It is estimated that diagnostic medical radiation exposure may be responsible for 0.5–2% of cancers worldwide. Because of the relapsing course of Crohn's disease (CD), these patients usually require multiple ionising radiation test.
ObjectiveStimulating the total cumulative effective dose received by our CD patients and identifying the risk factors associated with the exposure to a cumulative effective dose due to the disease (CEED) ≥50mSv.
Materials and methodsRetrospective cohort study (2001–2014). Population: patients with CD. Risk dose ≥50mSv. For calculating de cumulative effective dose and the CEED, all the ionising test done were taken. For identifying predictive factors for receiving a CEDD ≥50mSv, an univariate and a multivariate logistic regression analyses were performed using a ≥50mSv dose as dependent variable.
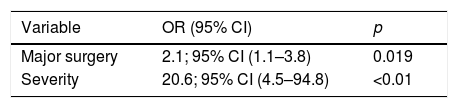
ResultsOf the 267 patients analysed the 24.6% of them received a cumulative effective dose ≥50mSv and the 15.2% a CEED ≥50mSv. In the multivariate analysis, the following variables were identified as independent predictors associated with a CEDD ≥50mSv: major surgery (OR=2.1; IC95% [1.1–3.8]; p=0.019) and severity (OR=20.6; IC95% [4.5–94.8]; p<0.01).
ConclusionsPatients with CD are more at risk of receiving risk CEED, so it would be advisable to monitor the cumulative effective dose received to anticipate our intervention in order to avoid reaching that dose. The ultrasounds and abdominal resonance enterography are alternatives in these cases, although their accessibility is limited in some centres.
La exposición a radiación ionizante procedente de pruebas médicas puede ser responsable del 0,5-2% de los cánceres a nivel mundial. Debido al curso crónico en brotes y al comienzo temprano de la enfermedad de Crohn (EC), estos pacientes requieren múltiples exploraciones radiológicas ionizantes.
ObjetivoEstimar la cantidad de radiación ionizante que reciben nuestros pacientes con EC así como identificar aquellos factores de riesgo asociados a recibir una dosis de radiación debida a su enfermedad (DEED)≥50mSv.
Material y métodosEstudio de cohorte retrospectivo (2001-2014). Población: pacientes con EC. Dosis de riesgo ≥50mSv. Para el cálculo de dosis efectiva total y DEED se recogieron las exploraciones radiológicas a las que fueron sometidos. Para la identificación de factores predictivos asociados a recibir una DEED ≥ 50mSv se realizó mediante regresión logística uni- y multivariante utilizando la dosis ≥50mSv como variable dependiente.
ResultadosDe los 267 pacientes con EC analizados, el 24,6% recibieron una dosis efectiva total ≥50mSv y el 15,2% una DEED ≥50mSv. En el análisis multivariante las variables que de forma independiente se asociaron a recibir una DEED ≥50mSv fueron la cirugía mayor (OR= 2,1; IC95% [1,1-3,8]; p=0,019) y la gravedad (OR=20,1; IC95% [2,7-148,4]; p<0,001).
ConclusionesLos pacientes con EC están más expuestos a recibir una DEED de riesgo, por lo que sería conveniente monitorizar la DE recibida para anticipar nuestra actuación con el fin de evitar llegar a dicha dosis. La ecografía y la entero-RNM son alternativas a considerar en estos casos, aunque su accesibilidad está limitada en algunos centros.
Ionising radiation exposure due to diagnostic medical testing is estimated to be responsible for 0.5–2% of all malignancies worldwide,1 with an effective dose (ED) ≥50mSv having been involved in the development of solid tumours, particularly of the large intestine.2
The chronic natural history of Crohn's disease (CD), and the early age of onset, mean that these patients undergo multiple radiological examinations over the course of their lives; according to previous studies, up to 20% of patients with inflammatory bowel disease (IBD) are exposed to high doses of radiation. Therefore, the risk of cancer, which is already present, may increase due to both their underlying disease and the medical treatments they require; however, very few published studies are available.
The aim of this study is to estimate ionising radiation exposure in our Crohn's disease patients, and to identify those risk factors associated with exposure to higher doses of radiation.
Material and methodsStudy designAll patients being treated by our hospital's specialised IBD clinic were analysed retrospectively based on their electronic medical records from 2001 until 2014. Only those patients with CD were included, while patients diagnosed with ulcerative colitis, microscopic colitis and indeterminate colitis were excluded. Our clinic treats patients from the age of 14 years, and belongs to a medium-sized hospital serving 250,000 people.
Demographic data (age and gender) and characteristics of the disease (years since diagnosis, age at diagnosis, behaviour, location, perianal disease, number of major surgeries and type of treatment) were collected. Those patients requiring immunosuppressant and/or biological drug treatment and/or surgery to control their disease were considered to have severe forms of the disease.3
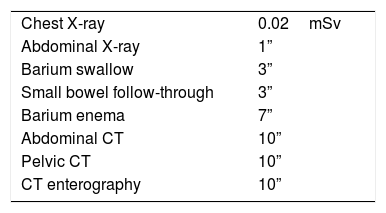
All radiological examinations were collated, and the cumulative effective dose (CED) and the cumulative effective dose due to the disease (CEDD) to which they were exposed were calculated. All imaging tests performed on each patient using ionising radiation were used to calculate the CED. Furthermore, all processes (regardless of the department ordering the tests) were reviewed for the CEDD, but only those tests requested for the patient's CD were used. The mSv calculation was based on the “Radiation Protection 118: Referral Guidelines for Imaging” and on articles found on PUBMED1,2,4 (Table 1).
Risk factors were calculated using CEDD ≥50mSv as the cut-off point, taking into account epidemiological studies in which such radiation increases the risk of developing cancer.5
Statistical analysesPercentages and medians were used with their interquartile range (IR) to describe categorical and quantitative variables. The chi-squared test was used to compare categorical variables, while the Student's t-test was used to compare quantitative variables. A univariate logistic regression analysis, followed by a multivariate logistic regression analysis, were performed to identify predictive factors associated with receiving a CEDD ≥50mSv. Only those variables that were significant in the univariate analysis, and other clinically significant variables, were included as independent variables in the multivariate analysis. All hypotheses were two-tailed and p-values less than 0.05 were considered statistically significant. Statistical analysis was performed using SPSS software (version 20.0).
Results684 patients undergoing follow-up at the IBD clinic were analysed, 297 of whom had been diagnosed with CD.
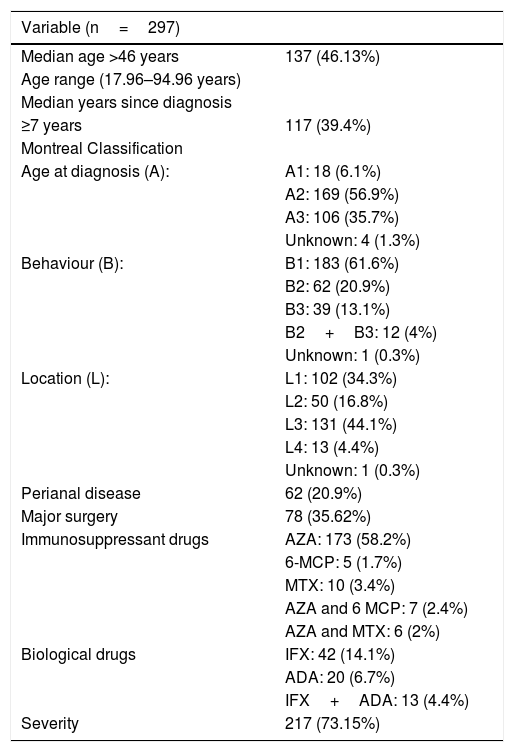
Demographic data and characteristics of the diseaseApproximately half of the 297 patients included were men, with a median age of 46.2 years (IR=35.5–58.4), while the median number of years since diagnosis was 7 (IR=4–14). Most of our patients had disease with inflammatory behaviour (61.6%), and the most common location was the ileocolon (44.1%). Over the course of their disease, 44.10% only received immunosuppressants, 1.68% received only biological drugs and 23.57% received combined immunosuppressant and biological drug therapy. 73% of the patients were considered to have severe forms of the disease. The remaining characteristics of the disease are summarised in Table 2.
Baseline characteristics.
| Variable (n=297) | |
|---|---|
| Median age >46 years | 137 (46.13%) |
| Age range (17.96–94.96 years) | |
| Median years since diagnosis | |
| ≥7 years | 117 (39.4%) |
| Montreal Classification | |
| Age at diagnosis (A): | A1: 18 (6.1%) |
| A2: 169 (56.9%) | |
| A3: 106 (35.7%) | |
| Unknown: 4 (1.3%) | |
| Behaviour (B): | B1: 183 (61.6%) |
| B2: 62 (20.9%) | |
| B3: 39 (13.1%) | |
| B2+B3: 12 (4%) | |
| Unknown: 1 (0.3%) | |
| Location (L): | L1: 102 (34.3%) |
| L2: 50 (16.8%) | |
| L3: 131 (44.1%) | |
| L4: 13 (4.4%) | |
| Unknown: 1 (0.3%) | |
| Perianal disease | 62 (20.9%) |
| Major surgery | 78 (35.62%) |
| Immunosuppressant drugs | AZA: 173 (58.2%) |
| 6-MCP: 5 (1.7%) | |
| MTX: 10 (3.4%) | |
| AZA and 6 MCP: 7 (2.4%) | |
| AZA and MTX: 6 (2%) | |
| Biological drugs | IFX: 42 (14.1%) |
| ADA: 20 (6.7%) | |
| IFX+ADA: 13 (4.4%) | |
| Severity | 217 (73.15%) |
Montreal Classification, A (age at diagnosis), A1: <17 years, A2: 17–40 years, A3: >40 years. B (behaviour), B1: inflammatory, B2: stricturing, B3: penetrating. L (location), L1: ileum, L2: colon, L3: ileocolon, L4: upper GI tract.
ADA: adalimumab; AZA: azathioprine; IFX: infliximab; 6-MCP: 6-mercaptopurine; MTX: methotrexate.
The median cumulative radiation dose received was 20.8mSv (IR=5.9–48.3mSv), with 24.6% of patients having a CED ≥50mSv. The median radiation dose received as a result of imaging scans to manage the disease was 10mSv (IR=3–31mSv), with 15.2% having a CEDD ≥50mSv. The most common tests ordered were: abdominal X-ray (63%), small bowel follow-through (58.9%) and a CT scan of the abdomen and pelvis (47.9%). Only 8.7% received MR enterography.
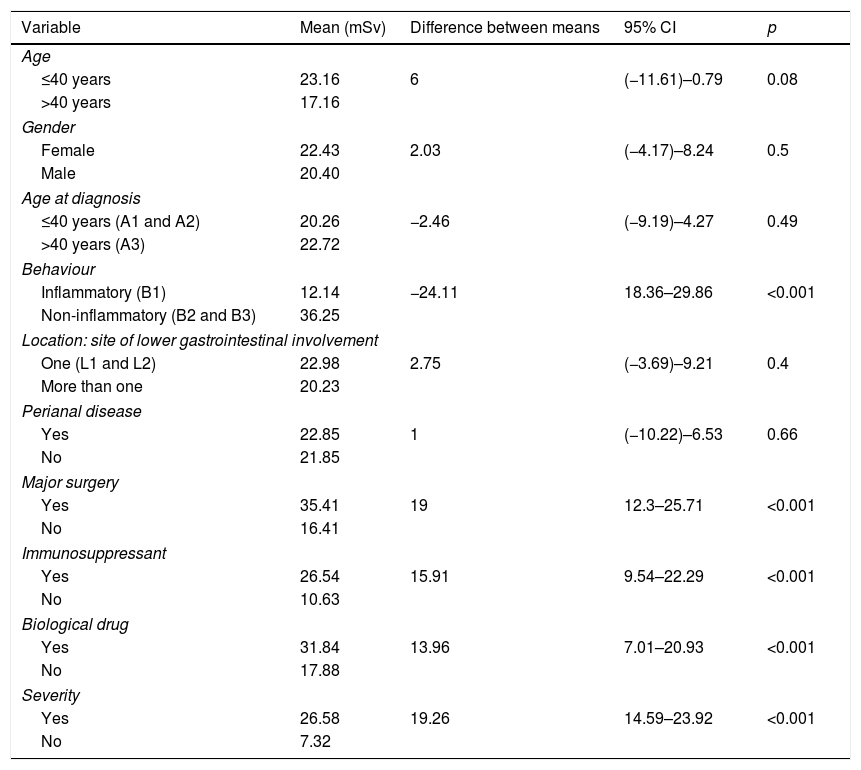
With regard to patients who received a higher average CEDD, patients whose disease showed inflammatory behaviour, those requiring major surgery, those who received immunosuppressant and biological drug therapy and those whose disease showed some degree of severity, are statistically significant. Patients aged >40 years, female patients, those with one area of gastrointestinal involvement (ileum or colon) and those with perianal disease (Table 3) are not statistically significant.
Average CEDD received.
| Variable | Mean (mSv) | Difference between means | 95% CI | p |
|---|---|---|---|---|
| Age | ||||
| ≤40 years | 23.16 | 6 | (−11.61)–0.79 | 0.08 |
| >40 years | 17.16 | |||
| Gender | ||||
| Female | 22.43 | 2.03 | (−4.17)–8.24 | 0.5 |
| Male | 20.40 | |||
| Age at diagnosis | ||||
| ≤40 years (A1 and A2) | 20.26 | −2.46 | (−9.19)–4.27 | 0.49 |
| >40 years (A3) | 22.72 | |||
| Behaviour | ||||
| Inflammatory (B1) | 12.14 | −24.11 | 18.36–29.86 | <0.001 |
| Non-inflammatory (B2 and B3) | 36.25 | |||
| Location: site of lower gastrointestinal involvement | ||||
| One (L1 and L2) | 22.98 | 2.75 | (−3.69)–9.21 | 0.4 |
| More than one | 20.23 | |||
| Perianal disease | ||||
| Yes | 22.85 | 1 | (−10.22)–6.53 | 0.66 |
| No | 21.85 | |||
| Major surgery | ||||
| Yes | 35.41 | 19 | 12.3–25.71 | <0.001 |
| No | 16.41 | |||
| Immunosuppressant | ||||
| Yes | 26.54 | 15.91 | 9.54–22.29 | <0.001 |
| No | 10.63 | |||
| Biological drug | ||||
| Yes | 31.84 | 13.96 | 7.01–20.93 | <0.001 |
| No | 17.88 | |||
| Severity | ||||
| Yes | 26.58 | 19.26 | 14.59–23.92 | <0.001 |
| No | 7.32 | |||
Statistical analysis using Student's t-test.
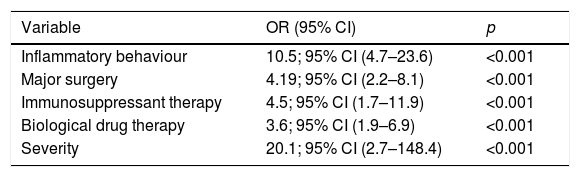
In the univariate analysis, patients whose disease showed inflammatory behaviour (OR=10.5; 95% CI [4.7–23.6]; p<0.001), patients receiving immunosuppressant (OR=4.5; 95% CI [1.7–11.9]; p<0.001) or biological drug therapy (OR=3.6; 95% CI [1.9–6.9]; p<0.001), patients requiring major surgery (OR=4.19; 95% CI [2.2–8.1]; p<0.001) and patients whose disease was considered to be severe (OR=20.1; 95% CI [2.7–148.4]; p<0.001) were associated with receiving a CEDD ≥50mSv; this is statistically significant (Table 4). However, in the multivariate analysis, the variables that were independently associated with receiving a CEDD ≥50mSv were major surgery (OR=2.1; 95% CI [1.1–3.8]; p=0.019) and severity (OR=20.1; 95% CI [2.7–148.4]; p<0.001) (Table 5).
Factors associated with receiving an ED >50mSv due to the disease. Univariate analysis.
| Variable | OR (95% CI) | p |
|---|---|---|
| Inflammatory behaviour | 10.5; 95% CI (4.7–23.6) | <0.001 |
| Major surgery | 4.19; 95% CI (2.2–8.1) | <0.001 |
| Immunosuppressant therapy | 4.5; 95% CI (1.7–11.9) | <0.001 |
| Biological drug therapy | 3.6; 95% CI (1.9–6.9) | <0.001 |
| Severity | 20.1; 95% CI (2.7–148.4) | <0.001 |
Other variables with no statistically significant association were: duration of the disease, age at diagnosis, gender, location and perianal disease.
Over recent decades, the development of imaging tests has been very important, becoming more widely available at most hospitals. However, many of these tests emit ionising radiation with well-known cancer-causing effects.
The first studies to investigate the relationship between receiving ionising radiation and the risk of developing tumours focused on atomic bomb survivors and nuclear power plant workers.6,7 They showed that there was a risk of malignancy if doses greater than 35–40mSv were received. It was later recognised that the ED received has a cumulative effect, and 50mSv was defined as the high-risk dose.6,8 We have therefore taken this value as the cut-off point.
Despite there being a clear relationship between cancer and ionising radiation, some patients are exposed to high doses, especially those with chronic diseases who require scans to manage and/or control their disease. During the time period analysed, approximately 15.2% of our patients received a high-risk dose due only to tests ordered for their disease; however, if we take into account all ionising radiation tests, 24.6% received a high-risk dose. Our results are similar to those of earlier studies since the percentage of patients in those studies8,9 who received a CED ≥50mSv ranged between 2.9% and 20%, with patients with CD receiving this dose most often.
Children, women and individuals under the age of 40 are the most radiosensitive.8,9 In our case, the population that received the highest dose of radiation included women and patients over the age of 40. We must also point out that patients with a more aggressive form of disease (behaviour B2 and B3), greater disease severity and those requiring immunosuppressant therapy and major surgery also received higher doses. This is due to the fact that older patients tend to have had the disease for longer, and patients with a more severe form of disease, with complications, tend to need more scans to detect it.
For the multivariate analysis, the variables that were associated independently with receiving a CEDD ≥50mSv were major surgery and severity. Despite our study focusing more on CEDD, other authors have studied variables associated with receiving a CED ≥50mSv in patients with IBD. In one of these studies,10 the variables used were an age at diagnosis of 40 years or more, disease behaviour A1, major surgery and IBD with a duration of more than 8 years. In another study, the variables used were smoking status, duration of the disease and prior major surgery.11 In another recent publication12 regarding a study conducted in CD patients, penetrating phenotype, abdominal surgery, steroid resistance or dependence and anti-TNF and azathioprine therapy were predictive factors for high-risk ED exposure. Although the populations included in the various studies are very different, it must be highlighted that both our study and the referenced studies agree that the relationship between major surgery and receiving a high-risk dose is statistically significant.
In our study, the imaging tests most commonly ordered, in order of frequency, were abdominal X-ray, small bowel follow-through and CT scan of the abdomen and pelvis. The fact that small bowel follow-through is the second most common exam may be explained by the fact that this exam was more widely available than CT scans during the first 10 years of the study, although this has since changed.
Over recent decades, MR enterography has become one of the main exams for studying the small intestine in patients with IBD.13 However, it must be noted that only 8.7% of patients underwent MR enterography imaging during our study. Despite this technique being widely accepted for the follow-up and/or diagnosis of complications, our study demonstrates that some centres cannot access this type of imaging test as easily as other types, such as CT scans.2
CD patients have an increased rate of colorectal cancer, skin cancers and lymphomas. This is due to chronic inflammation and the use of immunosuppressants, and is also affected by the amount of ionising radiation received.9 During our data collection period, 11 patients developed some type of cancer (the most common were gastrointestinal tract, skin and haematological cancers), and only 3 of them had received a CEDD ≥50mSv. These results must be interpreted cautiously, since our study is retrospective and was not designed to study the risk of developing tumours after a certain dose of radiation.
It must be highlighted that our study has certain limitations due to the fact it is retrospective. The CED could also be underestimated, since some of the ionising radiation tests have no equivalence in mSv.
To conclude, patients with CD are at high risk of receiving high doses of ionising radiation. In the most radiosensitive patients and in those patients with more severe forms of disease with an increased need for this type of test, we must try to reduce the number of ionising radiation diagnostic tests. It would also be advisable to monitor the ED received in order to anticipate our actions and avoid reaching a high-risk dose. Ultrasound and MR enterography are good alternatives in these cases, although their availability is limited at some centres.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Merino Rodríguez E, Carrera Alonso E, Torralba González de Suso M, Sánchez da Silva M, Martínez López M, Sánchez-Tembleque Zarandona MD. Exposición a radiación diagnóstica en pacientes con enfermedad de Crohn: estudio retrospectivo en un hospital medio y sus factores predictivos. Gastroenterol Hepatol. 2018;41:97–102.