Videolaryngoscopy has mainly been developed to facilitate difficult airway intubation. However, there is a lack of studies demonstrating this method's efficacy in pediatric patients. The aim of the present study was to compare the TruView infant EVO2 and the C-MAC videolaryngoscope with conventional direct Macintosh laryngoscopy in children with a bodyweight ≤10 kg in terms of intubation conditions and the time to intubation.
METHODS:In total, 65 children with a bodyweight ≤10 kg (0-22 months) who had undergone elective surgery requiring endotracheal intubation were retrospectively analyzed. Our database was screened for intubations with the TruView infant EVO2, the C-MAC videolaryngoscope, and conventional direct Macintosh laryngoscopy. The intubation conditions, the time to intubation, and the oxygen saturation before and after intubation were monitored, and demographic data were recorded. Only children with a bodyweight ≤10 kg were included in the analysis.
RESULTS:A total of 23 children were intubated using the C-MAC videolaryngoscope, and 22 children were intubated using the TruView EVO2. Additionally, 20 children were intubated using a standard Macintosh blade. The time required for tracheal intubation was significantly longer using the TruView EVO2 (52 sec vs. 28 sec for C-MAC vs. 26 sec for direct LG). However, no significant difference in oxygen saturation was found after intubation.
CONCLUSION:All devices allowed excellent visualization of the vocal cords, but the time to intubation was prolonged when the TruView EVO2 was used. The absence of a decline in oxygen saturation may be due to apneic oxygenation via the TruView scope and may provide a margin of safety. In sum, the use of the TruView by a well-trained anesthetist may be an alternative for difficult airway management in pediatric patients.
Direct laryngoscopy can be challenging in small children. Failure to successfully intubate the trachea and to secure a patient's airway remains a leading cause of morbidity and mortality in the operative setting (1). In children, adverse respiratory effects are responsible for the largest proportion of perioperative critical events (2).
The airway of infants is special, differing significantly from that of older children. Anatomic differences include a large head that tends to flex the short neck and obstruct the airway, a large tongue, a short jaw, a long palate, a long epiglottis, a more cephalad-located larynx, and a soft airway that may lead to airway obstruction (3).
Despite the development of numerous pediatric airway management tools and techniques, “classic” endotracheal intubation remains the gold standard in securing the airway (4). However, in the last several years, there has been intensive development of tools for the management of difficult pediatric airways. Several studies have shown that videolaryngoscopy provides a better laryngeal view than does direct laryngoscopy in adult patients or mannequins with either apparently normal or potentially difficult airways (5-10). Most of the published data related to videolaryngoscopy have been obtained from adults, as the implementation of videolaryngoscopy in pediatric airways has only been investigated in a few recent publications (11-14). Therefore, videolaryngoscopy in children is a developing area of research, and several different tools for indirect laryngoscopy are available today.
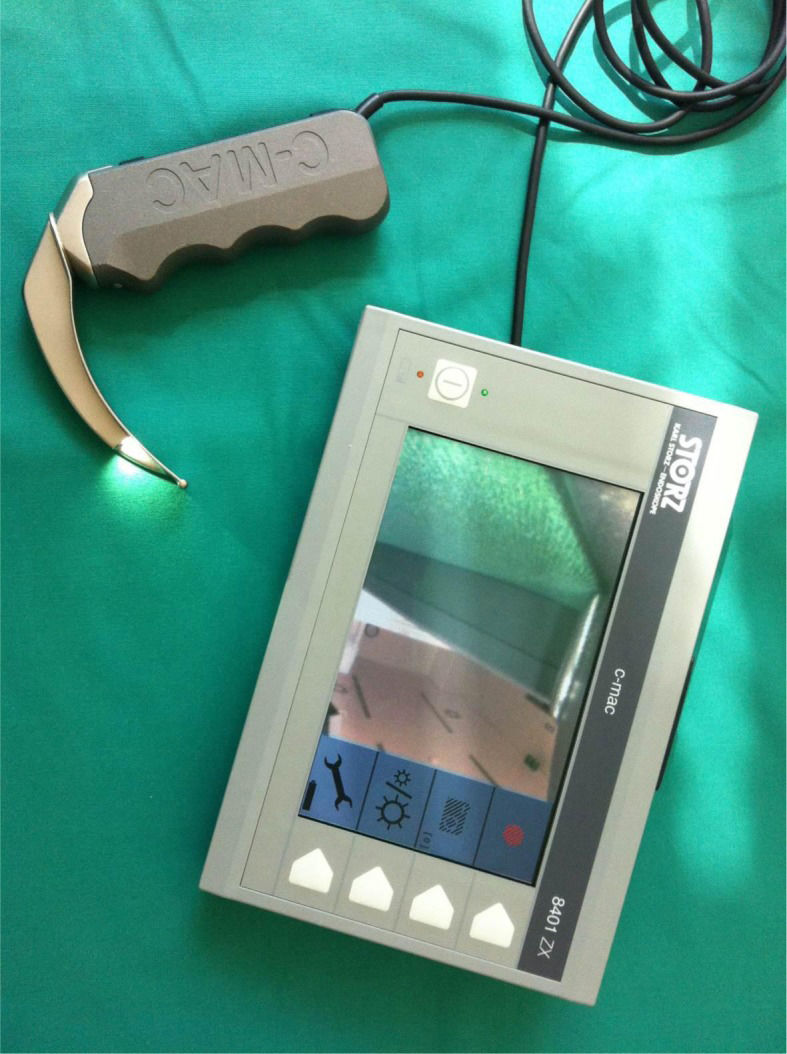
The C-MAC videolaryngoscope system (Karl Storz GmbH & Co. KG, Tuttlingen, Germany; Figure1) is a novel device that can be used with special Macintosh laryngoscope blades of different sizes (2,3,4) and a difficult-airway blade (D-Blade) (15,16). A camera providing an 80° angle of view and a light source are recessed from the tip of the blade. The electronic unit sits in a handle attached to the laryngoscope blade and is connected by a wire to a portable TFT video monitor. The system allows for the Macintosh laryngoscope blade to be used for direct and indirect laryngoscopy and for the D-Blade to be used for only indirect laryngoscopy. The low profile of the original British Macintosh blades may prove advantageous, especially when the mouth opening is limited.
In 2006, the Truphatek TruView EVO2 system (Truphatek International Limited, Netanya, Israel) was introduced for adult airway management (17), and in 2009, the device began to be used in pediatric anesthesia (18). The TruView system is a device with an integrated optical lens system and a unique blade tip angulation that provides an optimal line of sight, allowing a view of the glottis via the prismatic lens without having to align the oral, pharyngeal, and tracheal axes (Figure2). The blade of the laryngoscope has a magnified optic side port that provides a wide, magnified laryngeal view at a 46° anterior refracted angle. The tool has a narrower blade tip than does the Macintosh blade and an integrated oxygen jet-cleaning system (flow 2-5 l/min-1) to prevent fogging and provide apneic oxygenation. In its commercial version, a portable TFT monitor can be attached. An infant blade is also available and is recommended for use in children with a bodyweight of 1-10 kg. To provide the correct angulation and rigidity in the endotracheal tube, a special stylet (the OptiShapeTM) comes with the TruView.
This study was designed to compare intubation conditions using the TruView EVO2, the smallest available C-MAC videolaryngoscope (blade size 2), and standard direct laryngoscopy with a Macintosh blade in children with a bodyweight ≤10 kg. In contrast to the wide use of the Miller blade in this subset of patients, at our institution, the Macintosh blade is the standard blade for primary intubation, even in infants. Here, the study endpoints were the time to intubation (TTI) and visualization of the glottic structures.
MATERIALS AND METHODSApproval for this retrospective observational study was obtained from the local ethics committee of the Medical Faculty of Goethe University Frankfurt. The C-MAC and the TruView EVO2 devices are integral parts of the airway management process at our institution and are regularly used for airway management in children. For quality-control reasons, we collect data on intubation conditions and the handling of each device after introduction into a new environment. In this study, children were considered appropriate for recruitment if they were from 1-10 kg in weight and had undergone elective surgery with planned endotracheal intubation. The exclusion criteria included the presence of a high risk of pulmonary aspiration, the presence of any pathology of the head or neck, hemodynamic instability, and emergency surgery. The included children were retrospectively analyzed over a period of 4 months. The laryngoscopists were board certified and experienced in standard direct laryngoscopy and indirect laryngoscopy with the C-MAC device. Prior to clinical utilization of the TruView EVO2 device, the physicians performed 10 mannequin intubations and three human intubations with the device, before any data collection was started.
In the operating theater, all children were monitored using electrocardiograms, noninvasive arterial blood pressure measurements, pulse oximetry, capnography, and inspired oxygen concentration measurements. Additionally, all children underwent inhalational induction with sevoflurane. Prior to laryngoscopy, the lungs were ventilated with 4-8% sevoflurane in oxygen. A neuromuscular relaxant (mivacurium 0.2 mg kg-1) was administered routinely. When the anesthesia depth and neuromuscular blockade were deemed suitable for intubation, laryngoscopy was performed. All intubations were performed with a styletted endotracheal tube without a cuff. In the TruView EVO2 group, a special stylet, the OptiShapeTM, was used. Based on prior experience in the use of the C-MAC videolaryngoscope, angulation of the ETT in this group was 60-70° at the tip to achieve a better guidance toward the glottis.
The primary outcome parameter in this study was the TTI, defined as the time from the end of preoxygenation (mask taken from the face) to the first detection of endtidal CO2. Timing was determined by a member of the research team using a stopwatch (Finanzplatzuhr, Sinn, Frankfurt am Main, Germany). The laryngeal view was also graded according to the Cormack-Lehane (CL) score (19). Furthermore, the lowest peripheral oxygen saturation (LpO2) during intubation was noted. After intubation, the ease of intubation with the respective device was recorded using a 10 cm visual analog scale (VAS), with 0 being extremely difficult and 10 being easy and comfortable.
StatisticsAn analysis of the data confirmed that a Gaussian distribution was not present. All data were summarized using the median and range. The statistical analysis was performed using a software package (GraphPad InStat Version 3.06; GraphPad Software Inc., San Diego, CA). The data were analyzed with the nonparametric Kruskal-Wallis one-way analysis of variance (ANOVA) test, and a post-hoc analysis was performed using Dunn's multiple comparison test. Statistical significance was assumed with a probability of type I error of less than 5% (p<0.05).
RESULTSA total of 65 children with normal airways were retrospectively included over a period of 4 months: 23 children in the C-MAC group (C-MAC), 22 children in the TruView EVO2 group (TruView), and 20 children in the Macintosh blade group (Macintosh). The children in all groups were similar in terms of age, but there were statistically significant differences between the groups in the mean weights and heights. The patient characteristics are summarized in Table1.
Patient characteristics. The data are presented as the median and range.
| C-MAC (n = 23) | TruView (n = 22) | Macintosh (n = 20) | p-value | |
|---|---|---|---|---|
| Age (months) | 9.0 (1-22)* | 4.0 (0-21) | 7.5 (0-20) | *p<0.05 vs. TruView EVO2 |
| Weight (kg) | 8.6 (2.7-10)* | 5.2 (2.7-10) | 7.5 (2.5-10) | *p<0.05 vs. TruView EVO2 |
| Height (cm) | 70 (50-85)* | 60 (50-80) | 66.5 (50-95) | *p<0.05 vs. TruView EVO2 |
The time required for tracheal intubation was significantly longer in the TruView group (52 sec [20-102 sec]) than in the C-MAC (28 sec [8-93 sec]) and Macintosh (26 sec [18-95 sec]) groups (Table2). In most children, the devices produced excellent visualization of the vocal cords. Only one child in the C-MAC group and another in the Macintosh group were graded as CL III. The lowest peripheral oxygen saturation values during the intubation attempt were 94% in the C-MAC group, 86% in the TruView group, and 93% in the Macintosh group. Additionally, the ease of use, as analyzed by a VAS, was 9 (8-10) in the C-MAC group, 8 (6-10) in the TruView group, and 10 (0-10) in the Macintosh group.
Detailed outcome data for all devices. The data are presented as the median and range.
| C-MAC (n = 23) | TruView (n = 22) | Macintosh (n = 20) | p-value | |
|---|---|---|---|---|
| CL I | 19 | 21 | 17 | n.s. |
| CL II | 3 | 1 | 2 | n.s. |
| CL III | 1 | - | 1 | n.s. |
| CL IV | - | - | - | n.s. |
| TTI (sec) | 28 (8-93) | 52* (20-102) | 26 (18-95) | *p<0.05 vs. C-MAC and Macintosh |
| LpO2 (%) | 99 (94-100) | 100 (86-100) | 100 (93-100) | n.s. |
| VAS (cm) | 9 (8-10) | 8* (6-10) | 9 (0-10) | *p<0.05 vs. C-MAC and Macintosh |
CL = Cormack & Lehane grade; TTI = Time to intubation; LpO2 = Lowest peripheral oxygen saturation; VAS = Visual analog scale.
No complications directly related to the intubation attempt, no dental injuries, and no airway injuries were observed in any of the groups.
DISCUSSIONWe aimed to compare the effectiveness of two different videolaryngoscopes, the C-MAC videolaryngoscope and the TruView EVO2 laryngoscope, with that of direct laryngoscopy using a standard Macintosh blade in pediatric patients with a weight ≤10 kg. This weight class was selected because both video-assisted devices are certified for use in this patient population, according to the manufacturer's instructions.
The presented data were limited by a lack of randomization that led to significant differences in the demographic data of each group. However, on average, the time required for tracheal intubation with the TruView EVO2 laryngoscope was more than 20 sec longer than for the C-MAC or direct laryngoscopy. This finding was both statistically and clinically significant. This difference could have resulted from the more extensive experience of the participating anesthesiologists with the Macintosh blade of the C-MAC videolaryngoscope. Although the anesthesiologists who participated in this study had practiced with the TruView device several times before, their experience with this new technique was less extensive than their experience with the C-MAC videolaryngoscope, which is frequently used in our department in adult patients with difficult airways. In addition to this limited experience in the use of the TruView prior to the start of the study, its use was further complicated by the requirement to perform intubation in an indirect manner. The tube also needs to be advanced blindly until its tip enters the visual field of the TruView and is displayed on the attached monitor. Finally, due to the magnified laryngeal view at a 46° anterior refracted angle, tube insertion through the vocal cords remains difficult. The stylet (OptiShapeTM), with its preformed angulation, is not fixed with the tube, so posterior slipping of the tube into the esophagus is a concern when using the TruView EVO2 laryngoscope. Overall, this tool's use requires good hand-eye coordination. Indirect laryngoscopy was also performed using the C-MAC device, but this device is subjectively easier to use due to the similarity in shape with the Macintosh blade.
Malik et al. found that the duration of tracheal intubation with the TruView EVO2 was longer than with other laryngoscopes (20). However, the authors used the devices in adults with immobilized cervical spines. Although our results are in agreement with those obtained by Malik and colleagues, the direct comparability is limited. In contrast to our data, Malik et al. concluded that using the TruView with its optical entrance attached to the top of the blade and fogging on the distal lens were the primary reasons for the prolonged duration of tracheal intubation. In our study, fogging of the TruView lens was reduced by insufflation of oxygen directly to the top of the blade through a special port. Beyond the antifogging effects, the supplemental oxygen insufflation allowed for apneic oxygenation during laryngoscopy and tube placement. The TTI with the TruView was 56 sec on average, and the good tolerance of this long-lasting intubation procedure might have been due to the supplemental oxygen insufflation. Only one child experienced a short period of oxygen desaturation (SpO2 86%). In this case, the TTI was 52 sec, and the oxygen saturation was 100% before and 96% after preoxygenation, perhaps due to a leaky mask and an agitated child. In contrast, in the C-MAC group, the TTI was significantly shorter. Accordingly, the lowest peripheral oxygen saturation was higher (94% in one child), even though no supplemental oxygen was administered in this group. Under standard direct intubation with a Macintosh blade, the lowest peripheral oxygen saturation was 93% in our study.
Although a good view of the vocal cords is occasionally difficult to obtain by conventional direct laryngoscopy, tracheal tube placement is generally easier than when indirect techniques are used because the anatomical and optical axes are aligned. In contrast, indirect techniques may allow for good visualization of the vocal cords in most patients, but endotracheal tube placement is occasionally difficult and even impossible because of the divergent anatomical and optical axes (6,15).
Kim et al. compared the GlideScope with a Macintosh blade in 203 children with and without backward, upward, and rightward pressure (BURP) and found that use of the GlideScope was associated with a better laryngoscopic view but required a longer TTI (11). Li et al. and Barak et al. also demonstrated a longer duration of intubation when the TruView was used compared with the Macintosh blade. Despite the longer duration of the intubation, the laryngoscopic view was rated as good (21,22).
The main limitations of the study were its retrospective character and the variable experience of the participating anesthesiologists with the different devices, leading to significantly faster intubation using the Macintosh blade of the C-MAC videolaryngoscope. Additionally, the fact that no power analysis preceded the study may have additionally limited its informative content. However, a post-hoc power analysis revealed a power of 0.98, which is significant. Calculations were performed using the TTI as the main outcome variable, along with the number of cases, the mean and standard deviation of the statistically significant groups (TruView and Macintosh blade), and a two-tailed alpha value of 0.05. It should be noted that the significant differences in the weights and heights of the subjects did not influence the main results.
In our study, we found that in small children weighing ≤10 kg, tracheal intubation using the TruView EVO2 took nearly twice as long as using the smallest available C-MAC videolaryngoscope blade or conventional direct laryngoscopy. Visualization of the vocal cords was excellent, but the introduction of the tube with the preformed stylet was challenging in certain cases. Nevertheless, no significant difference in SpO2 was found after intubation. This phenomenon may be due to apneic oxygenation via the TruView scope and gives a margin of safety in this special subset of patients. Furthermore, in infants with difficult airways, the use of the TruView scope by an anesthetist with sufficient expertise in the TruView system may represent an alternative for the management of difficult airways. However, without further investigation in a clinical trial, this hypothesis remains speculative. The previously described visualization limitation of fogging when using the TruView device was not observed in our study. In particular, the application of oxygen through a special port on this device reduced fogging and blew secretions away from the optical lens.
ACKNOWLEDGMENTSThis work has not been funded by any sources. No ethical, financial, or other conflict of interest exists regarding the subject matter or materials. No person involved in this study has any financial relationship or competing interests with the manufacturers of either the TruView EVO2 or the C-MAC laryngoscopes. The C-MAC video laryngoscope (Karl Storz GmbH & Co. KG, Tuttlingen, Germany) and the TruView infant EVO2 laryngoscope (Truphatek International Ltd®, Netanya, Israel) are regularly used and are part of the Clinic of Anaesthesiology equipment inventory. There was no source of external funding.
AUTHOR CONTRIBUTIONSMutlak H, Byhahn C, Meininger D, Zacharowski K, Schalk R, and Rolle U wrote the paper and prepared the manuscript. Mutlak H, Meininger D, and Byhahn C conceived the study and performed the statistical analysis. Rosskopf W, Meininger D, and Mutlak H performed most of the tracheal intubations.
No potential conflict of interest was reported.