis) as well as gallbladder polyps without cholelithiasis in 10 cases (1.9%). A total of 250 of the patients (49.4%) had associated disease. These were classified ASA II in 240 cases (47.4%) and ASA III in 10 cases (2%). 198 patients (39.1%) had a body mass index (BMI) of 30 or more. LC was performed as AS in 353 cases (70%), while 153 (30%) required admission: for one night in 65 cases (13%) and for longer in 88 (17%). 10 patients were readmitted: 2 due to an uninfected subhepatic collection (“bilioma”), 2 due to subhepatic abscess, one because of nausea and vomiting, one due to wound infection, one due external biliary fistula, one for a subhepatic haematoma, one due to a paralytic ileus and one due to fever of undetermined origin (Table 1). 6 operations were repeated. Of this only one was an emergency, due to cystic artery haemorrhage. This was diagnosed immediately after the operation while the patient was still in reanimation. Another operation was repeated due to haemorrhage at 24h following a SO with difficult haemostasis, which showed excessive bleeding through the drainage. Two cases of choleperitoneum were also re-operated: one due to leakage through the cystic duct and the other due to complete section of the choledochus which required hepaticojejunostomy. One case was also operated again for biliary fistula, which required the placement of a Kehr tube and a subhepatic abscess in which percutaneous drainage was insufficient (Table 1). Only 2 of the readmitted patients were operated on again.
Postoperative Complications.
| Complication n (%) | Readmission n (%) | Reoperation n (%) | |
|---|---|---|---|
| Nausea or vomiting | 47 (9.3) | 1 | |
| Wound infection | 9 (1.7) | 1 | |
| Biliary fistula | 6 (1.2) | 1 | 1 |
| Bilioma | 3 (0.6) | 2 | |
| Intraabdominal abscess | 3 (0.6) | 2 | 1 |
| Paralytic ileum | 2 (0.5) | 1 | |
| Respiratory complications | 5 (1.2) | ||
| Choleperitoneum | 2 (1) | 2 | |
| Acute urine retention | 4 (1) | ||
| Postoperative haemorrhage | 2 (0.4) | 2 | |
| Subhepatic haematoma | 1 (0.2) | 1 | |
| Self-limited fever | 1 (0.2) | 1 | |
| Cardiac complications | 1 (0.2) | ||
| Total | 86 (17) | 10 (2) | 6 (1.2) |
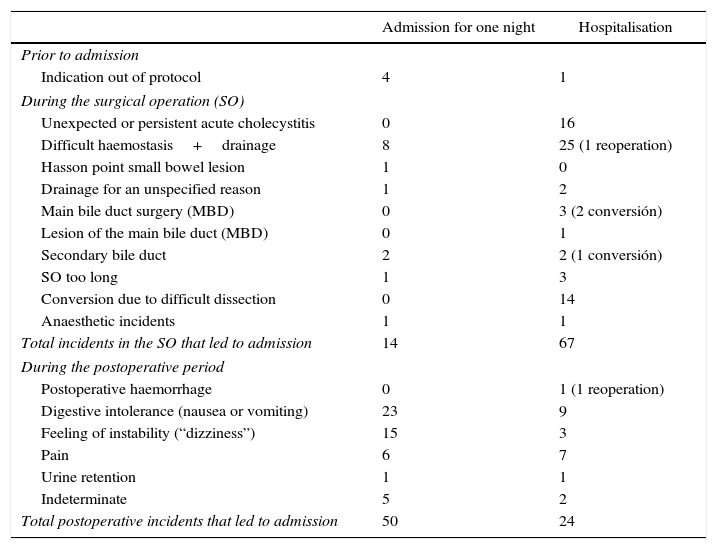
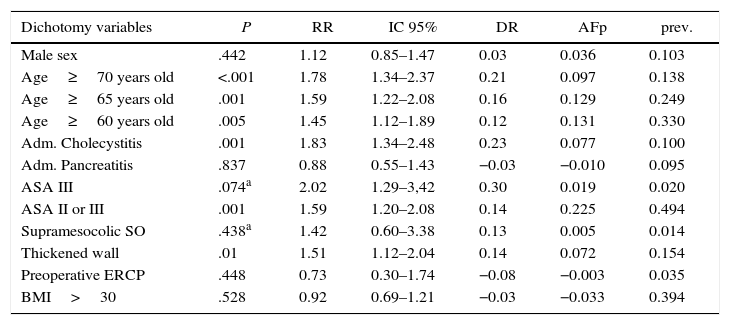
The reasons for “AS failure” are shown in Table 2. Bivariate study of possible predictive factors for “AS failure” are shown in Table 3. Multivariate analysis with binary logistic regression showed that independent predictive factors for “AS failure” were age above 65 years old (P .04; coefficient: 0.472; OR: 1.603 with an ICof 95%: 1.022–2.516), previous admission for cholecystitis (P .007; coefficient: 0.827; OR: 2.286 with an IC of 95%: 1.252–4.174), and risk of ASA II–III (P .022; coefficient: 0.478; OR: 1.613 with an IC of 95%: 1.070–2.432). The model shows overall significance of 0.0001 with an R2 determination coefficient of from 0.046 (Cox and Snell) and 0.066 (Nagelkerke). As a predictive model, if we consider a probability of 0.5 or higher to be predictive, it has a sensitivity of 10.5% and a specificity of 98.6%, with 71.9% of correct classifications.
Reasons for Admission in “AS Failures”.
| Admission for one night | Hospitalisation | |
|---|---|---|
| Prior to admission | ||
| Indication out of protocol | 4 | 1 |
| During the surgical operation (SO) | ||
| Unexpected or persistent acute cholecystitis | 0 | 16 |
| Difficult haemostasis+drainage | 8 | 25 (1 reoperation) |
| Hasson point small bowel lesion | 1 | 0 |
| Drainage for an unspecified reason | 1 | 2 |
| Main bile duct surgery (MBD) | 0 | 3 (2 conversión) |
| Lesion of the main bile duct (MBD) | 0 | 1 |
| Secondary bile duct | 2 | 2 (1 conversión) |
| SO too long | 1 | 3 |
| Conversion due to difficult dissection | 0 | 14 |
| Anaesthetic incidents | 1 | 1 |
| Total incidents in the SO that led to admission | 14 | 67 |
| During the postoperative period | ||
| Postoperative haemorrhage | 0 | 1 (1 reoperation) |
| Digestive intolerance (nausea or vomiting) | 23 | 9 |
| Feeling of instability (“dizziness”) | 15 | 3 |
| Pain | 6 | 7 |
| Urine retention | 1 | 1 |
| Indeterminate | 5 | 2 |
| Total postoperative incidents that led to admission | 50 | 24 |
Predictive Factors for AS Failure: Bivariate Analysis.
| Dichotomy variables | P | RR | IC 95% | DR | AFp | prev. |
|---|---|---|---|---|---|---|
| Male sex | .442 | 1.12 | 0.85–1.47 | 0.03 | 0.036 | 0.103 |
| Age≥70 years old | <.001 | 1.78 | 1.34–2.37 | 0.21 | 0.097 | 0.138 |
| Age≥65 years old | .001 | 1.59 | 1.22–2.08 | 0.16 | 0.129 | 0.249 |
| Age≥60 years old | .005 | 1.45 | 1.12–1.89 | 0.12 | 0.131 | 0.330 |
| Adm. Cholecystitis | .001 | 1.83 | 1.34–2.48 | 0.23 | 0.077 | 0.100 |
| Adm. Pancreatitis | .837 | 0.88 | 0.55–1.43 | −0.03 | −0.010 | 0.095 |
| ASA III | .074a | 2.02 | 1.29–3,42 | 0.30 | 0.019 | 0.020 |
| ASA II or III | .001 | 1.59 | 1.20–2.08 | 0.14 | 0.225 | 0.494 |
| Supramesocolic SO | .438a | 1.42 | 0.60–3.38 | 0.13 | 0.005 | 0.014 |
| Thickened wall | .01 | 1.51 | 1.12–2.04 | 0.14 | 0.072 | 0.154 |
| Preoperative ERCP | .448 | 0.73 | 0.30–1.74 | −0.08 | −0.003 | 0.035 |
| BMI>30 | .528 | 0.92 | 0.69–1.21 | −0.03 | −0.033 | 0.394 |
| Quantitative variables | P | DA | IC 95% |
|---|---|---|---|
| Age | 0.001 | 4.738 | 2.03–7.45 |
| BMI | 0.865 | −0.865 | −0.79 to 0.75 |
AFp: attributable population fraction; ERCP: endoscopic retrograde cholangiopancreatography; IC: interval of confidence; SO: surgical operation; BMI: body mass index; Adm.: previous admission; DA: difference in averages; prev: prevalence in the series; DR: difference in risks; RR: relative risk.
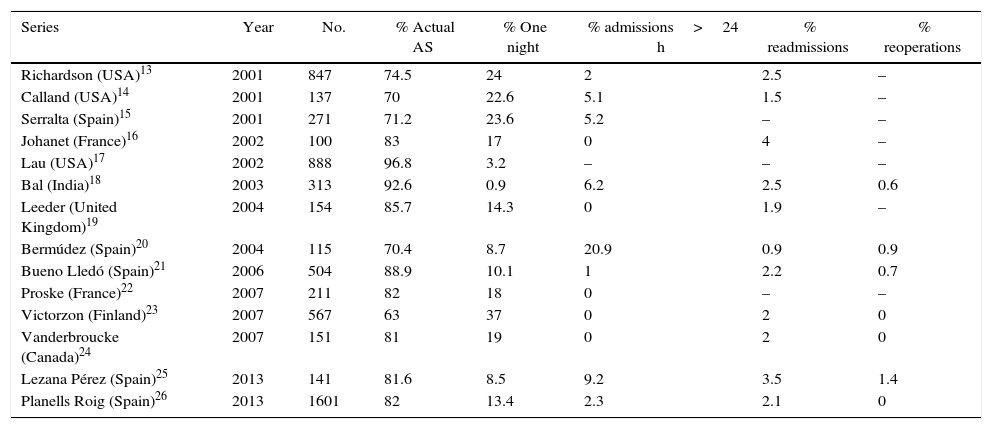
ASLC has not been widely included in usual practice. One of the reasons habitually suggested for this is the fear of serious complications arising after discharge4 and the difficulty of including programmes in major hospitals.5 The readmission rate is a key indicator, as it shows the patients who felt well at discharge and did not suspect that a complication would soon oblige them to seek admission again. In our series there were 10 readmissions (2.8%) (Table 1), a rate similar to those published by other authors13–26 (Table 4). The re-operation rate is another very important datum. In our series there were 6 re-operations (1.2%) (Table 1), only one of which was an emergency case due to cystic artery haemorrhage detected immediately after the operation while the patient was still in reanimation. Of the patients who were readmitted, only 2 required additional surgery: one for biliary fistula that required the placement of a Kehr tube and one due to subhepatic abscess. Our rate of complications is similar to those published by other authors.13,23,24,26 None of our patients died.
Admissions, Readmissions and Reoperations in Some AS Cholecystectomy Series.
| Series | Year | No. | % Actual AS | % One night | % admissions>24 h | % readmissions | % reoperations |
|---|---|---|---|---|---|---|---|
| Richardson (USA)13 | 2001 | 847 | 74.5 | 24 | 2 | 2.5 | – |
| Calland (USA)14 | 2001 | 137 | 70 | 22.6 | 5.1 | 1.5 | – |
| Serralta (Spain)15 | 2001 | 271 | 71.2 | 23.6 | 5.2 | – | – |
| Johanet (France)16 | 2002 | 100 | 83 | 17 | 0 | 4 | – |
| Lau (USA)17 | 2002 | 888 | 96.8 | 3.2 | – | – | – |
| Bal (India)18 | 2003 | 313 | 92.6 | 0.9 | 6.2 | 2.5 | 0.6 |
| Leeder (United Kingdom)19 | 2004 | 154 | 85.7 | 14.3 | 0 | 1.9 | – |
| Bermúdez (Spain)20 | 2004 | 115 | 70.4 | 8.7 | 20.9 | 0.9 | 0.9 |
| Bueno Lledó (Spain)21 | 2006 | 504 | 88.9 | 10.1 | 1 | 2.2 | 0.7 |
| Proske (France)22 | 2007 | 211 | 82 | 18 | 0 | – | – |
| Victorzon (Finland)23 | 2007 | 567 | 63 | 37 | 0 | 2 | 0 |
| Vanderbroucke (Canada)24 | 2007 | 151 | 81 | 19 | 0 | 2 | 0 |
| Lezana Pérez (Spain)25 | 2013 | 141 | 81.6 | 8.5 | 9.2 | 3.5 | 1.4 |
| Planells Roig (Spain)26 | 2013 | 1601 | 82 | 13.4 | 2.3 | 2.1 | 0 |
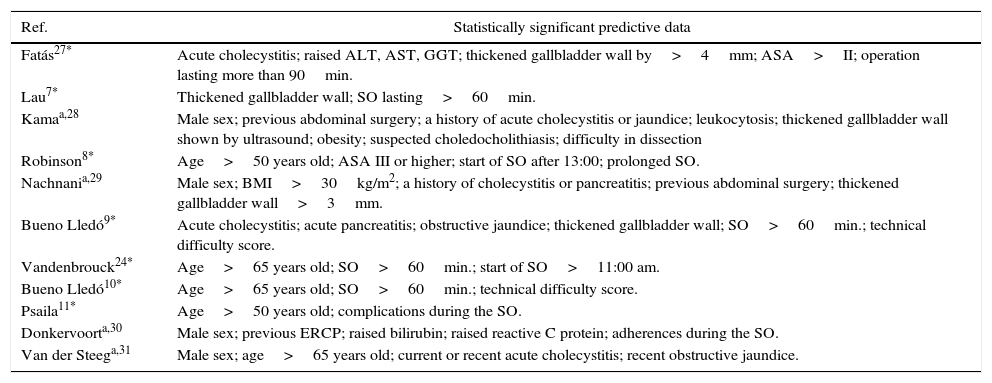
After more than 2 decades of experience with AS-LC and many publications13–26 (Table 4) and (Table 5).7–11,24,27–31 as well as meta-analysis,32,33 the safety of this technique now seems to have been clearly proven. Nevertheless, the rate of unplanned or undesired admissions or, as we term them, “AS failures”, is high.
Predictive Factors for AS Failure or Conversion in a Range of Studies.
| Ref. | Statistically significant predictive data |
|---|---|
| Fatás27* | Acute cholecystitis; raised ALT, AST, GGT; thickened gallbladder wall by>4mm; ASA>II; operation lasting more than 90min. |
| Lau7* | Thickened gallbladder wall; SO lasting>60min. |
| Kamaa,28 | Male sex; previous abdominal surgery; a history of acute cholecystitis or jaundice; leukocytosis; thickened gallbladder wall shown by ultrasound; obesity; suspected choledocholithiasis; difficulty in dissection |
| Robinson8* | Age>50 years old; ASA III or higher; start of SO after 13:00; prolonged SO. |
| Nachnania,29 | Male sex; BMI>30kg/m2; a history of cholecystitis or pancreatitis; previous abdominal surgery; thickened gallbladder wall>3mm. |
| Bueno Lledó9* | Acute cholecystitis; acute pancreatitis; obstructive jaundice; thickened gallbladder wall; SO>60min.; technical difficulty score. |
| Vandenbrouck24* | Age>65 years old; SO>60min.; start of SO>11:00 am. |
| Bueno Lledó10* | Age>65 years old; SO>60min.; technical difficulty score. |
| Psaila11* | Age>50 years old; complications during the SO. |
| Donkervoorta,30 | Male sex; previous ERCP; raised bilirubin; raised reactive C protein; adherences during the SO. |
| Van der Steega,31 | Male sex; age>65 years old; current or recent acute cholecystitis; recent obstructive jaundice. |
* Study purpose: factors associated with AS failure.
The main aim of AS-CC is that the patient, once operated, is able to return home with appropriate levels of well-being and clinical safety after a short observation period in the hospital (less than 12h) without remaining there for even a single night. In the published series this aim is achieved in a percentage of cases that varies from 63% to 96%13–26 (Table 4), while a rate of 80% is the most usual. The actual rate of AS in the largest series published in Spain (Planells)26 is 80.8%.
The variation in these results has been attributed to the inclusion criteria for this procedure.34 Some studies aimed to discover predictive factors for unplanned admission following AS-CC7–11,24,27 or predictors for conversion to laparotomy28–31 (Table 5). These works found a series of variables which are associated with “AS failure”: (1) demographic data: male sex28–31 and advanced age with different cut-off points (>50 years old,8,11 >65 years old,10,24 etc.); (2) clinical data: obesity measured by the BMI,29 raised transaminase levels,27 thickening of the gallbladder wall shown by ultrasound,7,27–29 previous ERCP,30 a previous episode of cholecystitis, pancreatitis or jaundice9,28,31; (3) associated pathology: in general summarised in the anaesthetic risk, ASA8; (4) SO data: difficulty of dissection, duration of the SO,8,24,29 and the time of the planned operation.8,24
We have been using AS-CC in our hospital since 1999. Our experience with AS-CC was published in the ASEAS journal in 2010.12 In the majority of series from 15% to 25% of cases are admitted for at least one night (Table 4). Our results are even worse, with 30% of “AS failures”. As our inclusion criteria are not very strict and are also similar to those used for other less important AS procedures, we believe that our series could be used to detect which variables are associated with admission to hospital and therefore improve the indication criteria.
In our series we studied the different variables proposed by these authors (Table 5). Bivariate analysis (Table 3) shows that there is a statistically significant association between age, ASA risk, gallbladder wall thickness as detected by ultrasound, previous admission due to cholecystitis and the duration of the SO. However, the variables of male sex, BMI higher than 30, previous supramesocolic surgery, previous ERCP and previous admission for pancreatitis are not associated with the risk of admission (Table 3). The above-mentioned studies are observational, so that confusion factors may exist that would have to be controlled by multivariate analysis. The studies that do this show a small number of independent variables: age, a history of cholecystitis and, invariably, the duration of the SO or complications during the operation.7,10,11 Nevertheless, these results are not useful in practice as AS must be indicated beforehand, and in many cases technical difficulties in the SO cannot be predicted. Planells,35 investigating the same subject, shows that an index composed of clinical and radiological data, age and data on associated disease which he denominates the “surgical complexity classification index (SCCI)” correlates well with the technical difficulty of the SO and its duration, so that it could be used to improve the indication for AS-LC. The usefulness of said index in practice has yet to be proven.
By applying logistic regression for the purpose of prediction, i.e., selecting the model that shows the highest capacity for correct classification, we obtain the following independent predictive variables: ASA risk, age over 65 years old and previous admission for cholecystitis. We select the cut-off point of 65 years old for age to keep a balance between the risk of admission and the exclusion of a large number of patients. However, the predictive capacity of this model is very low. It R2 determination index is only 0.05–0.06, indicating that more than 90% of the variability observed in the series is not explained by the model. Although it has a high specificity (98.6%) its sensitivity is practically zero, so that it lacks practical predictive value. If we decide to exclude all of the patients with a history of cholecystitis, and considering that its prevalence in our population of cases indicated for AS stands at 10%, this measure would improve results by 7.7% (the attributable fraction of the population) (Table 3). Nevertheless, it must be considered that half of our patients with a history of cholecystitis were discharged on the same day, so that if they were excluded they would cease to benefit from AS. We therefore believe that restricting the indications for AS-LC should take into account the capacity of the hospital to admit patients unplanned, and therefore, the particular situation of each surgical department. It should not be forgotten that in the majority of AS-LC series, from 15% to 25% of patients are admitted for at least one night (Table 4).
As our results show, data other than the indication for surgery determine the results, and these must be the cause of the unexplained variability in the regression model. Ahn36 in an excellent revision evaluates all of the factors that could be adjusted to achieve better results when performing LC as AS and which could be applied clinically.
To conclude, we believe that LC can safely be performed in an AS regime with the same indication criteria as any cholecystectomy while fulfilling the basic general criteria for any AS-SO, although we have to be ready to accept a high percentage of unplanned admissions. An improvement in results has to be sought not so much in restricting indications as in multidisciplinary perioperative care with a fast-track protocol.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Soler-Dorda G, San Emeterio Gonzalez E, Martón Bedia P. Factores asociados a ingreso no previsto tras colecistectomía laparoscópica en régimen de cirugía mayor ambulatoria. Cir Esp. 2016;94:93–99.