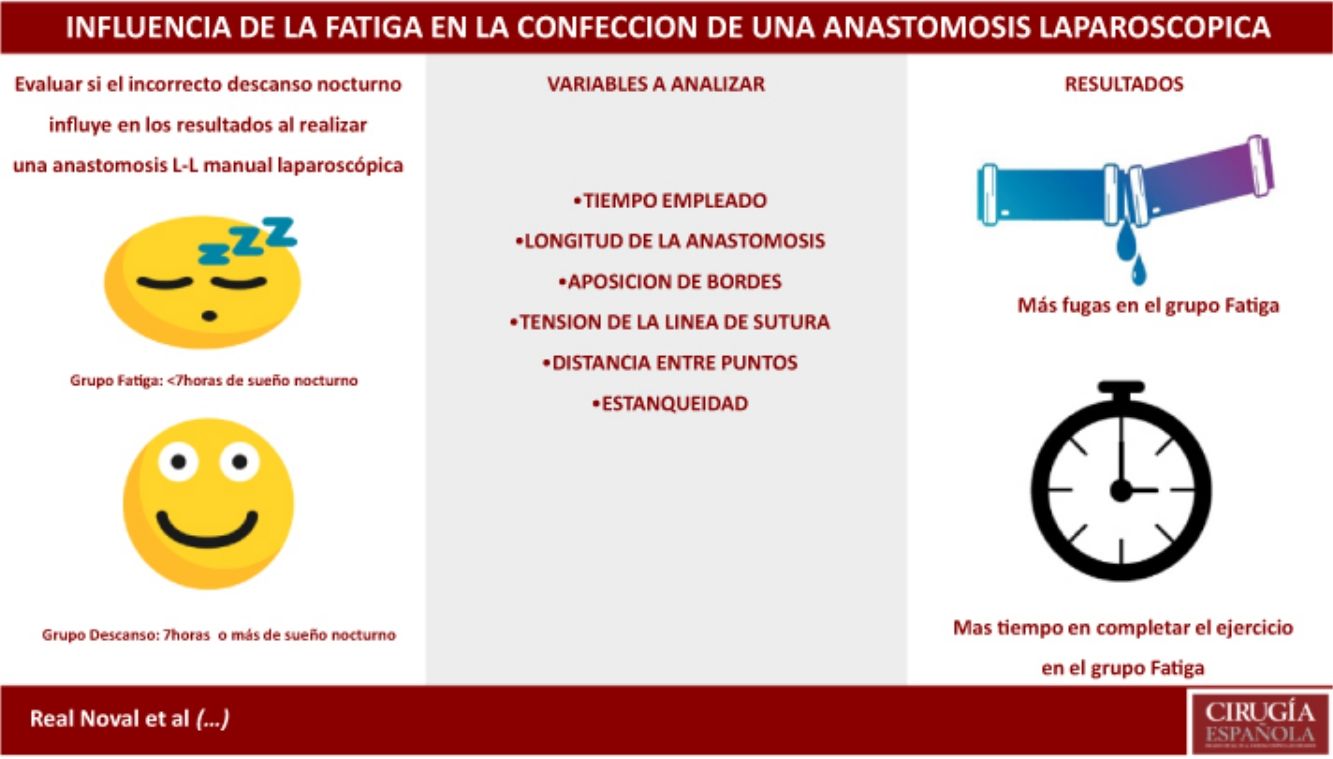
To assess the impact of fatigue due to incorrect night rest in the performance of a laparoscopic manual anastomosis.
MethodsA prospective study evaluating the results from the realization of a manual endotrainer entero-enteral anastomosis performed by residents in terms of fatigue caused by inadequate nightly rest. Two groups were established; the FATIGUE group (F): anastomosis performed by residents coming off shift who slept less than seven hours and the REST group(R), being those who slept at home for more than 7 h. The time taken, length of the anastomosis and quality of such were compared based on 4 parameters: Air leak test, correct tension on the suture line, accurate opposition of the edges and optimal distance between stitches.
Results402 anastomoses were studied (211 rest group, 191 fatigue group). In the fatigue group leaks were detected in 33.5% anastomoses, as opposed to 19.4% in the rest group (P < .01). El rest group performed the anastomosis in 56.75 min and the fatigue group in 61,49 min (P = .006). There were no significant differences in the others parameters.
ConclusionsFatigue increases the risk of leakage and the time to do the exercise.
Evaluar el impacto de la fatiga por incorrecto descanso nocturno en la realización de una anastomosis manual laparoscópica.
MétodosSe lleva a cabo un estudio prospectivo observacional evaluando la realización de una anastomosis manual enteroenteral en endotrainer por residentes. Se dividen en dos grupos; el grupo descanso incluye a residentes que han dormido en casa 7 o más horas frente al grupo fatiga formado por residentes de guardia o que han dormido menos de 7 horas. Se evalúa el tiempo empleado, la longitud de la anastomosis, la correcta tensión de la línea de sutura, la correcta aposición de los bordes, la distancia entre puntos y la fuga de aire en prueba neumática de estanqueidad.
ResultadosSe evalúan 402 anastomosis, siendo 211 pertenecientes al grupo descanso y 191 al grupo fatiga. Se detecta fuga en el 33,5% de las anastomosis del grupo fatiga frente al 19,% en el grupo descanso (p < 0,01). El tiempo empleado en el grupo descanso es de 56,75 min. frente a 61,49 en el grupo fatiga (p = 0,006). No hay diferencias en el resto de parámetros.
DiscusiónLa fatiga aumenta el riesgo de fuga y el tiempo que se tarda en completar el ejercicio.
In Spain, current legislation states that, after being on duty for 17–24 h, residents should be given at least 12 h off1. The training period for general surgery residents is 5 years, and sometimes the current Royal Decree is not always respected in order to maximize resident training. This leads to 24-h shifts, with little night rest, followed by activity the next morning. After evaluating 89 residents for one year, a moderate risk of fatigue and sleep deficit was observed2. The inherent fatigue of a poor night’s rest can affect a resident’s abilities and have an effect similar to having blood alcohol concentrations of 0.04%–0.05%3. Landrigan et al. detected 36% more serious errors and 5.6 times more diagnostic errors when they compared one group with a working day of 24 h or longer versus a group with shorter work hours in an intensive care unit4. In studies conducted with laparoscopy simulators, the group with little night rest made 20% more errors when performing the exercises and spent 14% more time performing them5. In residents, fatigue due to poor night’s sleep has also been identified as a cause of a greater number of percutaneous accidents (scalpel cuts, needle sticks), more traffic accidents in transit, and a greater risk of falling asleep at the wheel6,7.
However, Ellman et al. reviewed 6700 operations performed by cardiac surgeons and found no differences in morbidity and mortality when comparing patients operated on by surgeons with little sleep versus surgeons with proper rest8. Similar studies show that insufficient nighttime rest does not increase complications in operations carried out by residents or their simulator results9–11.
Since 2003, surgery residents in Cantabria have completed a training program in technical, cognitive and behavioral skills as part of the residency curriculum. The program takes place at the Valdecilla Virtual Hospital (VVH). A fundamental exercise is performing a correct laparoscopic intestinal anastomosis, which is an exercise that requires a high degree of concentration, skill and meticulous use of the instruments. Mastery of the technique requires a significant number of training hours12. The objective of this study is to evaluate whether residents with inadequate nighttime rest obtain worse results when performing a laparoscopic intestinal anastomosis.
MethodsParticipantsWe have carried out a prospective observational study within the VVH setting after recruiting 25 residents associated with the Marqués del Valdecilla University Hospital (Santander) and the Sierrallana Hospital (Torrelavega). Participants were selected through a non-probabilistic sampling of consecutive cases. We selected available residents from the Hospital Valdecilla and Hospital Sierrallana who had either completed or were completing the VVH training program. Therefore, there was no sample size calculation.
The participants signed a voluntary consent form, and the study was approved by the VVH Ethics Committee. The participants were divided into two groups: the rest group (Group D), which included residents who had slept at home for at least 7 h; and the fatigue group (Group F), which included residents who had slept for less than 7 h at home or while on call at the hospital. Seven hours is the minimum rest time recommended by the National Sleep Foundation13. To avoid the effects of the learning curve, we recruited residents who had completed at least one year training, thereby guaranteeing that the residents had repeated the exercise a number of times during the first year of residency12. In addition, each resident behaved as both a case and as a control, performing alternate anastomoses: some days after optimal rest and other days while sleep deprived.
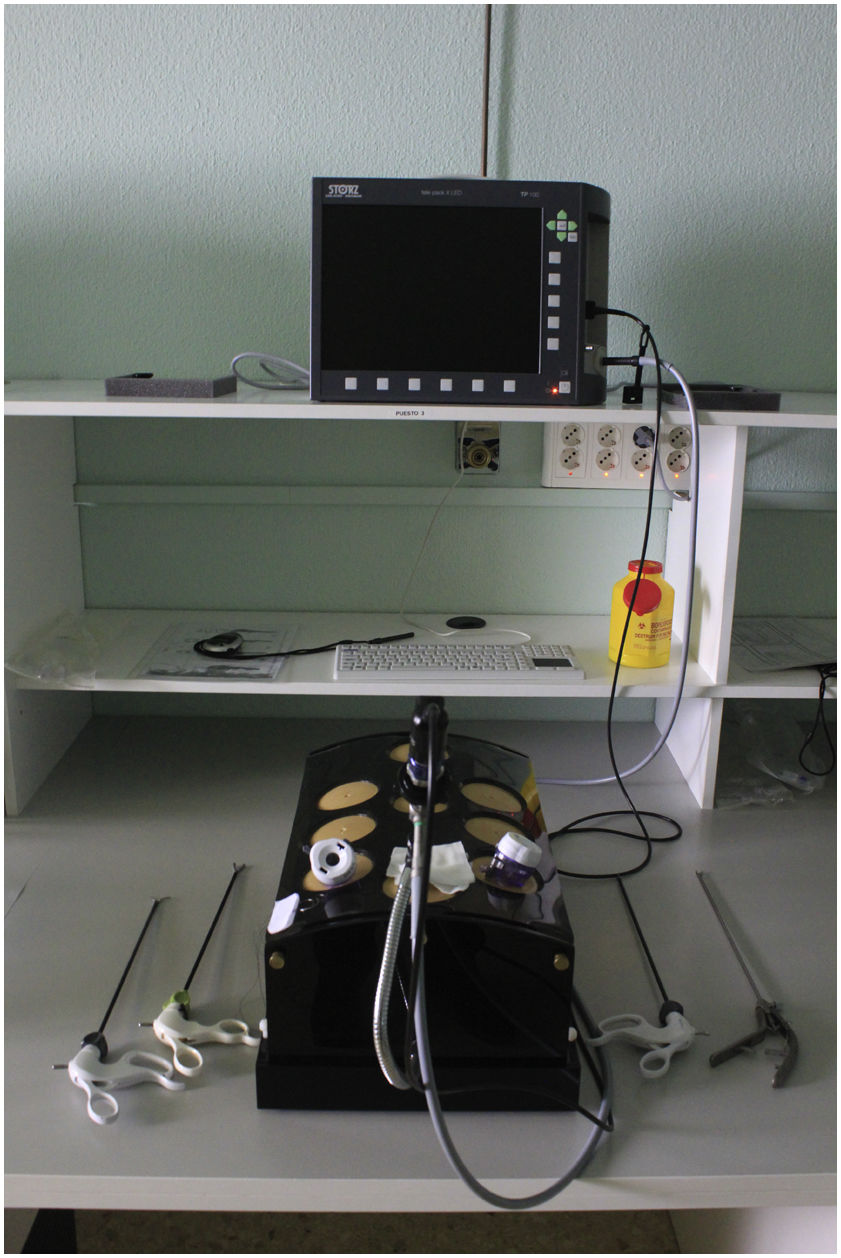
MaterialThe anastomoses were performed on ex vivo cryopreserved pig intestine. An endotrainer and 0° optics were used. The material used consisted of a dissector, needle holder, scissors, and grasping forceps. The suture material used was 3/0 silk for the interrupted stitches on the posterior side and 3/0 absorbable monofilament suture for the anastomosis (Fig. 1).
ExerciseA side-to-side laparoscopic anastomosis was performed, consisting of five seroserous fixation sutures on the posterior side, followed by an anastomosis in two continuous hemicircumferences (Fig. 2). The exercise was supervised by an assistant with proven experience in laparoscopic surgery, who gave no instructions to the resident and merely evaluated the activity.
The items that were assessed in the anastomosis were agreed upon by experts, according to a Delphi method, as previously published14–16.
- 1
Length of the anastomosis: a quantitative variable representing the distance between the 2 angles measured with a caliper, the objective result being an anastomosis of 50 mm.
- 2
Correct apposition of the tissue edges, measured directly by the observer: a dichotomous variable that takes as values the correct or the incorrect apposition of the edges. It is considered correct if the edges are not overlapping.
- 3
Correct suture line tension: measured by the observer by inserting the tip of a mosquito forceps to check for loose stitches. It is a dichotomous variable with two tension levels: correct or incorrect.
- 4
Distance between stitches: a dichotomous variable; the correct distance between stitches is 2.5–3.5 mm.
- 5
The anastomosis is tested for leaks using pneumatic pressure and a manometer. This is a dichotomous variable consisting of the existence of a leak when filling the anastomosis with water or not.
In addition, the following is recorded:
- 1
Number of hours of sleep of the resident. Continuous quantitative variable.
- 2
Time used to create the anastomosis, expressed in minutes. Continuous quantitative variable.
The analysis is carried out with the SPSS 15 software package for Windows (SPSS Inc, Chicago, IL, USA). Quantitative variables are expressed as mean and standard deviation, compared with the Mann-Whitney U test for non-normal distribution. Qualitative variables are expressed as a percentage and compared with the chi-squared or Fisher’s test. The variables that are significant in the univariate analysis are then input into a logistic regression-type multivariate analysis in order to control possible confounding variables. A P value <.05 is considered significant.
ResultsTwenty-five residents participated in the study: 10 men (40%), and 15 women (60%). In total, 402 anastomoses were evaluated: 211 (52.5%) completed by the well-rested group and 191 (47.5%) by the fatigue group.
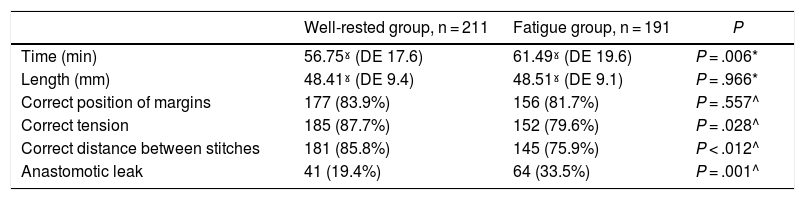
The fatigue group slept an average of 5.13 h (SD 1.1 h) versus a mean of 7.07 h (SD 0.3 h) in the rest group, which was statistically significant (P < .001). The fatigue group used an average of 61.49 (SD 19.6) minutes for completion of the exercise versus the 56.75 (SD 17.6) minutes used by the rest group. This result is statistically significant with a P value of .006. In contrast, there were no statistically significant differences in the length of the anastomosis.
The rest group obtained better results that were statistically significant for the correct tension of the suture line, the correct distance between stitches, and the leak test. In contrast, there were no statistically significant differences in the correct apposition of the edges between the 2 groups (Table 1).
Univariate comparison between the two groups.
| Well-rested group, n = 211 | Fatigue group, n = 191 | P | |
|---|---|---|---|
| Time (min) | 56.75ˠ (DE 17.6) | 61.49ˠ (DE 19.6) | P = .006* |
| Length (mm) | 48.41ˠ (DE 9.4) | 48.51ˠ (DE 9.1) | P = .966* |
| Correct position of margins | 177 (83.9%) | 156 (81.7%) | P = .557^ |
| Correct tension | 185 (87.7%) | 152 (79.6%) | P = .028^ |
| Correct distance between stitches | 181 (85.8%) | 145 (75.9%) | P < .012^ |
| Anastomotic leak | 41 (19.4%) | 64 (33.5%) | P = .001^ |
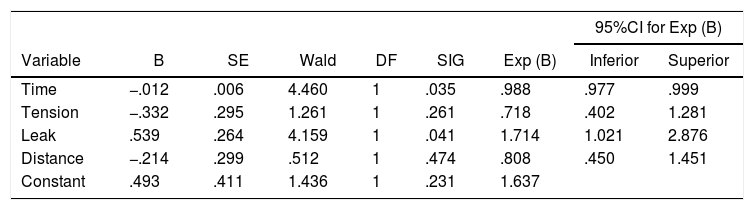
The logistic regression analysis showed that only the execution time variable (P = .035) and the experimental anastomotic leak variable (P = .041) were statistically significant (Table 2).
Variables of the logistic regression equation.
| 95%CI for Exp (B) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | Wald | DF | SIG | Exp (B) | Inferior | Superior |
| Time | −.012 | .006 | 4.460 | 1 | .035 | .988 | .977 | .999 |
| Tension | −.332 | .295 | 1.261 | 1 | .261 | .718 | .402 | 1.281 |
| Leak | .539 | .264 | 4.159 | 1 | .041 | 1.714 | 1.021 | 2.876 |
| Distance | −.214 | .299 | .512 | 1 | .474 | .808 | .450 | 1.451 |
| Constant | .493 | .411 | 1.436 | 1 | .231 | 1.637 | ||
B: variable coefficient; SE: standard error; Wald: Wald test; DF: degrees of freedom; SIG: P value of the Wald test; Exp (B): exponential coefficient of the variable; 95%CI: 95% confidence interval for Exp (B).
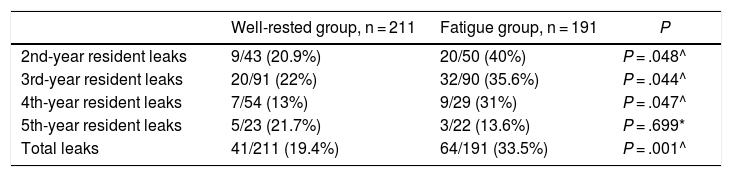
In terms of the year of residency, residents in their 2nd, 3rd and 4th years had more leaks in the fatigue group, which was a statistically significant result. In contrast, there were no differences observed in 5th-year residents (Table 3).
Results of the anastomotic leak variable depending on the years of residency.
| Well-rested group, n = 211 | Fatigue group, n = 191 | P | |
|---|---|---|---|
| 2nd-year resident leaks | 9/43 (20.9%) | 20/50 (40%) | P = .048^ |
| 3rd-year resident leaks | 20/91 (22%) | 32/90 (35.6%) | P = .044^ |
| 4th-year resident leaks | 7/54 (13%) | 9/29 (31%) | P = .047^ |
| 5th-year resident leaks | 5/23 (21.7%) | 3/22 (13.6%) | P = .699* |
| Total leaks | 41/211 (19.4%) | 64/191 (33.5%) | P = .001^ |
The study design aims to assess the impact of fatigue during the execution of a complex psychomotor and cognitive activity. In this case, the fatigue caused by inadequate sleep at night leads to a greater number of experimental anastomotic leaks and a more time spent for completion.
There is controversy among the published studies regarding whether proper or inadequate nighttime rest worsens the results obtained during simulation. Some studies have not found significant differences between the groups with adequate rest versus the groups without adequate rest10,17–22. Robinson et al. did not find significant differences in the acquisition of skills between the fatigue group and the rest group using a DaVinci model surgical robot23. In contrast, other studies obtain worse results in the fatigue group versus the well-rested group in the execution of the exercises5,24–28.
The simulators used in these studies are both virtual and physical, and the exercises that are evaluated methodologically are heterogeneous and differ in complexity. This fact could explain the discrepancies in the results. In our opinion, some articles assess exercises that are too simple, such as changing a nut from one bolt to another, applying an endoloop, or simple cutting exercises. These exercises are not comparable with a complete surgical procedure as they are exercises that can be performed in a few minutes. By comparison, manual laparoscopic anastomosis is a more complex psychomotor procedure that requires greater concentration, motivation, and mental and physical effort. In addition, it requires greater laparoscopic skills.
Insufficient rest may not be relevant when performing simple laparoscopic exercises that are short in duration and mere psychomotor exercises, but its deleterious effect becomes evident when practicing complex exercises that require mental activity and concentration over a long period of time. This idea is supported by various articles that speak of a greater resistance to fatigue of psychomotor activities versus activities that require intense cognitive activity29–31.
In our study, the well-rested group performed the exercise in a shorter time. This result is consistent with other studies, in which the fatigue group takes longer to perform tasks5,26,28. In one case, Brandenberger et al. reported a shorter time in the execution of the exercise in the fatigue group versus the rested group. They justify this with the thinking that the participants were more tolerant to errors in order to finish as soon as possible and go home to rest25.
Tsafrir reports a greater deleterious effect in new residents26. In our group of participants, there were worse results in 2nd to 4th-year residents, but not in 5th-year residents. Year 5 residents performed fewer anastomoses than the other groups, which may paradoxically contribute to more fatigue in the rest group, although without reaching statistical significance. The lower number of anastomoses is due to the fact that this group of residents spend more time performing in vivo animal laparoscopic techniques.
We feel that one advantage of our study is that it compares the effect of fatigue on a complex and complete surgical procedure versus the execution of simple individual exercises, with no common purpose or relationship. It is true that the use of cryopreserved porcine viscera does not faithfully represent the structure of the human intestine, it does not bleed, and intestinal material is not spilled into the cavity, which is why we speak of an experimental anastomotic leak, not a clinical anastomotic leak. But it is also true that it allows us to assess factors that other exercises cannot assess, such as suture tension, care in tissue handling, or the presence of anastomotic leak. We believe that simulating a complex process that is carried out regularly in operating rooms can give us a better idea of the impact of fatigue on surgical activity and provide us more valid results. We feel that another strong point of the study is that it was conducted in a virtual laboratory. Thus, fatigue was evaluated in a safe environment, which minimizes the risks for the residents while also eliminating risk for patients because at no time was there any contact between the resident and patients. In this way, by avoiding the action of a fatigued resident on a patient, errors are avoided (which lead to 100 000 deaths/year in the US), and ethical conflicts derived from the patient-resident interaction are avoided32,33.
Our study has limitations. First of all, the number of participants is low, as only 25 residents were recruited. We have attempted to resolve this inconvenience by having each resident do the exercise several times. To limit the learning effect, we selected residents who had already performed the exercise a sufficient number of times and were considered competent in performing it12. In addition, each participant has alternated between the fatigue group and the rest group, in such a way that anastomoses created after a proper night’s rest alternated with anastomoses made after a poor night’s rest. Each participant thus acted as case and control, performing a similar number of anastomoses in each of the two groups.
The second limitation of the study is that the number of hours of sleep was self-reported by the participants. Also, the number of hours slept is given, but the quality of that sleep was not evaluated. In addition, chronic sleep deprivation in the days prior to exercise was not taken into account.
The third limitation is an inherent characteristic of the virtual experimental laboratory. The exercise does not represent 100% of the operating room reality. As mentioned before, cryopreserved viscera do not bleed, there is less stress knowing that it is not a patient, etc. On the other hand, the virtual laboratory is currently the situation that most closely imitates clinical practice, without actually going into an operating room.
The fourth limitation of the study is that we did not assess the impact that the use of substances such as caffeine or other stimulating drinks may have on the results.
ConclusionsIn our study, fatigue caused by inadequate nighttime rest is responsible for a greater number of anastomotic leaks and a greater time spent performing the exercise.
It is necessary to evaluate how fatigue affects residents’ health and wellbeing in order to avoid fatigue-related errors. In addition, it is necessary to reconcile the need to acquire a wide range of skills in a limited amount of time, while also recognizing the need for optimal rest. For all these reasons, more studies are required to understand and evaluate the possible deleterious effects that fatigue and lack of sleep have on clinical and surgical practice.
FundingThis study has received no funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Real Noval H, Martin Parra JI, Fernández Fernández J, del Castillo Criado Á, Ruiz Gómez JL, López Useros A, et al. Fatiga por deprivación de sueño en residentes de cirugía: ¿Afecta a los resultados al realizar una anastomosis laparoscópica intestinal? Cir Esp. 2022;100:223–229.