The ability to drive after a stroke has been recognised by many authors as a sign of independence and it is closely associated with proper social reintegration. However, it remains unclear how the driving ability of an individual who has suffered a stroke should be evaluated, and by whom. Neurorehabilitation can produce improvements in patients who have suffered a stroke, and patients may therefore be able to resume driving at the end of an appropriate neurorehabilitation programme.
The aim of this article is to present a literature review in order to highlight current evidence regarding methods for assessing driving ability and therapeutic methods applied in order to recover a patient's ability to drive.
DevelopmentA literature search was performed in different databases for the period between 1993 and 2011. Studies were analysed individually based on methods for assessing driving ability and neurorehabilitation measures.
ConclusionsIf there are any doubts regarding stroke patients’ ability to drive, patients should be assessed appropriately. The proper way to assess these patients according to the literature is by employing a multidisciplinary evaluation to determine who is able to take a road test. Neurorehabilitation exercises currently in use may be able to improve driving ability in stroke patients.
La habilidad para conducir después de un ictus ha sido reconocida por muchos autores como un indicador de independencia y se asocia de forma significativa con una reintegración social adecuada. Sin embargo, no queda claro quién y como debe valorarse la capacidad de conducción de un individuo que ha sufrido un ictus. El proceso Neurorrehabilitador es capaz de obtener mejorías en los pacientes que han sufrido un ictus y por lo tanto un paciente puede volver a estar capacitado para conducir tras un tratamiento Neurorrehabilitador adecuado.
El objetivo de este artículo es realizar una revisión de la literatura, con el fin de poner de manifiesto la evidencia actual respecto a los métodos de evaluación de la capacidad para conducir y de aquellas intervenciones llevadas a cabo para recuperar la capacidad de conducir.
DesarrolloSe llevó a cabo una búsqueda de la literatura de diferentes bases de datos entre los años 1993 y 2011. Se analizaron de forma individual los estudios realizados en base a los métodos de evaluación de la capacidad de conducir y de intervención neurorrehabilitadora.
ConclusionesSe debe valorar de forma apropiada a todos los pacientes con un ictus en los que existen dudas sobre su capacidad de conducir. La forma adecuada de valorar estos pacientes según la literatura es mediante una valoración multidisciplinar que determine quien esta capacitado para someterse a un test en carretera. Los ejercicios de Neurorrehabilitación existentes pueden mejorar la capacidad de conducir de los pacientes con ictus.
Stroke is a catastrophic illness. In developed countries, it is listed as one of the main causes of death and the leading cause of disability. In addition to its considerable repercussions on patients and their families,1 it also has an elevated social impact.2 Direct and indirect costs of stroke account for at least 3% of all healthcare costs in a developed country.3 Future projections are not very encouraging. The ageing population is associated with a higher incidence of stroke, while advances in the understanding of pathophysiology in brain damage and the development of new diagnostic and therapeutic techniques are associated with rising stroke prevalence. Given this panorama, neurorehabilitation units are crucial for minimising stroke sequelae.4
Strokes have a negative effect on patients’ social activities and quality of life.5 The ability to drive after a stroke has been recognised by many authors as an indicator of independence, and it demonstrates a strong association with good social reintegration. In particular, it is significantly associated with appropriate social reintegration at one year after stroke.6 Nevertheless, it remains unclear how ability to drive should be evaluated in a stroke patient, and who should be entrusted with the task. The difficulty resides in the complexity of the act of driving, which requires full function of multiple systems that may be damaged totally or partially, and permanently or temporarily, in stroke patients. Some of the most important systems are visual function, motor function, and cognitive ability (including executive functions, response time, praxis and knowledge, decision-making, attention, planning, etc.).
Patients who have experienced stroke have greater deficiencies when driving than stroke-free subjects.7 Stroke patients older than 65 years have a higher risk of being involved in accidents while driving, regardless of the medication they take, compared to patients with other chronic diseases (cancer, diabetes, cognitive impairment, glaucoma, other).8 This being the case, it is of vital importance to determine which individuals with a history of stroke should not drive, especially when it has been shown that stroke patients and their families tend to overestimate their driving ability.9
In practice, many patients who have experienced stroke resume driving without medical advice or evaluation,10 while others choose not to drive again for safety reasons.5,11,12
The purpose of this article is to present a literature review with current evidence on methods for evaluating driving ability and the interventions that have been performed so that patients can recover their abilities.
ProcedureUsing a variety of databases (CINAHL, EMBASE, MEDLINE and PSYCHINFO), we performed a literature search for the years 1980–2011. We selected published studies on assessing driving ability in stroke patients, or studies analysing interventions designed to improve patients’ driving abilities. Those studies not detected by our original literature search, but cited in review articles, meta-analyses, or systematic reviews, were also included.
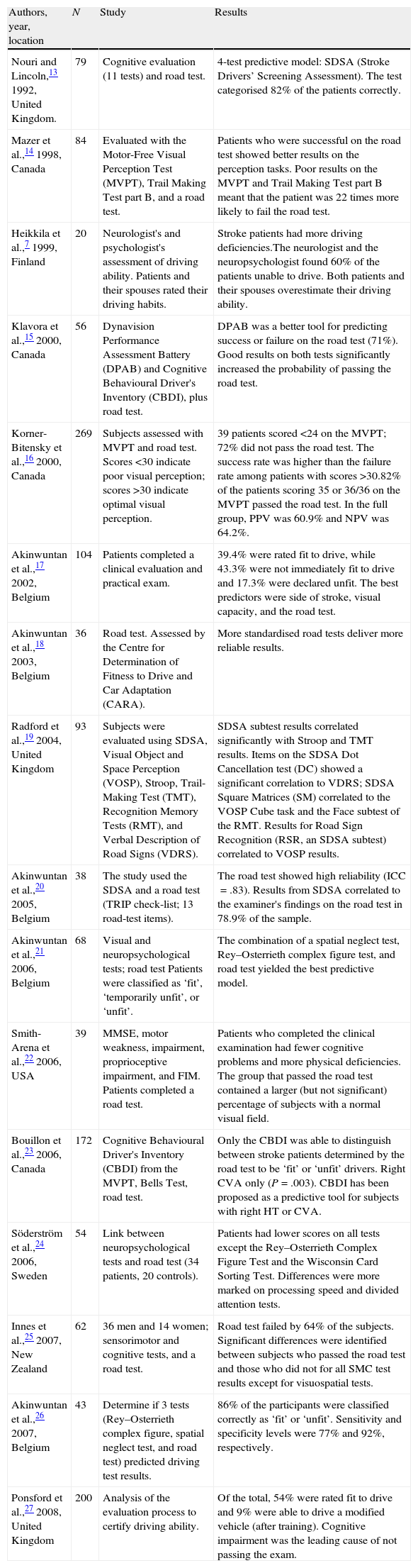
Evaluating driving abilityIn some countries, doctors are responsible for assessing a patient's ability to drive after a stroke, but few clinical guidelines indicate how this ability should be measured. Table 1 provides a summary of studies examining how driving ability is evaluated.
Studies addressing driving ability after a stroke.
| Authors, year, location | N | Study | Results |
| Nouri and Lincoln,13 1992, United Kingdom. | 79 | Cognitive evaluation (11 tests) and road test. | 4-test predictive model: SDSA (Stroke Drivers’ Screening Assessment). The test categorised 82% of the patients correctly. |
| Mazer et al.,14 1998, Canada | 84 | Evaluated with the Motor-Free Visual Perception Test (MVPT), Trail Making Test part B, and a road test. | Patients who were successful on the road test showed better results on the perception tasks. Poor results on the MVPT and Trail Making Test part B meant that the patient was 22 times more likely to fail the road test. |
| Heikkila et al.,7 1999, Finland | 20 | Neurologist's and psychologist's assessment of driving ability. Patients and their spouses rated their driving habits. | Stroke patients had more driving deficiencies.The neurologist and the neuropsychologist found 60% of the patients unable to drive. Both patients and their spouses overestimate their driving ability. |
| Klavora et al.,15 2000, Canada | 56 | Dynavision Performance Assessment Battery (DPAB) and Cognitive Behavioural Driver's Inventory (CBDI), plus road test. | DPAB was a better tool for predicting success or failure on the road test (71%). Good results on both tests significantly increased the probability of passing the road test. |
| Korner-Bitensky et al.,16 2000, Canada | 269 | Subjects assessed with MVPT and road test. Scores <30 indicate poor visual perception; scores >30 indicate optimal visual perception. | 39 patients scored <24 on the MVPT; 72% did not pass the road test. The success rate was higher than the failure rate among patients with scores >30.82% of the patients scoring 35 or 36/36 on the MVPT passed the road test. In the full group, PPV was 60.9% and NPV was 64.2%. |
| Akinwuntan et al.,17 2002, Belgium | 104 | Patients completed a clinical evaluation and practical exam. | 39.4% were rated fit to drive, while 43.3% were not immediately fit to drive and 17.3% were declared unfit. The best predictors were side of stroke, visual capacity, and the road test. |
| Akinwuntan et al.,18 2003, Belgium | 36 | Road test. Assessed by the Centre for Determination of Fitness to Drive and Car Adaptation (CARA). | More standardised road tests deliver more reliable results. |
| Radford et al.,19 2004, United Kingdom | 93 | Subjects were evaluated using SDSA, Visual Object and Space Perception (VOSP), Stroop, Trail-Making Test (TMT), Recognition Memory Tests (RMT), and Verbal Description of Road Signs (VDRS). | SDSA subtest results correlated significantly with Stroop and TMT results. Items on the SDSA Dot Cancellation test (DC) showed a significant correlation to VDRS; SDSA Square Matrices (SM) correlated to the VOSP Cube task and the Face subtest of the RMT. Results for Road Sign Recognition (RSR, an SDSA subtest) correlated to VOSP results. |
| Akinwuntan et al.,20 2005, Belgium | 38 | The study used the SDSA and a road test (TRIP check-list; 13 road-test items). | The road test showed high reliability (ICC=.83). Results from SDSA correlated to the examiner's findings on the road test in 78.9% of the sample. |
| Akinwuntan et al.,21 2006, Belgium | 68 | Visual and neuropsychological tests; road test Patients were classified as ‘fit’, ‘temporarily unfit’, or ‘unfit’. | The combination of a spatial neglect test, Rey–Osterrieth complex figure test, and road test yielded the best predictive model. |
| Smith-Arena et al.,22 2006, USA | 39 | MMSE, motor weakness, impairment, proprioceptive impairment, and FIM. Patients completed a road test. | Patients who completed the clinical examination had fewer cognitive problems and more physical deficiencies. The group that passed the road test contained a larger (but not significant) percentage of subjects with a normal visual field. |
| Bouillon et al.,23 2006, Canada | 172 | Cognitive Behavioural Driver's Inventory (CBDI) from the MVPT, Bells Test, road test. | Only the CBDI was able to distinguish between stroke patients determined by the road test to be ‘fit’ or ‘unfit’ drivers. Right CVA only (P=.003). CBDI has been proposed as a predictive tool for subjects with right HT or CVA. |
| Söderström et al.,24 2006, Sweden | 54 | Link between neuropsychological tests and road test (34 patients, 20 controls). | Patients had lower scores on all tests except the Rey–Osterrieth Complex Figure Test and the Wisconsin Card Sorting Test. Differences were more marked on processing speed and divided attention tests. |
| Innes et al.,25 2007, New Zealand | 62 | 36 men and 14 women; sensorimotor and cognitive tests, and a road test. | Road test failed by 64% of the subjects. Significant differences were identified between subjects who passed the road test and those who did not for all SMC test results except for visuospatial tests. |
| Akinwuntan et al.,26 2007, Belgium | 43 | Determine if 3 tests (Rey–Osterrieth complex figure, spatial neglect test, and road test) predicted driving test results. | 86% of the participants were classified correctly as ‘fit’ or ‘unfit’. Sensitivity and specificity levels were 77% and 92%, respectively. |
| Ponsford et al.,27 2008, United Kingdom | 200 | Analysis of the evaluation process to certify driving ability. | Of the total, 54% were rated fit to drive and 9% were able to drive a modified vehicle (after training). Cognitive impairment was the leading cause of not passing the exam. |
In 1993, Lincoln et al.28 showed that general practitioners’ interpretations of results from cognitive tests allowed them to predict the result of a road test in only 56% of the patient sample.28 In contrast, a multidisciplinary team made up of a neurologist and neuropsychologist was able to predict safe driving ability in 75% of the cases.7
The road test seems to be the most valid measurement, but this test remains subjective; there are no standard guidelines for what the test is intended to measure. Akinwuntan et al.20 used a 13-item list to evaluate this test. These authors concluded that the 13-item list was reliable and that results were good. Furthermore, results from non-road tests in the SDSA (Stroke Drivers’ Screening Assessment) coincided with results on road tests in 78.9% of the sample.20
Some have suggested that a combination of non-road tests (neurological and neuropsychological evaluation) and a road test would provide the most precise information about driving ability.17,26 It is understood that non-road tests select the patients who are prepared to take the road test, the step which to some extent provides the definitive answer regarding the patient's driving ability. Although researchers have identified 111 different predictors of the road test result, cut-off points are not sensitive or specific enough to support their utility in stroke patients.29 Nevertheless, the SDSA is considered the most feasible way of performing an initial non-road assessment.30
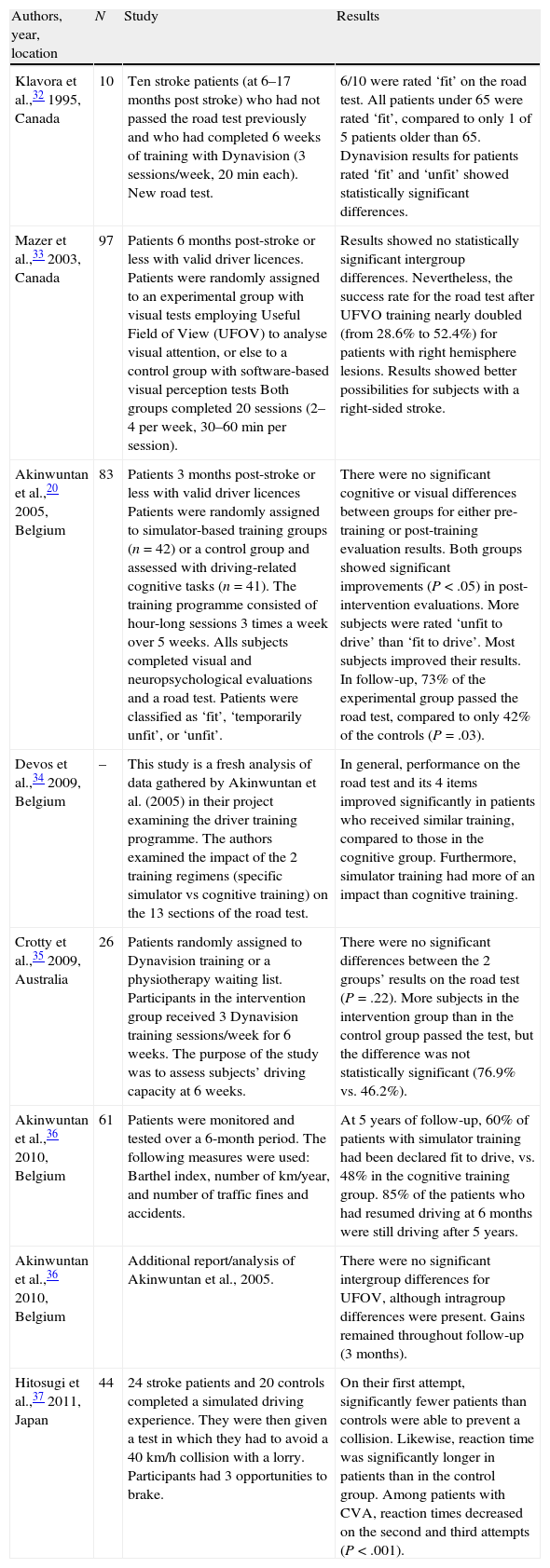
Interventions for improving driving abilityNeurorehabilitation should be tailored to the individual. Sufficient scientific evidence is available for some areas of the process, such as management of shoulder pain.31 Nevertheless, despite the importance of resuming driving for social integration and adopting a normal lifestyle after stroke, there have been few studies on interventions designed to improve driving ability post-stroke.
Table 2 presents articles that examine interventions aiming to improve patients’ driving ability after a stroke.
Studies addressing interventions intended to recover driving ability after a stroke.
| Authors, year, location | N | Study | Results |
| Klavora et al.,32 1995, Canada | 10 | Ten stroke patients (at 6–17 months post stroke) who had not passed the road test previously and who had completed 6 weeks of training with Dynavision (3 sessions/week, 20min each). New road test. | 6/10 were rated ‘fit’ on the road test. All patients under 65 were rated ‘fit’, compared to only 1 of 5 patients older than 65. Dynavision results for patients rated ‘fit’ and ‘unfit’ showed statistically significant differences. |
| Mazer et al.,33 2003, Canada | 97 | Patients 6 months post-stroke or less with valid driver licences. Patients were randomly assigned to an experimental group with visual tests employing Useful Field of View (UFOV) to analyse visual attention, or else to a control group with software-based visual perception tests Both groups completed 20 sessions (2–4 per week, 30–60min per session). | Results showed no statistically significant intergroup differences. Nevertheless, the success rate for the road test after UFVO training nearly doubled (from 28.6% to 52.4%) for patients with right hemisphere lesions. Results showed better possibilities for subjects with a right-sided stroke. |
| Akinwuntan et al.,20 2005, Belgium | 83 | Patients 3 months post-stroke or less with valid driver licences Patients were randomly assigned to simulator-based training groups (n=42) or a control group and assessed with driving-related cognitive tasks (n=41). The training programme consisted of hour-long sessions 3 times a week over 5 weeks. Alls subjects completed visual and neuropsychological evaluations and a road test. Patients were classified as ‘fit’, ‘temporarily unfit’, or ‘unfit’. | There were no significant cognitive or visual differences between groups for either pre-training or post-training evaluation results. Both groups showed significant improvements (P<.05) in post-intervention evaluations. More subjects were rated ‘unfit to drive’ than ‘fit to drive’. Most subjects improved their results. In follow-up, 73% of the experimental group passed the road test, compared to only 42% of the controls (P=.03). |
| Devos et al.,34 2009, Belgium | – | This study is a fresh analysis of data gathered by Akinwuntan et al. (2005) in their project examining the driver training programme. The authors examined the impact of the 2 training regimens (specific simulator vs cognitive training) on the 13 sections of the road test. | In general, performance on the road test and its 4 items improved significantly in patients who received similar training, compared to those in the cognitive group. Furthermore, simulator training had more of an impact than cognitive training. |
| Crotty et al.,35 2009, Australia | 26 | Patients randomly assigned to Dynavision training or a physiotherapy waiting list. Participants in the intervention group received 3 Dynavision training sessions/week for 6 weeks. The purpose of the study was to assess subjects’ driving capacity at 6 weeks. | There were no significant differences between the 2 groups’ results on the road test (P=.22). More subjects in the intervention group than in the control group passed the test, but the difference was not statistically significant (76.9% vs. 46.2%). |
| Akinwuntan et al.,36 2010, Belgium | 61 | Patients were monitored and tested over a 6-month period. The following measures were used: Barthel index, number of km/year, and number of traffic fines and accidents. | At 5 years of follow-up, 60% of patients with simulator training had been declared fit to drive, vs. 48% in the cognitive training group. 85% of the patients who had resumed driving at 6 months were still driving after 5 years. |
| Akinwuntan et al.,36 2010, Belgium | Additional report/analysis of Akinwuntan et al., 2005. | There were no significant intergroup differences for UFOV, although intragroup differences were present. Gains remained throughout follow-up (3 months). | |
| Hitosugi et al.,37 2011, Japan | 44 | 24 stroke patients and 20 controls completed a simulated driving experience. They were then given a test in which they had to avoid a 40km/h collision with a lorry. Participants had 3 opportunities to brake. | On their first attempt, significantly fewer patients than controls were able to prevent a collision. Likewise, reaction time was significantly longer in patients than in the control group. Among patients with CVA, reaction times decreased on the second and third attempts (P<.001). |
Visual attention training is not more effective than traditional visual perception training as a means of improving driving ability in stroke patients. Lastly, use of a simulator-based training programme presenting complex adapted scenarios that resemble those in real life is associated with better driving, increased ability, and success on road tests.
ConclusionsIf a stroke patient's driving ability is questionable, it must be thoroughly evaluated. If patients are unfit to drive, they should begin a neurorehabilitation programme designed to recover driving ability.
An assessment of driving ability should not be based solely on the road test or solely on a neurological/neuropsychological evaluation. The assessment should be considered in 2 steps: first, a multidisciplinary evaluation (neurological/neuropsychological assessment) to determine if the patient is ready for the road test, and the road test as the second and final step.
Patients may improve their driving ability by using simulators that reproduce real situations.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Murie-Fernandez M, Iturralde S, Cenoz M, Casado M, Teasell R. Capacidad de conducción tras un ictus: evaluación y recuperación. Neurología. 2014:29:161–167.