Individuals with major depressive disorder (MDD) are usually observed making inappropriate risky decisions. However, whether and to what extent MDD is associated with impairments in risky decision-making remains unclear. We performed a three-level meta-analysis to explore the relationship between risky decision-making and MDD.
MethodWe searched the Web of Science, PubMed, Scopus, and PsycINFO databases up to February 7, 2023, and calculated Hedges' g to demonstrate the difference in risky decision-making between MDD patients and healthy controls (HCs). The moderating effect of sample and task characteristics were also revealed.
ResultsAcross 73 effect sizes in 39 cross-sectional studies, MDD patients exhibited greater risk-seeking than HCs (Hedges' g = 0.187, p = .030). Furthermore, age (p = .068), region (p = .005), and task type (p < .001) were found to have moderating effects. Specifically, patients preferred risk-seeking over HCs as age increased. European patients showed significantly increased risk-seeking compared to American and Asian patients. Patients in the Iowa Gambling Task (IGT) exhibited a notable rise in risk-seeking compared to other tasks, along with an increased risk aversion in the Balloon Analogue Risk Task (BART). The multiple-moderator analysis showed that only task type had significant effects, which may be explained by a tentative framework of "operationalization-mechanism-measure" specificity.
ConclusionsMDD patients generally exhibit higher risk-seeking than HCs. It implies that impaired risky decision-making might be a noteworthy symptom of depression, which should be placed more emphasis for clinical management and psycho-education.
With the growing attention to the link between mental health and risky decision-making, increasing studies have revealed that mental disorders could affect such decision-making, resulting in certain extent of risky decision-making impairment. For example, individuals with bipolar disorder (Ramírez-Martín et al., 2020) and attention-deficit/hyperactivity disorder (Dekkers et al., 2016) preferred risk-seeking over healthy controls (HCs), while those with social anxiety and obsessive-compulsive disorder have exhibited increased risk aversion (Buelow, 2020). Major Depressive Disorder (MDD) is a prevalent mood disorder and a leading determinant of disability worldwide (GBD, 2020). Thus, whether MDD patients exhibit such risky decision-making impairment should also be explored.
MDD patients often experience negative cognitive bias, motivational deficits, indecision, and other dysfunctions that may bias their evaluations of risk and reward, resulting in inappropriate risky decision-making. Growing evidence has revealed the crucial impacts of MDD on risky decision-making. Specifically, MDD patients frequently engage in risky behaviors such as self-harm (Xu et al., 2023) and substance abuse (Jetelina et al., 2016). Moreover, empirical studies have found that MDD patients exhibit different risk preferences from HCs (e.g., Cella et al., 2010; Kong et al., 2022). Additionally, neuroimaging studies have also shown that the neural circuitry involved in risky decision-making overlaps with that impaired in MDD (e.g., left ventral striatum, right prefrontal cortex) (Gao et al., 2021; Husain et al., 2021), and these regions are involved in how MDD affects risky decision-making (Hiser & Koenigs, 2018).
Despite substantial evidence linking MDD and risky decision-making, previous findings regarding the magnitude and direction of this link are inconclusive. Some studies have shown that MDD patients exhibit increased risk-seeking (e.g., Deisenhammer et al., 2018; Oldershaw et al., 2009) since their impaired learning abilities make it difficult to optimize decision-making (Tom et al., 2007). However, some other studies have revealed that MDD patients exhibit increased risk aversion (e.g., Chapman et al., 2007; Ji et al., 2021). Because of anhedonia and increased loss sensitivity, these patients do not desire great gains or accept losses with inflated probabilities, thus presenting more conservative behaviors (Vrieze et al., 2013). Moreover, some studies found no difference between MDD patients and HCs in risky decision-making (e.g., Gao et al., 2021; Hart et al., 2019).
These mixed findings might partly relate to a lack of power due to small sample sizes. In any case, whether MDD is associated with increased risk-seeking or risk aversion remains unclear. This is troublesome when conflicting interpretations are applied to understand phenomena or provide suggestions for interventions. Thus, to clarify the associations between MDD and risky decision-making, we performed a meta-analysis to assess risky decision-making in individuals with and without MDD. Moreover, we also attempted to uncover potential moderators, including sample and task characteristics, to address inconsistent findings better.
On the one hand, sample characteristics are crucial for differences in effect sizes in previous meta-analyses on other mental disorders and risky decision-making (e.g., Dekkers et al., 2016; Mukherjee & Kable, 2014). Different demographics may lead to inconsistent risk preferences in MDD. For example, age-related differences in risk preference have been identified in HCs (Mata et al., 2011), yet it is unclear whether the same applies in MDD patients. Similarly, Han et al. (2012) found differences in risk preference between male and female MDD patients, but further research is required to test its robustness. Moreover, depression symptoms affect risk preference. Some studies found a significant correlation between depression severity and risk preference (e.g., Cella et al., 2010), while others found no significant relationship (e.g., Must et al., 2006). Furthermore, the impact of the MDD phases (acute and euthymic) (Kong et al., 2022; Siqueira et al., 2021) and suicide attempts (e.g., Hegedűs et al., 2021) on risky decision-making also remains unclear. In sum, we explored the potential moderating effects of sample characteristics, including demographics and depression symptoms, on risky decision-making in MDD.
On the other hand, we underscored the role of task characteristics which was ignored in previous studies, because different tasks used to evaluate risk preference might bias the results. Risky decision-making refers to weighing and choosing between options with uncertain outcomes (Kahneman & Tversky, 1979), and risk-seeking refers to the tendency to choose risky options, as opposed to risk aversion. Behavioral tasks are the mainstream way to evaluate risk preference, including (a) Risky Choice Tasks (i.e., variants of tasks in which participants choose between a low-risk and a high-risk option), such as Game of Dice Task (GDT) and Wheel of Fortune (WOF); (b) dynamic gambling tasks, such as Iowa Gambling Task (IGT) and Cambridge Gambling Task (CGT); and (c) tasks closer to real-world contexts, such as Balloon Analogue Risk Task (BART). Although these tasks are often used to measure risky decision-making, they differ in design, indicator meaning, and some other aspects, leading to low correlations across tasks (Frey et al., 2017). Previous studies have shown differing, even contradictory, risk preferences of MDD patients in various tasks, such as increased risk-seeking in IGT (e.g., Moniz et al., 2016) but increased risk aversion in BART (e.g., Hevey et al., 2017). Likewise, another study (Deisenhammer et al., 2018) revealed that MDD patients showed different risk preferences between GDT and IGT. Furthermore, reviews of other mental disorders, such as bipolar disorder (Ramírez-Martín et al., 2020) and psychosis-spectrum disorders (Purcell et al., 2022), have confirmed the essential role of task characteristics in risk preference. Therefore, this study considered task characteristics as potential moderators to test whether MDD patients' risk preferences varied across tasks.
The present study conducted a meta-analysis to clarify the associations between MDD and risky decision-making. We expected to answer two questions: (a) Do MDD patients exhibit different risk preferences from HCs? (b) Do sample characteristics and task characteristics moderate these differences? These answers will help us comprehensively understand the similarities and differences in risky decision-making between MDD patients and HCs. Moreover, impaired risky decision-making might be a noteworthy characteristic of depression. In this context, we need to pay more attention to this characteristic for clinical management and psycho-education.
MethodsSearch strategiesWe preregistered this meta-analysis study on PROSPERO (CRD42021275900). We searched studies through Web of Science, PubMed, Scopus, and PsycINFO using a combination of three types of search terms: (a) depression-related terms; (b) terms related to risky decision-making; and (c) terms related to behavioral tasks (see Supplementary Table 1). Only English articles in the psychology and psychiatry domain from the inception of each database to February 7, 2023 were included.
Inclusion criteriaThe eligibility criteria for study inclusion were as follows: (1) published in a peer-reviewed journal; (2) included a group with MDD as the primary diagnosis; (3) included an HCs group with no diagnosed psychopathology; and (4) included a behavioral task of risky decision-making. Additional criteria implemented during the full-text review stage were (5) diagnoses based on validated criteria and (6) reported sufficient details to calculate effect sizes and variance.
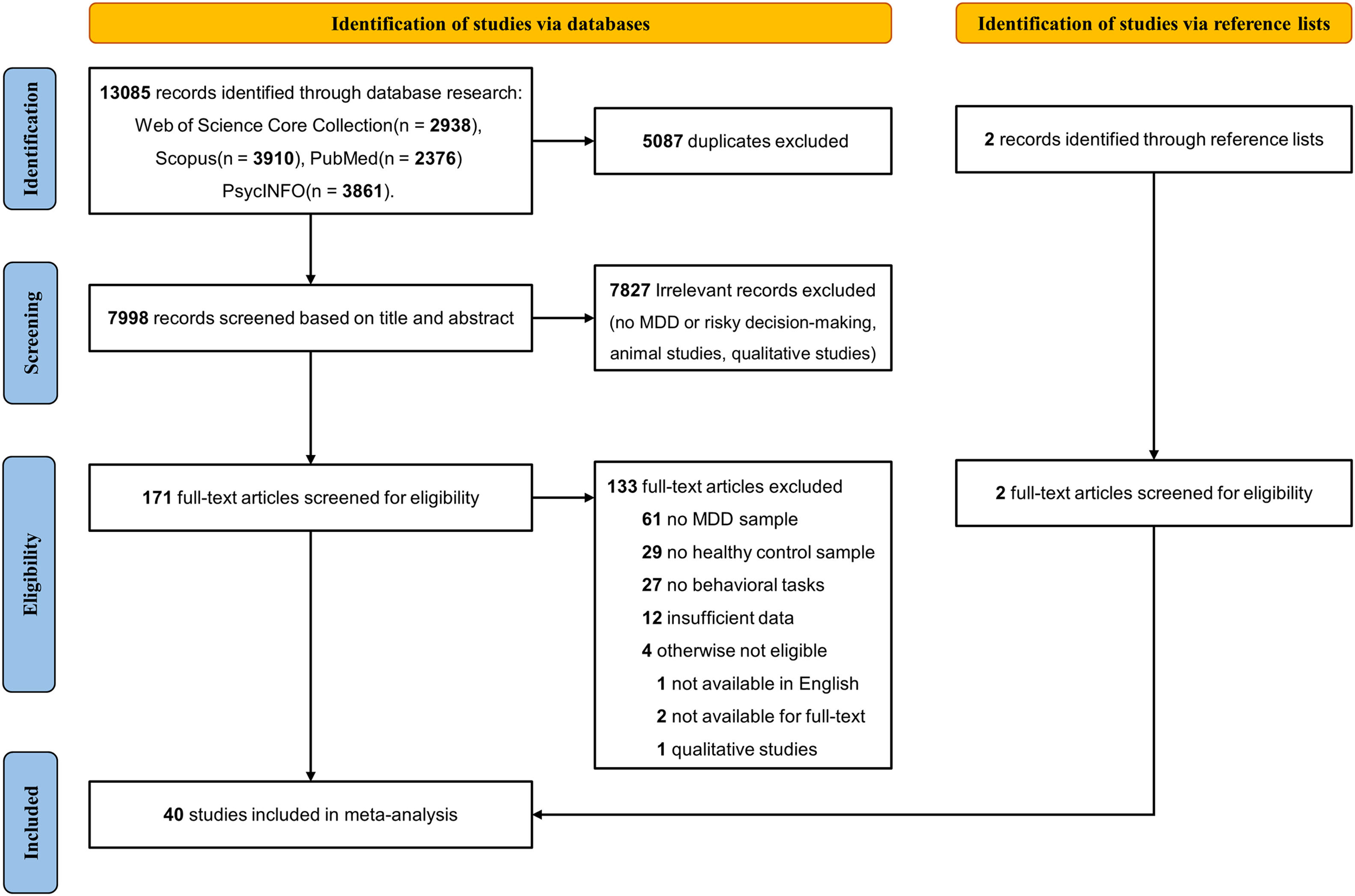
We independently screened the titles and abstracts twice to identify clearly eligible or ineligible studies. The same process was repeated for the full-text review. Any uncertainty was reconciled among the authors. Our systematic search identified 7998 articles, of which 7827 were excluded after the titles and abstracts were screened. After the full-text screening of the remaining 171 articles, we identified 40 eligible articles (see Fig. 1).
Data extractionTwo authors independently extracted the data from the same included articles, collecting the following information: (1) first author; (2) year of publication; (3) geographic regions; (4) type of diagnostic criteria and depression scale; (5) MDD phases and suicide attempts; (6) type of behavioral task; and (7) information of MDD and HCs group (mean and SD), including sample size, age, gender ratio, years of education, IQ, depression severity, and task score. In case of discrepancies in the extracted data, the authors would reexamine the article to confirm them. In addition, we aspire to mitigate instances of exclusion due to insufficient data for effect size calculation by contacting authors to obtain the required data. Fortunately, we received a response with the requisite data from Baek et al. (2017).
Statistical analysisWe conducted analyses using a metafor package in the R environment (Viechtbauer, 2010). We calculated effect sizes in terms of standardized mean differences (Hedges' g) between MDD patients and HCs on measures for risky decision-making. Therefore, a positive effect size indicated that MDD patients exhibited increased risk-seeking compared to HCs, and a negative value indicated the opposite regularity. If studies reported effects in other convertible statistics (e.g., means with SD), we transformed them into Hedges' g by the esc package in R (Lüdecke, 2019). Additionally, effect sizes that markedly deviate from others (i.e., outliers) may distort summary statistics and yield biased results (Kepes & Thomas, 2018; Lipsey & Wilson, 2001). Thus, we examined data for outliers, defined as effect sizes greater than or equal to 3 SD above or below the mean effect size, and excluded the effects from Pan et al. (2013). In such a case, 39 articles were included in the final meta-analysis.
Some studies contributed multiple effect sizes, such as studies that included multiple clinical groups or conditions of tasks, leading to intercorrelated effect sizes. Because using nested effect sizes violates an independence assumption for effect sizes, whereas not considering this dependency might bias the results, we adopted a three-level random-effects model with a restricted maximum likelihood (Assink & Wibbelink, 2016). It considered the dependence of effect sizes, resulting in maximum information and greater statistical power (Cheung, 2014). In our study, the three-level model examined three sources of variance: the sampling variance of the extracted effect sizes at Level 1, the variance between effect sizes within a study at Level 2, and the variance between studies at Level 3. In short, this model allows effect sizes to vary between participants (Level 1), outcomes within a study (i.e., different measures of risky decision-making, Level 2), and studies (Level 3).
Heterogeneity analysisWe assessed heterogeneity in effect sizes using Cochran's Q test and I2 statistics. Cochran's Q test distinguished whether the variability among the observed effect sizes was greater than the studies' sampling error alone. In contrast, the I2 statistic estimated the percentage of the variance caused by true heterogeneity rather than sampling error alone. Values of 25%, 50%, and 75% indicated low, moderate, and high degrees of heterogeneity, respectively.
Moderation analysisGiven the substantial heterogeneity in effect sizes, we conducted moderation analyses for sample and task characteristics. We conducted a multiple-moderator analysis that included all significant moderators to avoid multicollinearity issues due to interrelated moderators (Hox et al., 2010).
Sample characteristics. (a) Demographic variables. Most studies matched demographic variables between MDD patients and HCs, so we adopted demographics of MDD patients as moderators, including age, gender ratio, years of education, IQ, and region (1 = Europe; 2 = America; 3 = Asia). (b) Depression symptoms. We selected depression severity, MDD phases (0 = euthymic, 1 = acute), and suicide attempts (0 = no suicide ideations or attempts; 1 = only suicide ideations; 2 = exhibit suicide attempts) as moderators. Since depression scales had different items and severity level categories, we transformed depression scale scores into a standard metric (Snyder, 2013) (see Supplementary Table 2).
Task characteristics. (a) Task type. Except for IGT, BART, and CGT, the remaining tasks were all variants of risky choice tasks, including WOF, GDT, Probability discounting, and Lottery games (see Supplementary Table 3). Due to the few studies on the single risky choice task, we would consolidate these tasks under a category termed " Risky Choice Tasks" (RC tasks). Thus, we coded task type as 1 = IGT; 2 = BART; 3 = CGT; 4 = RC tasks. (b) The explicitness of the task. Researchers have distinguished tasks into decisions from description and experience based on whether the full information about probabilities and outcomes is provided (Hertwig et al., 2004). Following Dekkers et al. (2016), we adopted the explicitness of the task to classify these two types of tasks. Specifically, we coded as 0 = explicit task (i.e., decisions from description that the full information about probabilities and outcome is provided, as in GDT) and 1 = implicit task (i.e., decisions from experience that provide no explicit information about probabilities, and participant need to learn through feedback, as in IGT).
Publication biasTypically, studies with nonsignificant findings or small effect sizes have a decreased probability of being published, so we considered publication bias to avoid inflated estimates of the effect sizes of published studies. We calculated the risk of publication bias using funnel plots and Egger's regression test (Egger et al., 1997). In the presence of publication bias, the funnel plot becomes asymmetrical, and Egger's test has significant statistic values.
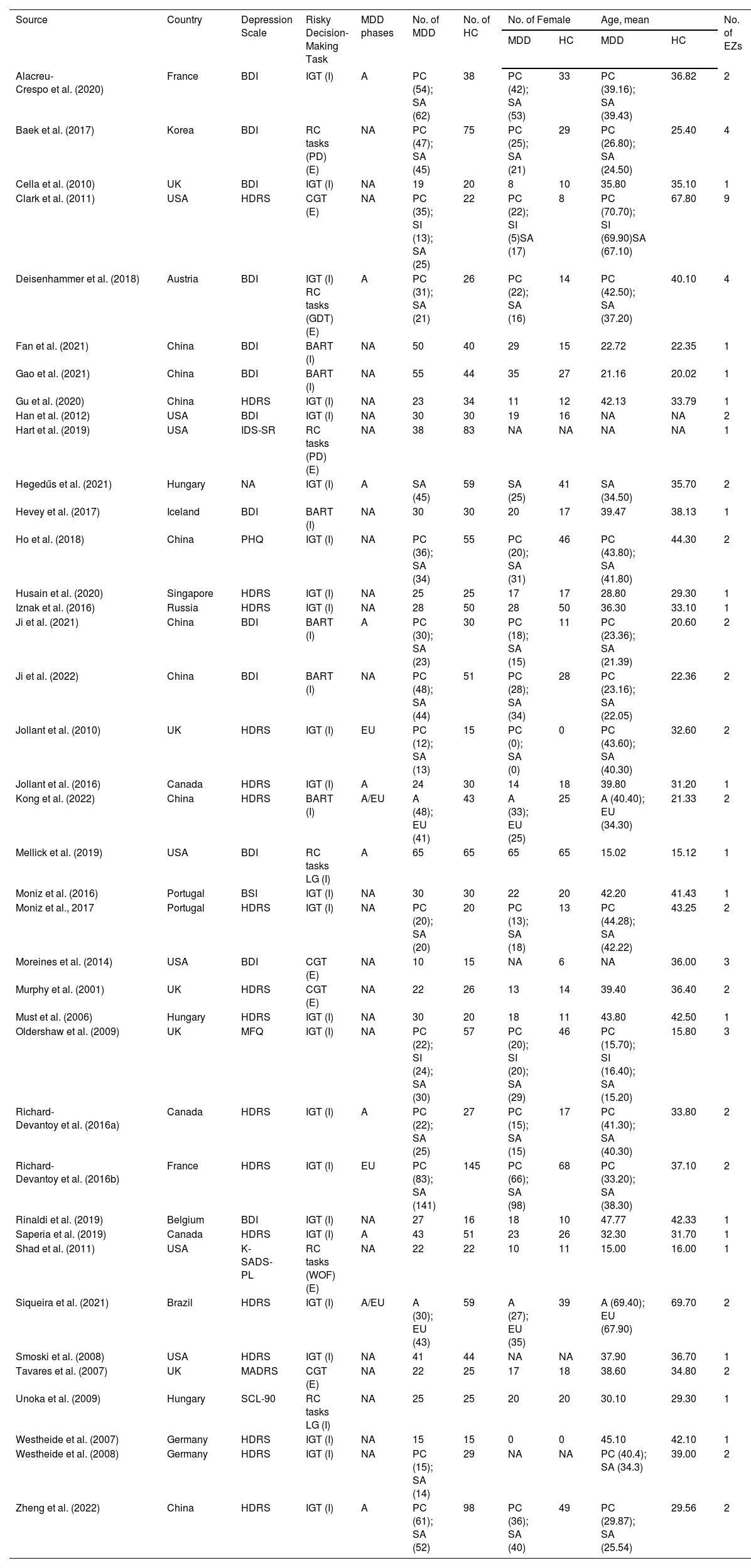
ResultsSample characteristicsThis meta-analysis included 39 eligible studies that compared risky decision-making between MDD patients (N = 1997; Mage = 34.77; 67.69 % female) and HCs (N = 1575; Mage = 33.06; 58.77% female), and 15 studies divided MDD patients with (N = 660; Mage = 34.76; 71.00% female) or without suicide attempts or ideations (N = 501; Mage = 35.52; 65.27% female) (see Table 1).
Characteristics of the included studies.
| Source | Country | Depression Scale | Risky Decision-Making Task | MDD phases | No. of MDD | No. of HC | No. of Female | Age, mean | No. of EZs | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MDD | HC | MDD | HC | ||||||||
| Alacreu-Crespo et al. (2020) | France | BDI | IGT (I) | A | PC (54); SA (62) | 38 | PC (42); SA (53) | 33 | PC (39.16); SA (39.43) | 36.82 | 2 |
| Baek et al. (2017) | Korea | BDI | RC tasks (PD) (E) | NA | PC (47); SA (45) | 75 | PC (25); SA (21) | 29 | PC (26.80); SA (24.50) | 25.40 | 4 |
| Cella et al. (2010) | UK | BDI | IGT (I) | NA | 19 | 20 | 8 | 10 | 35.80 | 35.10 | 1 |
| Clark et al. (2011) | USA | HDRS | CGT (E) | NA | PC (35); SI (13); SA (25) | 22 | PC (22); SI (5)SA (17) | 8 | PC (70.70); SI (69.90)SA (67.10) | 67.80 | 9 |
| Deisenhammer et al. (2018) | Austria | BDI | IGT (I) RC tasks (GDT) (E) | A | PC (31); SA (21) | 26 | PC (22); SA (16) | 14 | PC (42.50); SA (37.20) | 40.10 | 4 |
| Fan et al. (2021) | China | BDI | BART (I) | NA | 50 | 40 | 29 | 15 | 22.72 | 22.35 | 1 |
| Gao et al. (2021) | China | BDI | BART (I) | NA | 55 | 44 | 35 | 27 | 21.16 | 20.02 | 1 |
| Gu et al. (2020) | China | HDRS | IGT (I) | NA | 23 | 34 | 11 | 12 | 42.13 | 33.79 | 1 |
| Han et al. (2012) | USA | BDI | IGT (I) | NA | 30 | 30 | 19 | 16 | NA | NA | 2 |
| Hart et al. (2019) | USA | IDS-SR | RC tasks (PD) (E) | NA | 38 | 83 | NA | NA | NA | NA | 1 |
| Hegedűs et al. (2021) | Hungary | NA | IGT (I) | A | SA (45) | 59 | SA (25) | 41 | SA (34.50) | 35.70 | 2 |
| Hevey et al. (2017) | Iceland | BDI | BART (I) | NA | 30 | 30 | 20 | 17 | 39.47 | 38.13 | 1 |
| Ho et al. (2018) | China | PHQ | IGT (I) | NA | PC (36); SA (34) | 55 | PC (20); SA (31) | 46 | PC (43.80); SA (41.80) | 44.30 | 2 |
| Husain et al. (2020) | Singapore | HDRS | IGT (I) | NA | 25 | 25 | 17 | 17 | 28.80 | 29.30 | 1 |
| Iznak et al. (2016) | Russia | HDRS | IGT (I) | NA | 28 | 50 | 28 | 50 | 36.30 | 33.10 | 1 |
| Ji et al. (2021) | China | BDI | BART (I) | A | PC (30); SA (23) | 30 | PC (18); SA (15) | 11 | PC (23.36); SA (21.39) | 20.60 | 2 |
| Ji et al. (2022) | China | BDI | BART (I) | NA | PC (48); SA (44) | 51 | PC (28); SA (34) | 28 | PC (23.16); SA (22.05) | 22.36 | 2 |
| Jollant et al. (2010) | UK | HDRS | IGT (I) | EU | PC (12); SA (13) | 15 | PC (0); SA (0) | 0 | PC (43.60); SA (40.30) | 32.60 | 2 |
| Jollant et al. (2016) | Canada | HDRS | IGT (I) | A | 24 | 30 | 14 | 18 | 39.80 | 31.20 | 1 |
| Kong et al. (2022) | China | HDRS | BART (I) | A/EU | A (48); EU (41) | 43 | A (33); EU (25) | 25 | A (40.40); EU (34.30) | 21.33 | 2 |
| Mellick et al. (2019) | USA | BDI | RC tasks LG (I) | A | 65 | 65 | 65 | 65 | 15.02 | 15.12 | 1 |
| Moniz et al. (2016) | Portugal | BSI | IGT (I) | NA | 30 | 30 | 22 | 20 | 42.20 | 41.43 | 1 |
| Moniz et al., 2017 | Portugal | HDRS | IGT (I) | NA | PC (20); SA (20) | 20 | PC (13); SA (18) | 13 | PC (44.28); SA (42.22) | 43.25 | 2 |
| Moreines et al. (2014) | USA | BDI | CGT (E) | NA | 10 | 15 | NA | 6 | NA | 36.00 | 3 |
| Murphy et al. (2001) | UK | HDRS | CGT (E) | NA | 22 | 26 | 13 | 14 | 39.40 | 36.40 | 2 |
| Must et al. (2006) | Hungary | HDRS | IGT (I) | NA | 30 | 20 | 18 | 11 | 43.80 | 42.50 | 1 |
| Oldershaw et al. (2009) | UK | MFQ | IGT (I) | NA | PC (22); SI (24); SA (30) | 57 | PC (20); SI (20); SA (29) | 46 | PC (15.70); SI (16.40); SA (15.20) | 15.80 | 3 |
| Richard-Devantoy et al. (2016a) | Canada | HDRS | IGT (I) | A | PC (22); SA (25) | 27 | PC (15); SA (15) | 17 | PC (41.30); SA (40.30) | 33.80 | 2 |
| Richard-Devantoy et al. (2016b) | France | HDRS | IGT (I) | EU | PC (83); SA (141) | 145 | PC (66); SA (98) | 68 | PC (33.20); SA (38.30) | 37.10 | 2 |
| Rinaldi et al. (2019) | Belgium | BDI | IGT (I) | NA | 27 | 16 | 18 | 10 | 47.77 | 42.33 | 1 |
| Saperia et al. (2019) | Canada | HDRS | IGT (I) | A | 43 | 51 | 23 | 26 | 32.30 | 31.70 | 1 |
| Shad et al. (2011) | USA | K-SADS-PL | RC tasks (WOF) (E) | NA | 22 | 22 | 10 | 11 | 15.00 | 16.00 | 1 |
| Siqueira et al. (2021) | Brazil | HDRS | IGT (I) | A/EU | A (30); EU (43) | 59 | A (27); EU (35) | 39 | A (69.40); EU (67.90) | 69.70 | 2 |
| Smoski et al. (2008) | USA | HDRS | IGT (I) | NA | 41 | 44 | NA | NA | 37.90 | 36.70 | 1 |
| Tavares et al. (2007) | UK | MADRS | CGT (E) | NA | 22 | 25 | 17 | 18 | 38.60 | 34.80 | 2 |
| Unoka et al. (2009) | Hungary | SCL-90 | RC tasks LG (I) | NA | 25 | 25 | 20 | 20 | 30.10 | 29.30 | 1 |
| Westheide et al. (2007) | Germany | HDRS | IGT (I) | NA | 15 | 15 | 0 | 0 | 45.10 | 42.10 | 1 |
| Westheide et al. (2008) | Germany | HDRS | IGT (I) | NA | PC (15); SA (14) | 29 | NA | NA | PC (40.4); SA (34.3) | 39.00 | 2 |
| Zheng et al. (2022) | China | HDRS | IGT (I) | A | PC (61); SA (52) | 98 | PC (36); SA (40) | 49 | PC (29.87); SA (25.54) | 29.56 | 2 |
Abbreviations: NA, Not applicable; HDRS, Hamilton Depression Rating Scale; BDI, Beck Depression Inventory; BSI, Brief Symptom Inventory; IDS, Inventory of Depressive Symptomatology; MADRS, Montgomery–Asberg Depression Rating Scale; MFQ, Mood and Feelings Questionnaire; PHQ, Patient Health Questionnaire; SCL-90, Symptom Checklist 90; IGT, Iowa Gambling Task; BART, Balloon Analogue Risk Task; CGT, Cambridge Gambling Task; RC tasks, Risky Choice Task (GDT, Game of Dice Task; PD, Probability Discounting; WOF, Wheel of Fortune); LG, Lottery Game. E, Explicit task; I, Implicit task; EU, Euthymic; A, Acute; SA, patients with suicide attempts; SI, patients with suicide ideations; PC, patients without suicide ideations and attempts.
The included studies collected data in Europe (46.15%; n = 18), America (28.21%; n = 11), and Asia (25.64%; n = 10). Thirty-one studies (79.48%) were published in or after 2010. All studies were cross-sectional. Regarding the depression scales used, most studies used the Hamilton Depression Rating Scale (HDRS) (46.15%; n = 18) and the Beck Depression Inventory (BDI) (33.33%; n = 13). Regarding the behavioral tasks, 24 studies used the IGT, 4 used the CGT, 6 used the BART, and the remaining used RC tasks.
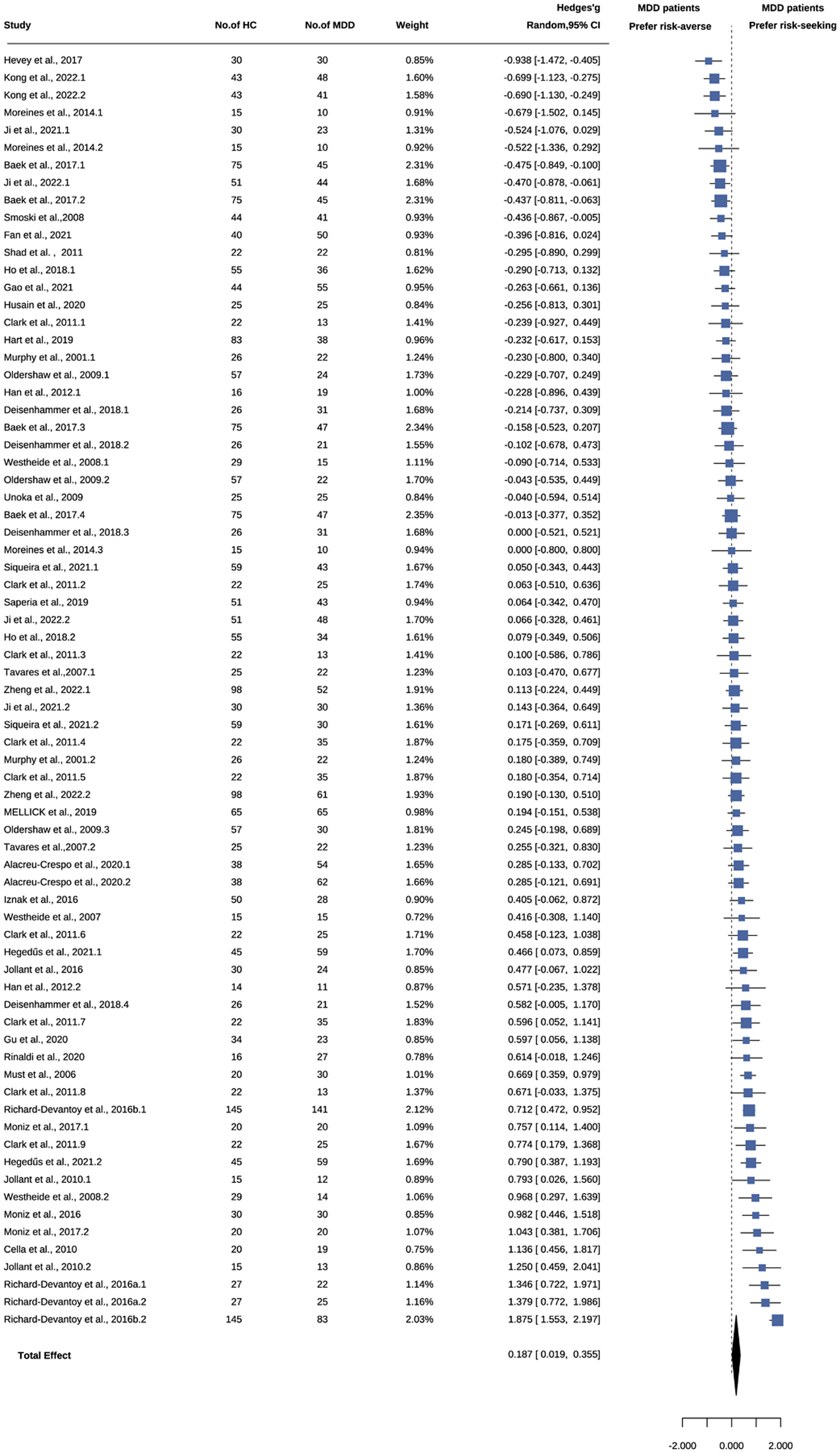
Overall effects on risky decision-making: MDD patients vs. HCsThe overall effect size was small but significant (k = 73; Hedges' g = 0.187, 95% CI [0.019, 0.355]; t = 2.21; p = .030), indicating that MDD patients exhibited more risk-seeking than HCs (see Fig. 2). Overall heterogeneity was substantial, QE (72) =380.26, p <.001, and I2 = 81.10%. Follow-up analysis found that the variances at the sampling, within-study and between-study levels were 18.90%, 18.43%, and 62.67%, respectively, suggesting a necessity to explore potential moderators.
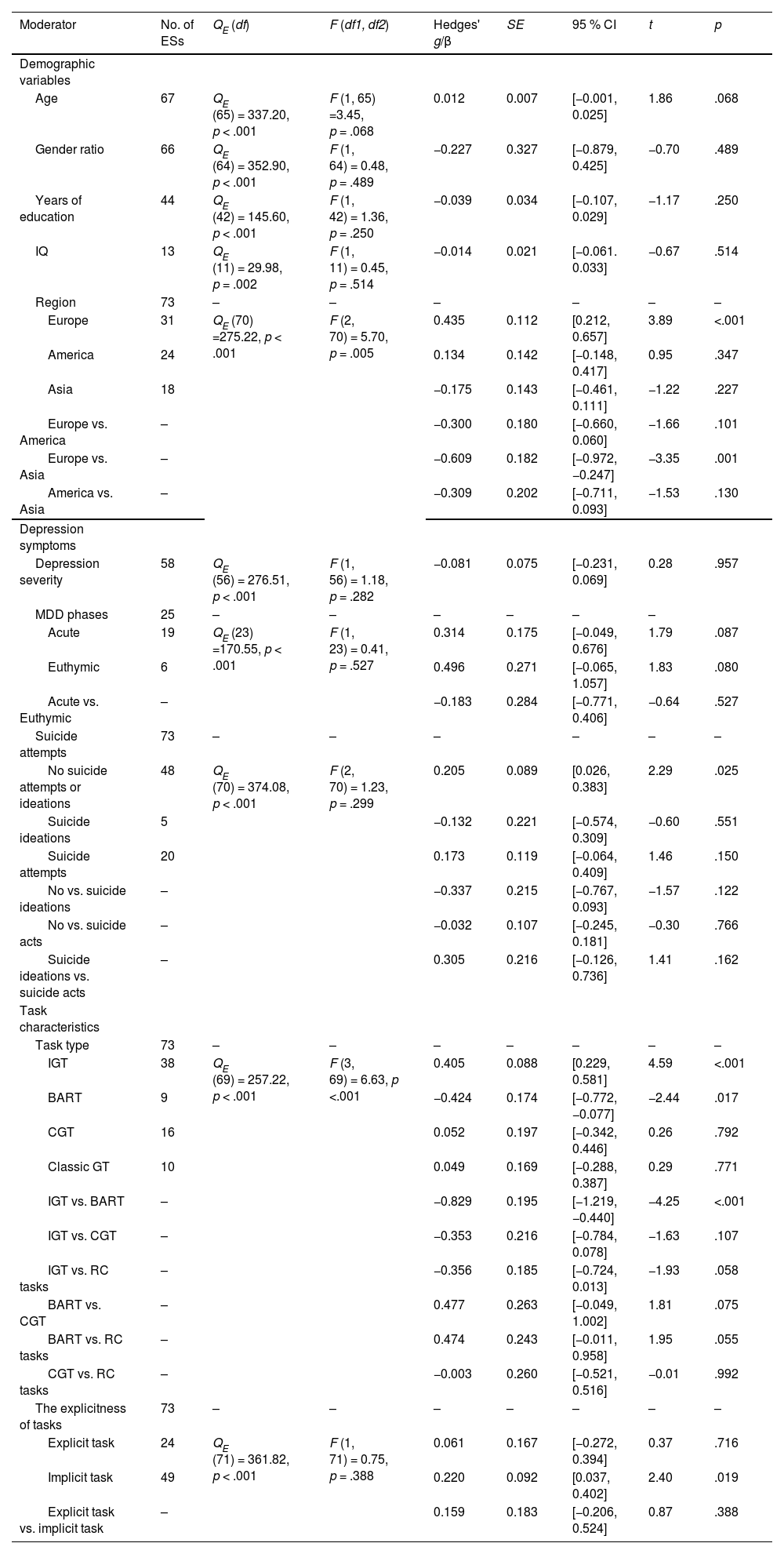
Moderator analysisConsidering the high level of heterogeneity, we assessed potential moderators, namely, sample and task characteristics (see Table 2). For sample characteristics, region (QE (70) = 275.22, p <.001; F (2, 70) = 5.70, p = .005) and age (β = 0.012; QE (65) = 337.20, p < .001; F (1, 65) = 3.45, p = .068) were (marginally) significant. None of the other sample characteristics, including gender ratio, years of education, IQ, MDD phases, depression severity, or suicide attempts, had significant moderating effects. Regarding task characteristics, task type was significant (QE (69) = 257.22, p <.001; F (3, 69) = 6.63, p <.001), but the explicitness of the task was not.
Results of the moderation analysis regarding the associations between MDD and risky decision-making.
Abbreviations: IGT, Iowa gambling task; BART, Balloon analogue risk task; CGT, Cambridge gambling task; RC tasks, Risky choice task.
We conducted a follow-up comparison based on the significant moderators. Pertaining to the region, only effect sizes for European studies were significant (k = 31; Hedges' g = 0.435, 95% CI [0.212, 0.657]; t = 3.89; p <.001) and significantly larger than Asian Studies (β = −0.609, 95% CI [−0.972, −0.247], t = −3.35; p = .001). The statistical power of effect sizes in studies conducted in Europe, the Americas, and Asia were 100%, 28.4%, and 52.6%, respectively (see Supplementary Table 4 and Supplementary Figure 1).
Regarding the task type, effect sizes in IGT studies were significant (k = 38; Hedges' g = 0.405, 95 % CI [0.229, 0.581]; t = 4.59; p < .001) and marginally significantly larger than those in RC tasks studies (β = −0.356, 95% CI [−0.724, 0.013], t = −1.93; p = .058). Likewise, effect sizes in BART studies were significant but negative (k = 9; Hedges' g = −0.424, 95% CI [−0.772, −0.077]; t = −2.44; p = .017) and (marginally) significantly smaller than studies using the other three tasks (IGT: β = 0.829, 95% CI [0.440, 1.219], t = 4.25; p <.001; CGT: β = 0.477, 95% CI [−0.049, 1.002], t = 1.81; p = .075; RC tasks: β = 0.474, 95% CI [−0.011, 0.958], t = 1.95; p = .055). The statistical power of effect sizes in studies employing IGT, BART, CGT, and RC tasks were as follows: 100%, 94.4%, 5.75%, and 7.13%, respectively (see Supplementary Table 5 and Supplementary Figure 2).
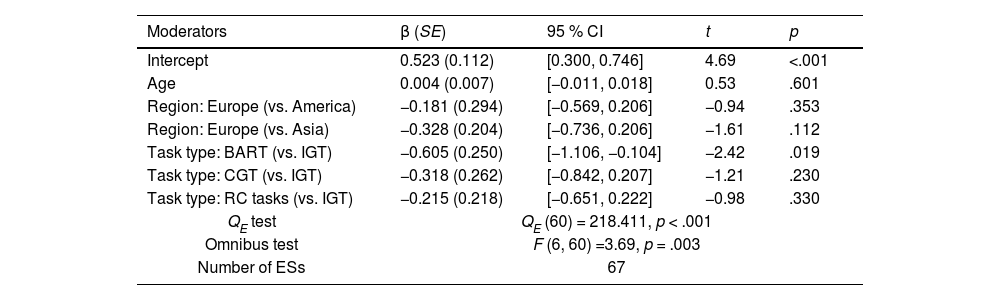
Multiple-moderator modelWe conducted a multiple-moderator analysis with significant moderators (see Table 3). An omnibus test showed a significant result, F (6, 60) = 3.69, p = .003, suggesting that at least one regression coefficient of the moderators significantly deviated from zero. It indicated that task type of IGT (vs. BART) (βIGT (vs. BART) = −0.605, 95% CI [−1.106, −0.104], t = −2.42; p = .019) had unique moderating effects on the association between MDD and risky decision-making. We also observed variations in the mean age of MDD patients (F (2, 33) = 3.31, p = .049) and task types used (χ2 (6, N = 40) = 15.60, p = .016) among different regions (see Supplementary Table 6 and Supplementary Figure 3). Consequently, alongside the continued significant effects of task type in the multiple-moderator model, we speculated that the moderating effect of region might be attributed to task type variations across regions.
Moderation analysis: Results from the multiple-moderator model.
Abbreviations: IGT, Iowa gambling task; BART, Balloon analogue risk task; CGT, Cambridge gambling task; RC tasks, Risky choice task.
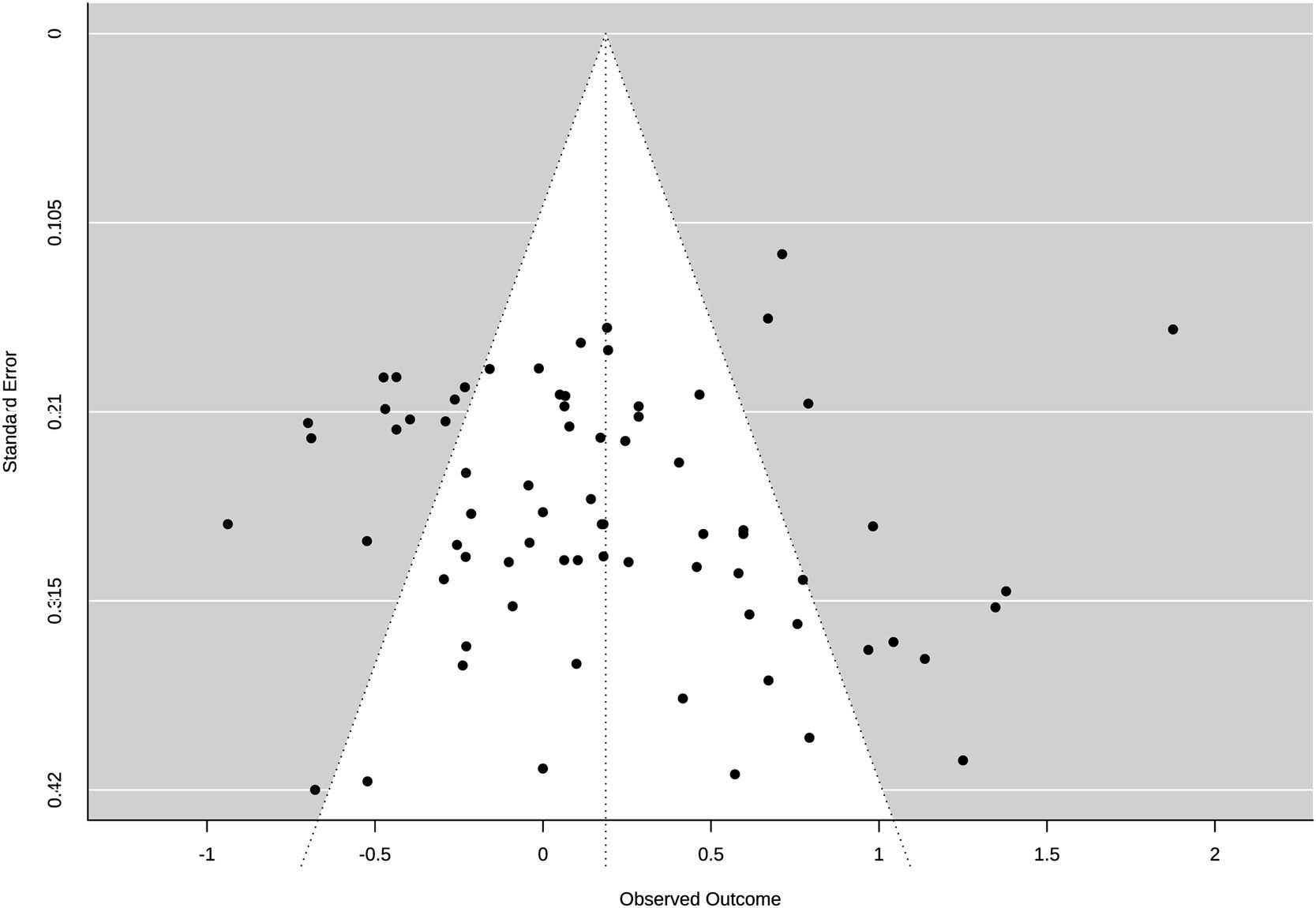
We inspected a funnel plot (see Fig. 3) and Egger's regression test to statistically check publication bias. Egger's regression test results showed no significant asymmetry in the funnel plot (z = 1.17; p = .241), suggesting no significant publication bias for the above findings.
DiscussionThe current three-level meta-analysis quantified risky decision-making differences between MDD patients and HCs. Across 39 studies, we found that MDD patients exhibited significantly greater risk-seeking than HCs but with a small effect size (Hedges' g = 0.187, p = .030). Considering the high heterogeneity observed, we speculated that this small effect size could be partly attributed to the influence of moderators. In such a case, we tested whether sample and task characteristics moderated the association between MDD and risky decision-making. The findings revealed that task type and region exerted significant moderating effects, while age showed a marginally significant effect. Besides, the moderating effects of other sample characteristics and the explicitness of tasks were not significant.
The result that MDD patients showed increased risk-seeking was consistent with some prior studies (e.g., Cell et al., 2010; Hegedűs et al., 2021) and supported the notion that MDD patients frequently engage in daily risky behaviors. Considering the small effect size of this phenomenon, future studies need to investigate and verify its robustness. Moreover, we tried to provide speculations for this phenomenon. First, the Emotion Maintenance Hypothesis (Isen & Partick, 1983) proposes that individuals in negative emotional states may take risks to improve their emotions. As such, MDD patients might exhibit more risky behaviors to relieve their depression. Moreover, MDD patients may have anhedonia, resulting in a decreased response to stimulation (Treadway & Zald, 2011), which may cause them to seek stronger stimulation through high-risk activities to arouse positive emotions. Additionally, MDD patients often experience cognitive impairment, manifested as decreased processing speed and executive function (Rock et al., 2014), which may affect their decision-making abilities and result in inappropriate risk preferences. The above speculations need to be tested in future research.
The moderation effect of sample characteristicsRegarding demographics, we found that age exhibited a marginally significant moderating effect. Specifically, as age increased, MDD patients exhibited a stronger preference trend for risk-seeking than HCs. When individuals get older, their cognitive abilities may decline gradually (Hartshorne & Germine, 2015), which reduces their capacity to evaluate risks or rewards accurately and optimize decision-making strategies, resulting in greater risk-seeking. MDD might further impair cognitive abilities and worsen cognitive decline (da Silva et al., 2013), especially in older adults (John et al., 2019). Thus, MDD patients exhibit greater risk-seeking than HCs with age due to the widening gap in cognitive ability. Given the marginal significance of age's moderating effect, additional research would be needed to retest the robustness of this conclusion.
Besides, this study showed a surprising moderating effect of the region. Effect sizes for European studies were significant and larger than that for Asian studies. These results may be related to a statistical power problem or differences in age distribution or task selection across regions. We further tested these two speculations. On the one hand, we found that the statistical powers of effect sizes in American and Asian studies were small, which makes it difficult to detect significance based on the current effect sizes. If the number of studies in the Americas and Asia increased in the future, the statistical powers would improve. On the other hand, in different regions, the mean age of MDD patients and task type used had significant differences. Specifically, European and American patients' mean age was significantly older than that of Asian patients. Additionally, European and American studies predominantly employ IGT, whereas Asian studies exhibit a more equitable distribution of task types, with a relatively higher usage of BART. In this case, the moderating effect of region might be related to the age distribution and task type used among regions. Considering that only task type was significant in the multiple-moderator model, we inferred that the moderating effect of the region could be explained by task type variations across regions. However, we still cannot rule out the possibility that impaired risky decision-making in MDD varies across cultures. Thus, we should accumulate studies using a balanced number of task types in different regions to verify the current findings.
Regarding depression symptoms, this study did not show any significant moderators. However, it did reveal that MDD patients in both acute and euthymic phases exhibited increased risk-seeking compared to HCs with marginally significant effect sizes. This finding suggests that changes in risk preference in MDD patients might be a stable characteristic no matter the MDD phases, but further research is needed to test its robustness. Moreover, we encoded the mean depression scores of the MDD group from 0 (euthymic) to 3 (severe or very severe) and tested the moderating effect of this depression severity. However, the results found no significant moderating effects, persisting same even upon stratifying depression severity into two groups (i.e., the above codes 0 or 1 were combined into a "euthymic and mild depression" group, while codes 2 or 3 were combined into a " moderate and severe depression " group). While our study's existing data did not show the effect of depression severity on risky decision-making, it did not imply the absence of such an effect. On the one hand, it may be attributed to an unbalanced number of effect sizes across different levels of depression severity. On the other hand, relying solely on mean scores cannot adequately reflect the entire spectrum of patients within the MDD group. Therefore, to achieve a more precise understanding of the depression severity effect, it is necessary to continually accumulate studies on the correlation between depression severity and risky decision-making. Additionally, we found that MDD patients without suicide attempts exhibited increased risk-seeking; but this was not found in patients with suicide attempts, which is inconsistent with previous meta-analyses (e.g., Perrian et al., 2021; Richard-Devantoy et al., 2016b). This may be due to the small number of suicide studies, resulting in low statistical power to detect differences. Nevertheless, it is worth noting that previous meta-analyses primarily used IGT as a measure, while this study used diverse tasks. Thus, considering task specificity, this study may exhibit different results from previous studies. If only focusing on IGT studies, we did find that MDD patients with suicide attempts showed increased risk-seeking compared to HCs (Hedges' g = 0.470, p = .004).
The moderation effect of task characteristicsRegarding task characteristics, one exciting finding was the moderating effect of task type. Specifically, the effect sizes in IGT and BART studies were significant but contradictory; that is, MDD patients exhibited increased risk-seeking in IGT but increased risk-averse in BART. These findings indicated that using different tasks may result in a lack of consensus on risky decision-making in MDD.
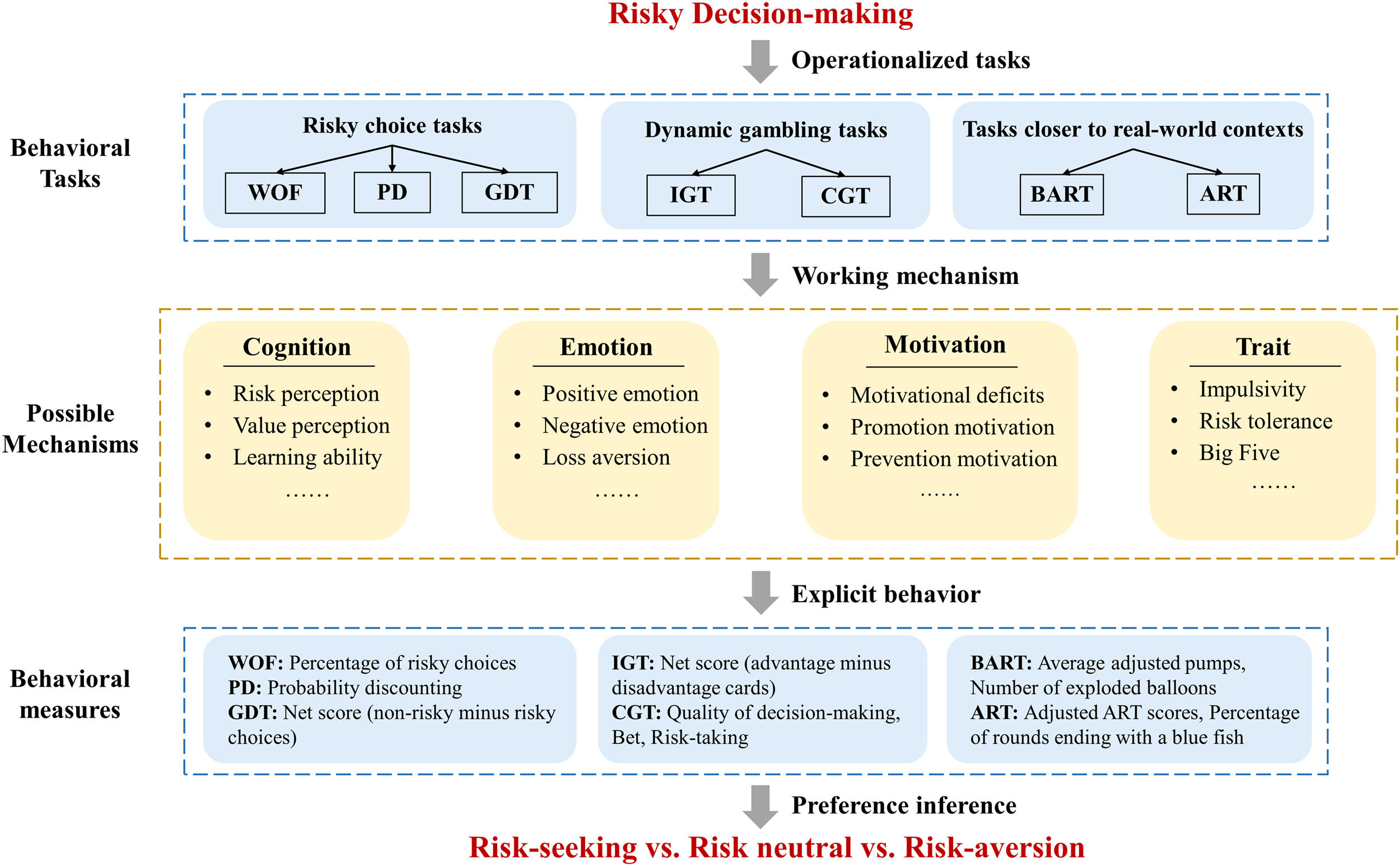
The first possible explanation for the inconsistent risk preferences is operationalization specificity, which means the construct of risky decision-making was operationalized into different tasks (see Fig. 4). Buelow and Blaine (2015) found overlapping and unique components within the construct of risky decision-making across various tasks. Consequently, these unique components within the construct may cause inconsistency in risk preference. It implicated the necessity of utilizing multiple measures to comprehensively understand risky decision-making in MDD patients, as no single risky decision-making task fully assesses the construct.
A Tentative framework for risk preference inferring in different risk decision tasks.
(Abbreviations: WOF, Wheel of fortune; PD, Probability discounting; GDT, Game of dice task; IGT, Iowa gambling task; BART, Balloon analogue risk task; CGT, Cambridge gambling task; ART, Angling risk tasks).
The second possible explanation is mechanism specificity, by which MDD patients vary in the extent and direction of various mechanisms changed in risky decision-making (see Fig. 4). Shared and unique mechanisms of risky decision-making underlie different tasks (Bishara et al., 2009). For example, in IGT, cognitive (e.g., working memory and learning ability; Toplak et al., 2010) and emotional factors (e.g., somatic marker hypothesis; Bechara et al., 1994) are likely to serve as the main working mechanisms, while in BART, emotional (e.g., positive or negative emotions; Tao et al., 2023) and motivational factors (e.g., motivational deficits; Culbreth et al., 2018) are considered the primary working mechanisms. Contradictory effect sizes in IGT and BART studies may be attributed to distinct impaired mechanisms of risky decision-making in these two tasks. Similarly, this study revealed that MDD patients only showed increased risk-seeking in implicit tasks, indicating that the changes in risk preference in MDD may be related to mechanisms underlying implicit tasks. Thus, future studies are necessary to refine our understanding of MDD and its mechanisms of risky decision-making using various tasks.
However, even the same impairment in different risk decision tasks may lead to differing explicit behaviors. For example, the impaired mechanism was the inability to recognize tasks' optimal strategies, which may lead to different explicit behaviors in IGT and BART. In IGT, individuals need to learn that disadvantageous cards result in long-term losses and should select fewer disadvantageous cards (i.e., the optimal strategy is less risk-seeking) to get better performance. If they fail to do so, they will display increased risk-seeking (Bechara et al., 1994). In contrast, in BART, individuals need to balance the trade-off between risks and rewards by adequate pumps for unexploded balloons (i.e., the optimal strategy is appropriate risk-seeking). They might display increased risk aversion if they fail to do so (Lejuez, 2002). Therefore, MDD patients who cannot identify the optimal strategy can be reasonably considered to exhibit different risk preferences in these two tasks. Therefore, future studies on the relationship between MDD and risky decision-making should not only concentrate on explicit behaviors but also consider the underlying mechanisms.
In addition, different behavioral measures may lead to inconsistent preference inference in risky decision-making, which means measure specificity. It mainly occurs when studies adopt the same task (i.e., characterized by identical operationalizations and working mechanisms) but use different behavioral measures. Although it has little to do with the task type's moderating effect, future studies could pay some attention to the measure specificity.
Implications for future research and clinical practiceFirst, our study provides initial evidence of increased risk-seeking among MDD patients, but this effect was affected by various factors, with instances where the effect even reversed. Moreover, there is a lack of studies on the psychological mechanism underlying how MDD affects risky decision-making. Hence, it is necessary to accumulate more studies to explore this phenomenon and the mechanisms underlying it.
Second, we should deliberately consider the moderating effect of task type and attach importance to the cross-paradigm consistency of the relationship between MDD and risky decision-making. Most studies have judged whether MDD patients exhibited increased risk-seeking or risk aversion based on the results of a single task. However, operationalization specificity, mechanism specificity, and measure specificity, as shown above, may affect the robustness of these judgments. Thus, future studies need various tasks and measures to draw a more robust conclusion across paradigms, especially clarifying the exact meaning of complex measures in tasks such as the net score in IGT. More importantly, the effect of task type indicated that the binary conceptualization of increased risk-seeking or risk-aversion might not be the best way to characterize risky decision-making in MDD and may even lead to inconsistent findings. In this way, we should avoid overgeneralized interpretations of task-specific risk-seeking/aversion and explore underlying impairments that generate these seemingly different explicit behaviors.
Third, based on the existing literature, there is no compelling evidence to suggest that impaired risky decision-making is exclusive to MDD. However, it could be considered a noteworthy behavioral characteristic in clinical management and psycho-education. In light of this, clinicians should maintain vigilance about the performance of risky decision-making in MDD patients, regardless of the depression severity. They should be attentive to signs of decision-making impairment and respond promptly when symptoms manifest. Additionally, it is crucial to provide MDD patients and their families with information about these impairments and strategies for coping.
Finally, this study suggests that intervening in risky behaviors may offer a possible approach to ameliorating MDD symptoms. Studies have found that mindfulness training has positive effects on decision-making (Du et al., 2023; Forman et al., 2016) and reduces risky behaviors such as gambling (Lakey et al., 2007) and dangerous driving (Baltruschat et al., 2021). Additionally, self-regulatory interventions, such as goal setting and personalized feedback, have also effectively reduced risky behaviors (Protogerou et al., 2020). Thus, these interventions targeting to decrease risk-seeking may offer a promising way to improve MDD symptoms.
LimitationsThe present study had some limitations. First, we could not assess the association of some potential sample characteristics with group differences due to the limited data collection in the original samples. For example, most studies did not provide data on drug use and comorbidities in MDD patients. Second, this analysis primarily focused on risky decision-making in the financial domain and found a small significant effect size. However, risk-taking propensity has been domain-specific and varies across domains such as health and social (Mishra, 2014). Therefore, future studies need to explore whether and how MDD patients' risky decision-making changes in other domains. Finally, this was a cross-sectional data meta-analysis; hence, we could not determine the causal associations between MDD and risky decision-making.
ConclusionConducting a three-level meta-analysis of 39 studies, we found that MDD was associated with risky decision-making impairments and varied extents across age, regions, and task types. These findings answered whether and how MDD patients' risky decision-making changes relative to HCs and provided possible practical significance for clinical management and psycho-education in depression based on risky decision-making.
ContributorsAll authors designed the study and wrote the protocol. Lu, Zhao, and Wei conducted literature searches and coded the data. Lu conducted the statistical analysis and wrote the first draft of the manuscript. Professor He supervised the project, obtained funding, and substantially revised the manuscript. All authors contributed to and have approved the final manuscript.
Data availabilityThe data and the analysis scripts used for this article can be also accessed at this OSF page: https://osf.io/t6q4u/?view_only=57e563f2ca104ebfabc416b3cf6ced4c
FundingThis study was supported by the National Natural Science Foundation of China (72071178). The funding source had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
References marked with an asterisk indicate studies included in the meta-analysis.