Hepatitis A is an infectious disease caused by the hepatitis A virus (HAV). It is primarily transmitted through oral contact with faeces, humans are the virus’ only reservoir and it is found all over the world.1 The World Health Organisation estimates that there are around 1.4 million new cases every year.2
In Chile, improved sanitary conditions like wastewater treatment, campaigns to promote the consumption of cooked seafood as well as macroeconomic improvements, have helped to reduce the incidence of hepatitis A.3,4 In 2007, Ibarra reported a reduction and shift in seroprevalence of the anti-HAV IgG antibody to later life, from around the age of fifty.1 To date, no reports have been published that compare reduced HAV seroprevalence over time with recent data.
Our aim was to retrospectively evaluate and compare the prevalence of anti-HAV IgG antibodies in two periods (2004–2006 and 2014–2016) separated by a 10-year gap, based on examinations that requested anti-HAV antibody testing, in a reference laboratory belonging to the Hospital Clínico Universidad de Chile [University of Chile Clinical Hospital] in Santiago, which processes samples from various sites in the metropolitan region.
In total, 1014 results were collected and analysed using the mini VIDAS® HAV Total (Biomerieux, France) ELFA technique for anti-HAV IgG and results from males and females (53% male) over two years of age were included. The seroprevalence of anti-HAV IgG was determined for the periods 2004–2006 (498 samples, group A) and 2014–2016 (516 samples, group B) and by age range. The chi-squared test was used for statistical analysis (p<0.05).
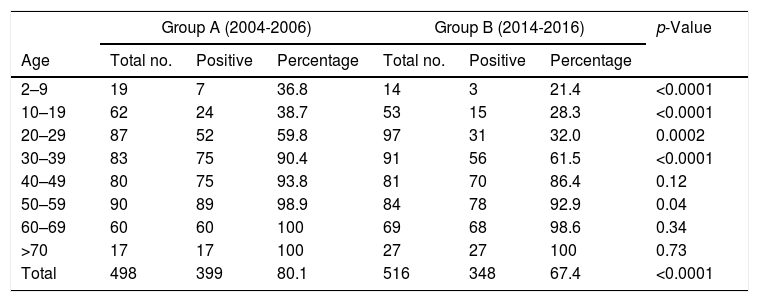
The seroprevalence of anti-HAV antibodies was 80.1% in group A and 67.4% in group B (p<0.0001). A significant drop in antibody levels was observed in both periods in patients aged between 2 and 39 years (p<0.0001). A high anti-HAV IgG seroprevalence was maintained in both groups in the population over the age of 40 (Table 1), with no significant differences. No differences between the genders were found (p=0.12).
Anti-HAV IgG antibody seroprevalence by age range for the periods 2004–2006 and 2014–2016.
| Group A (2004-2006) | Group B (2014-2016) | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Age | Total no. | Positive | Percentage | Total no. | Positive | Percentage | |
| 2–9 | 19 | 7 | 36.8 | 14 | 3 | 21.4 | <0.0001 |
| 10–19 | 62 | 24 | 38.7 | 53 | 15 | 28.3 | <0.0001 |
| 20–29 | 87 | 52 | 59.8 | 97 | 31 | 32.0 | 0.0002 |
| 30–39 | 83 | 75 | 90.4 | 91 | 56 | 61.5 | <0.0001 |
| 40–49 | 80 | 75 | 93.8 | 81 | 70 | 86.4 | 0.12 |
| 50–59 | 90 | 89 | 98.9 | 84 | 78 | 92.9 | 0.04 |
| 60–69 | 60 | 60 | 100 | 69 | 68 | 98.6 | 0.34 |
| >70 | 17 | 17 | 100 | 27 | 27 | 100 | 0.73 |
| Total | 498 | 399 | 80.1 | 516 | 348 | 67.4 | <0.0001 |
Our study, which uses current data, confirms the trend identified by Ibarra,1 accentuating the seroprevalence shift to even later in life. The fall in seroprevalence under the age of 40 could be explained by the fact that subjects have not come into contact with, or been vaccinated against HAV. Improved sanitary conditions and Chile's economic development have helped reduce the prevalence of HAV contact among the population. However, epidemic outbreaks arise every three to five years, making Chile a country with an epidemiological pattern of intermediate endemicity.3
An outbreak of hepatitis A was recorded in Chile at the end of 2016 and the beginning of 2017, with 706 cases of hepatitis caused by the hepatitis A virus reported by epidemiological week 18. 36% of the cases were concentrated in the metropolitan region and a rate of 3.4 cases per 100,000 population was identified. The outbreak primarily affected subjects between the ages of 15 and 39 years, with anal–oral contact in men who have sex with men being one of the primary factors,3 and at least one case required a liver transplant. The usual course of hepatitis A virus infection is predominantly benign, although the Acute Liver Failure Study Group and the United Network for Organ Sharing Patient Population suggest that older patients are at increased risk of developing severe acute hepatitis.
In light of the above, our findings appear even more relevant given that the population affected by the outbreak is the same population that saw a drop in anti-HAV antibody seroprevalence according to the results of this study. It is worth noting that the HAV vaccine, which is highly immunogenic and offers protection to both children and adults, has been available in Europe since 1991 and in the USA since 1996.5 Villena et al. recommend vaccinating the at-risk population and gradually rolling out the HAV vaccination programme, prioritising those areas that have seen the most cases.3
In conclusion, it can be confirmed that our site has seen a fall in anti-HAV antibody seroprevalence over the last decade. Incorporation of the HAV vaccine in the early stages of the universal vaccination plan is recommended, with a particular focus on the population under the age of 40 years as this group is more susceptible to acquiring and presenting a severe course of the infection.
Please cite this article as: Miranda J, Valenzuela M, Hurtado C, Vera DB, Brahm J. Disminución de la seroprevalencia del virus de la hepatitis A en Santiago de Chile, comparación de una década. Gastroenterol Hepatol. 2019;42:248–249.