To evaluate the feasibility of using endovascular repair to treat penetrating arterial injuries with covered stents. Feasibility was examined according to the circumferential extent of the injury.
INTRODUCTION:Surgical trauma often increases the risk of major morbidity and mortality associated with vascular injury, and endovascular repair has many advantages in such situations.
METHODS:Twenty white male domestic pigs weighing 28-38 kg with controlled vascular injuries were divided into four equal groups according to the circumferential extent of their vascular lesion (i.e., no lesion, lesion <50%, lesion >50%, and complete lesion). The left common carotid artery was dissected with proximal and distal control, and this procedure was followed by controlled sectioning of the arterial wall. Local manual compression was applied for 10 min and was followed by endovascular repair with the placement of a 5×50 mm VIABHANTM covered stent using the femoral approach. We also monitored additional variables, such as the duration of the procedures (the mean was 56.3±19.1 min), ultrasound parameters (e.g., maximum arterial diameter, peak systolic and diastolic velocity, and resistance index), arteriography findings, and fluctuations in vital signs (e.g., cardiac output, arterial pressure, and central venous pressure).
RESULTS:The experimental procedure was found to be feasible and reproducible. Repairs were successful in all animals in the control (no lesion) and <50% lesion groups. Success was also achieved in four out of five pigs in the >50% group and in one pig in the complete lesion group.
DISCUSSION:The endovascular repair of an arterial injury is possible, but success depends on the circumferential extent of the arterial lesion. The present experimental model, which involved endovascular techniques, highlighted important factors that must be considered in future studies involving similar animals and materials.
Trauma-related vascular injuries constitute 3% of civilian trauma casualties,1 and 5-10% of all vascular traumas are carotid artery injuries that are usually attributed to direct-penetrating forces.2 The consequences of such trauma-related injuries depend on the type of traumatic mechanism. Avulsion of large vessels, intimal tears, and dissection flaps resulting in luminal thrombosis are generally caused by direct crushing and deceleration injuries from blunt collisions.3 Other damage, such as the laceration of the outer adventitial layer of the arterial wall or the complete transection of the vessel with a high risk of exsanguinating hemorrhage, commonly results from direct-penetrating injuries.4 Both blunt and penetrating trauma forces can disrupt the vessel wall and result in the formation of a pseudoaneurysm.5 Excessive morbidity and mortality rates are associated with penetrating vascular injuries.6
Open wound exploration and appropriate surgical repair is the treatment of choice for polytrauma patients and patients showing signs of peripheral vascular trauma.1,7 Surgical trauma, however, can increase the risk of morbidity in stable patients, and endovascular treatment has been notably beneficial in such cases.8,9 Vessel embolization techniques, for example, are used to treat heavy bleeding from pelvic fractures resulting from blunt trauma.10
Covered stents seem to be ideal for treating arterial ruptures and aneurysms and for sealing off intravascular communication between the true and false lumen of a dissection.3 The use of covered stents in the endovascular repair of trauma-related peripheral vascular injuries, however, is still under development, and few experimental studies have examined this procedure.
Endovascular repair is thought to be inappropriate for complete arterial sections because the distal stump cannot be catheterized,10 but no scientific evidence has proved that this procedure is not possible. The association between the circumferential extent of damage to the vessel wall and the feasibility of endovascular management has not previously been studied.
The present study presented an animal model to examine the feasibility of endovascular repair using covered stents in the treatment of penetrating peripheral vascular injuries. Feasibility was evaluated according to the circumferential extent of the injured arterial wall.
MATERIALS AND METHODSTwenty white male domestic pigs weighing 28 to 37.5 kg (the mean weight was 31.3±2.5 kg) were divided into four groups of five pigs each. Group 1 included control pigs that were not submitted to the controlled carotid injury, which allowed the feasibility of the procedure to be analyzed in models with healthy vessels. In the other three groups, controlled vascular (carotid) lesions were carried out, and the lesions had circumferential extents of 33% (i.e., <50%), 66% (i.e., >50%), and 100% for Groups 2, 3, and 4, respectively. The measurement of the circumferential extent of the arterial lesion was subjective and based on the opinion of two researchers.
All pertinent guidelines prescribed by current Brazilian legislation (Decree 6,899/2009) on the use and protection of animals in experimental research were rigorously followed, and this study was approved by the Ethics Board in Scientific Research of the Medical School of São Paulo University (protocol number: 0603/09).
A BV Pulsera Philips RX 0930
was used to take arteriographs before and after the procedure to evaluate patency, the presence of arterial spasm, extravasation and the flow rate of the contrast (meglumine Ioxitalamato - Telebrix).A Doppler ultrasound was taken with a Sonosite Titan
before the surgical preparation and after the control arteriogram. We evaluated the maximum arterial diameter (in centimeters), the systolic peak velocity (in centimeters per second), the diastolic peak velocity (in centimeters per second), and the resistance index.Before this study began, a pilot study was conducted with four pigs to address technical issues.
Anesthesia and perioperative maneuvers: All animals were pre-anesthetized with intramuscular ketamine (5.0 mg/kg) and midazolam (0.25 mg/kg). Anesthesia was induced with sodium thiopental (20 mg/kg) and an initial volume of NaCl (0.9%) to compensate for fasting-related volume loss. Anesthesia was maintained with inhaled halothane and fentanyl (5 μg/kg) and was followed by continuous intravenous infusion of 0.4 μg/kg/min. Breathing was maintained within physiological parameters with mechanical ventilation, and fluids (20 ml/kg) were continuously administered during surgery.
Surgical technique: Controlled carotid injuries were created with the animals in a prone position. The right femoral artery was dissected to allow for puncture, catheterization, and invasive monitoring of arterial pressure. A longitudinal cervical incision was created through the dissection of the left common carotid artery, and the incision was controlled by means of two short incisions made distally and proximally to the cervicotomy, where the vascular clamps were placed. Xylocaine (2%) was administered locally.
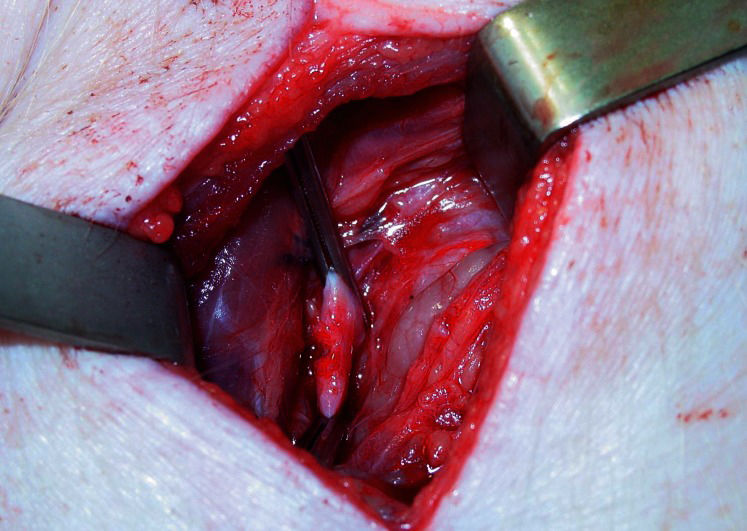
Next, the arterial wall was sectioned (Fig. 1), and the subcutaneous and cutaneous planes were sutured. The sutures in three planes mimicked the action of perilesional tissue in penetrating trauma when there is no access incision.
After releasing the vascular clamps, the site was manually compressed for ten minutes before the endovascular procedure began. This period of manual compression and fluid administration mimicked the prehospital care received by trauma patients.
The left common femoral artery was cannulated with an 8F introducer, and this process was followed by systemic heparinization (145 U/kg). A control arteriogram was carried out using a 0.0035-inch hydrophilic guidewire and a 5F VERT catheter to identify the location of the lesion (Figure 2). A 5×50 mm VIABAHN® covered stent was released as soon as the guidewire passed over the lesion. At this time, papaverine (0.7 mg/kg) and heparin (15 U/kg) were administered via a catheter.
The animals were sacrificed at the end of the procedures while still under general anesthesia.
Assessment of the procedure's feasibility: After the successful release of the covered stent, another arteriogram was conducted to examine the stent placement and luminal patency at the site of implantation and distal to the implantation site (Figure 3).
Local and distal blood flow was registered by Doppler ultrasonography before and after the procedures, and these data were used to assess peak systolic and diastolic velocity and the resistance index.
Statistical analysis: The data were analyzed using parametric (Student's t test) and nonparametric (Wilcoxon signed-rank test) procedures to compare the quantitative parameters (means and standard deviation) observed before and after the procedures. The groups were compared by the Kruskal-Wallis test. Differences were considered significant at the 95% confidence level (p<0.05).
RESULTSThe control arteriography resulted in the successful placement of covered stents (introduced through the left femoral artery) to repair a perforating lesion in the left carotid artery. The procedure was successful in all five pigs in the control group (no lesion), in all five pigs in the group with lesions measuring 33% in circumference (the <50% group), in four pigs in the group with lesions measuring 66% in circumference (the >50% group) and in one pig with a complete lesion (the 100% group).
The duration of the complete procedure from the induction of anesthesia to the control arteriography varied from 38 to 118 min (the mean duration was 56.3±19.1 min). After the lesion was induced, the length of time from the clamp release to the control arteriography varied from 17 to 45 min (the mean time was 27.0±6.9 min).
In 14 (70.0%) successful procedures (not including the sole successful procedure in Group 4), the mean maximal arterial diameter before the procedure decreased significantly from 0.50±0.04 mm to 0.45±0.07 mm after the procedure (t = 0.02; T = 11.5; p<0.025). Peak systolic and diastolic velocities increased significantly after the procedures in all groups, but no differences were observed in peak resistance after the procedures (Table 1). These parameters did not vary significantly when comparing Groups 1, 2, and 3 among themselves (Table 2).
Doppler ultrasonography parameters (means ± standard deviation) before the lesion was created and after the placement of the covered stent and control arteriography with a perforating lesion model.
| Doppler ultrasonography parameters | Before | After | Student's t test | Wilcoxon signed-rank test |
|---|---|---|---|---|
| Maximum arterial diameter | 0.50±0.04 | 0.45±0.07 | p = 0.02 | T = 15; p<0.025 |
| Peak systolic velocity | 56.18±13.83 | 65.28±17.48 | p = 0.05 | T = 18; p<0.025 |
| Peak diastolic velocity | 16.14±5.53 | 24.40±9.96 | p = 0.00 | T = 9; p<0.005 |
| Resistance index | 0.73±0.08 | 0.67±0.11 | p = 0.09 | T = 24.5; p>0.05 |
Doppler ultrasonography parameters (means ± standard deviation) before the lesion was created and after the placement of the covered stent and control arteriography in control and experimental groups.
| Doppler ultra-sonography parameters | Group 1 | Group 2 | Group 3 | Kruskal-Wallis |
|---|---|---|---|---|
| Maximum arterial diameter | ||||
| Before | 0.50±0.03 | 0.52±0.07 | 0.47±0.04 | |
| After | 0.44±0.06 | 0.46±0.08 | 0.47±0.05 | |
| Mean difference | -0.06 | -0.06 | -0.01 | H = 1.75; p>0.10 |
| Peak systolic velocity | ||||
| Before | 48.48±7.05 | 62.22±20.18 | 54.84±10.04 | |
| After | 61.64±15.00 | 71.18±21.35 | 62.47±18.05 | |
| Mean difference | 13.26 | 8.96 | 4.10 | H = 0.22; p>0.30 |
| Peak diastolic velocity | ||||
| Before | 16.36±3.28 | 16.24±7.48 | 15.75±6.59 | |
| After | 20.98±3.70 | 26.10±3.51 | 23.26±19.11 | |
| Mean difference | 4.62 | 6.66 | 10.8 | H = 0.61; p>0.30 |
| Resistance index | ||||
| Before | 0.66±0.06 | 0.79±0.09 | 0.73±0.03 | |
| After | 0.70±0.07 | 0.62±0.08 | 0.69±0.17 | |
| Mean difference | 0.04 | -0.16 | -0.03 | H = 4.52; p>0.08 |
In most cases, arterial spasm and the leakage of contrast were present in the preprocedure arteriograms. In the postprocedure arteriography findings, we observed cases where the procedure was not successful (Table 3).
DISCUSSIONResearchers continue to debate the best way to approach injuries to the proximal common carotid and distal internal carotid arteries in stable patients. Approaches vary from routine exploration to selective exploration based on either clinical findings alone or based on clinical findings combined with radiological features. This debate continues even though the feasibility and safety of endovascular management has already been well established.9
The use of covered stents has been proposed for the management of femoral artery lesions,11 injuries to the subclavian and axillary arteries,12 and even in carotid artery trauma.2,13,14 These stents can help avoid the high rates of morbidity and mortality associated with surgical exploration. Covered stents have important advantages. For example, they can be inserted with a minimally invasive procedure and deployed through a remote site of percutaneous access under local anesthesia.3 Most previous studies, however, included unhealthy arteries (i.e., those with atherosclerosis), and covered stents have been developed with a focus on diseased arteries. The endovascular management of lesions in normal arteries must be studied to establish the feasibility of this procedure in the treatment of perforating blunt trauma injuries and to reveal the long-term behavior of covered stents. This research can also help determine the circumferential extent of a lesion that can be managed with an endovascular approach. All of these issues can be answered in experimental studies.
The intent of the present study was to create an animal model to understand better the endovascular repair of penetrating injuries to peripheral arteries. A pilot study that included four pigs was carried out so that technical difficulties could be solved before the full experiment began. The first difficulty was the occurrence of vasospasm, which is common in experimental vascular studies with swine because their peripheral blood vessels are prone to vasospasm and rupture relatively easily.15 The local administration of xylocaine (2%) and the administration of papaverine (0.7 mg/kg) via a catheter solved this problem. Systemic heparinization (140 U/kg) after the placement of the introducer and local heparinization (15 U/kg) via a catheter after the stent was released addressed problems with intrastent thrombosis.
The covered stent placement was successful in all of the animals in the control group (those without a carotid lesion) and in the group with lesions with a circumference of 33% (<50%). Furthermore, the covered stent placement was successful in 80% of the animals with lesions with a circumference of 66% (>50%) and, surprisingly, in one pig with a complete (100%) lesion. These results point to the feasibility of the experimental procedure and show that success is associated with the circumferential extent of the lesion.
These results are especially significant because pigs share important aspects of cardiovascular anatomy and physiology with humans.15 There are differences, however, in the extracranial cerebrovascular anatomy between pigs and humans, and caution should be used when extrapolating from these preliminary findings to surgical practice.
It is important to clarify that the large range in the duration of the procedures (38 to 118 min) was related to the learning curve of the surgical team rather than the circumferential extent of the lesions. Indeed, the first procedures were much longer than the final ones.
The resistance index did not significantly differ before and after the procedure or among Groups 1, 2, and 3. We did not analyze Doppler ultrasonography parameters in the group with complete lesions because the procedure only succeeded in one pig. Nevertheless, it is important to emphasize that the resistance index increased in the group without lesions and decreased in the groups with lesions (i.e., in both the <50% and >50% groups) (Table 2). This difference between the lesioned groups and those without injury could have occurred as a result of cerebral vasoreactivity. In animals with lesions, insufficient cerebral vascular reactivity results in vasodilation, which leads to a decrease in vascular resistance to blood flow. This effect did not occur in the control group.16
The maximum luminal diameter decreased significantly in Groups 1, 2, and 3, and peak systolic and diastolic velocity increased significantly after the procedure; however, none of these variables differed between the three groups. The increase in velocity was expected, due to the decreased compliance of the vessel at the site of the stent implantation.17 This effect has been documented in clinical practice by monitoring patients who received uncoated stents in the internal carotid artery to treat atherosclerotic stenosis. This observation also indicated that a spectral velocity with duplex scan can be used for clinical follow-up as long as it is recognized that the velocity changes with the insertion of stents.
Because we faced difficulties with some aspects of the ultrasonographic assessment, including the measurement of hematoma and atmospheric air and intrastent and distal visualization, the analyzed parameters did not include measures taken distally to the placement of the covered stent. These parameters were only measured in three out of five control pigs, in one pig with a lesion <50% and in one pig with a lesion >50%. The measurements were similar before and after the covered stent placement.
The present results can be useful in the development of endovascular treatment for victims of trauma-related vascular injuries. In addition, the present pig model can contribute to the development of more complete information that will allow an endovascular approach to be applied in humans.