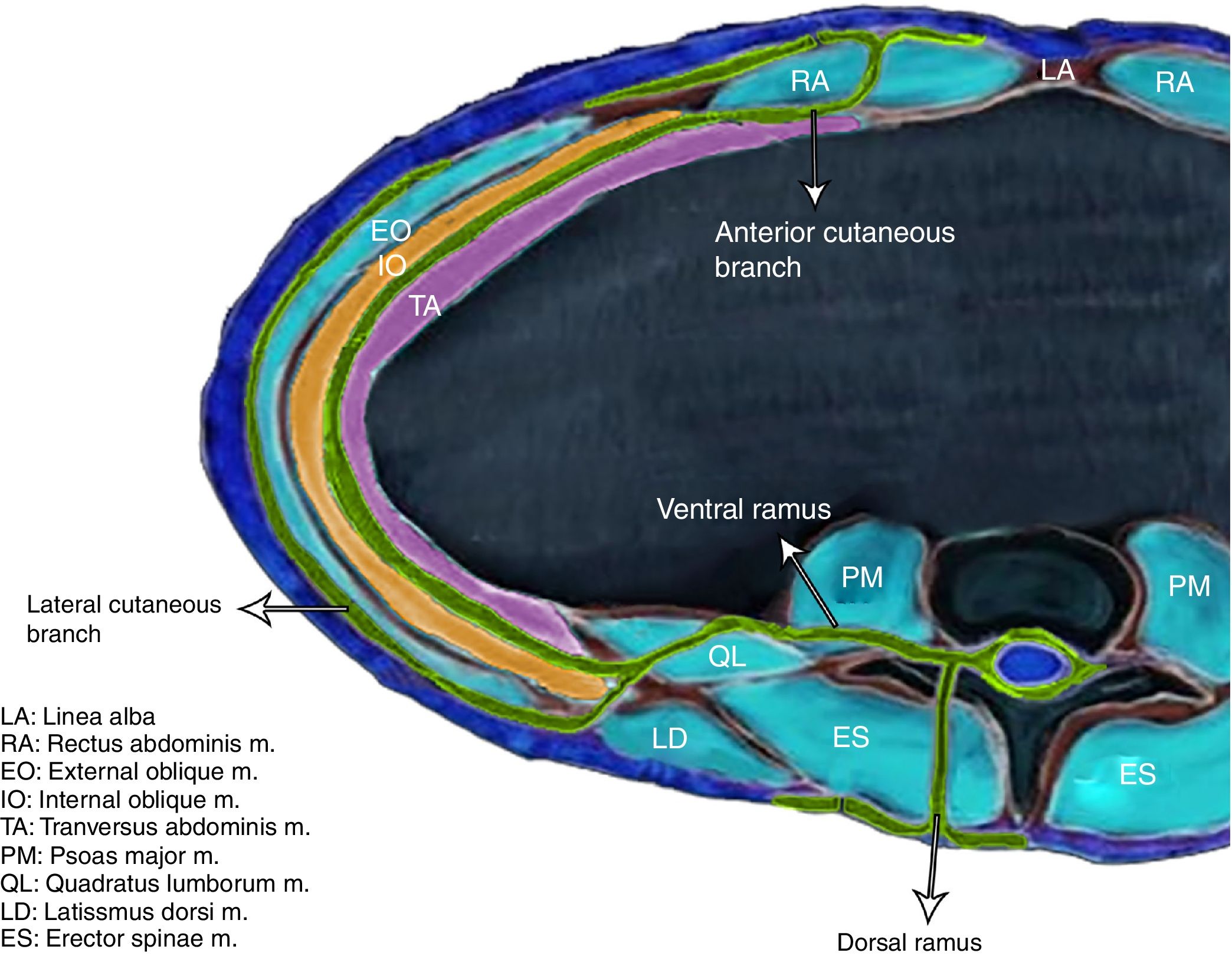
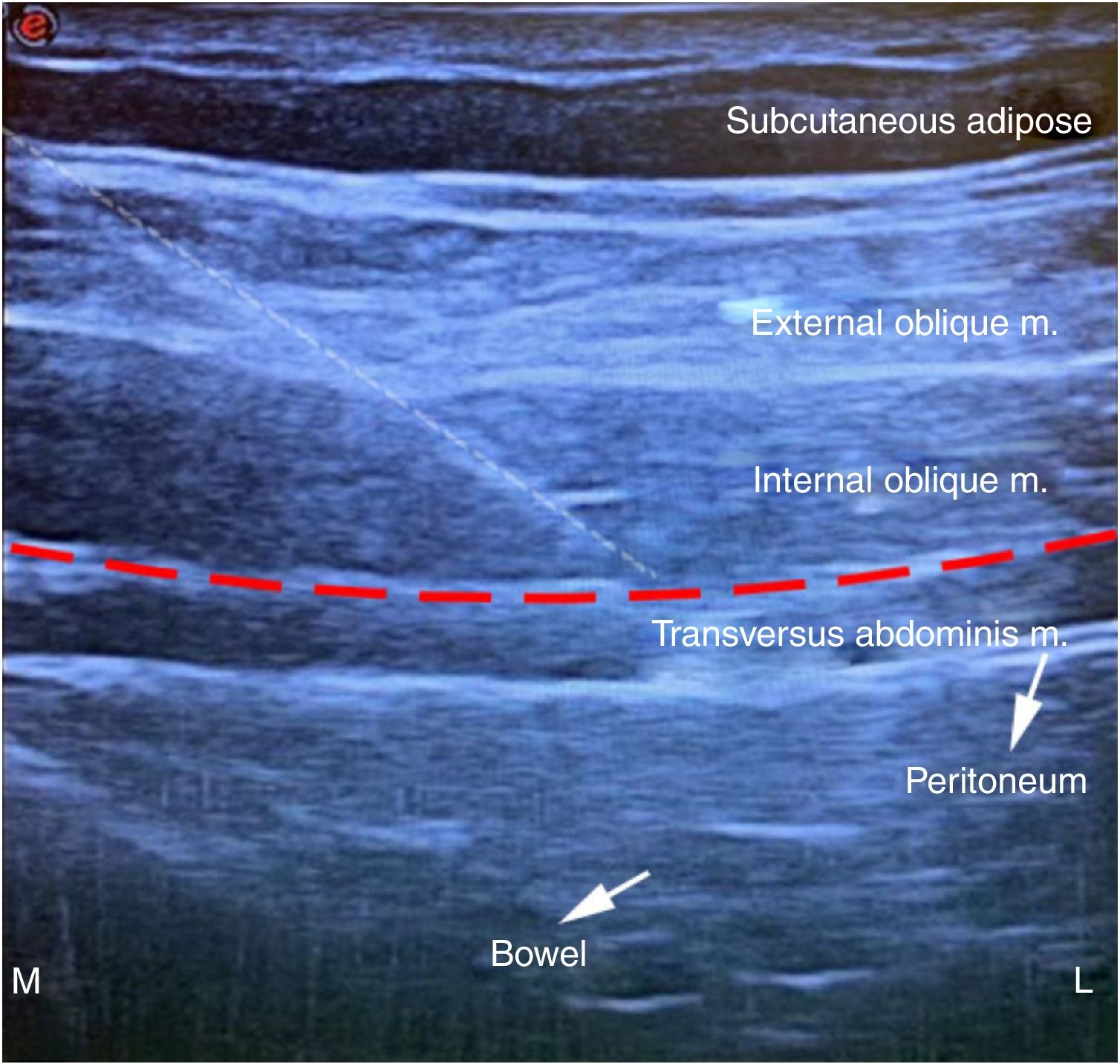
array:23 [ "pii" => "S2341192920301530" "issn" => "23411929" "doi" => "10.1016/j.redare.2020.01.015" "estado" => "S300" "fechaPublicacion" => "2020-12-01" "aid" => "1124" "copyrightAnyo" => "2020" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2020;67:572-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:18 [ "pii" => "S0034935620300463" "issn" => "00349356" "doi" => "10.1016/j.redar.2020.01.016" "estado" => "S300" "fechaPublicacion" => "2020-12-01" "aid" => "1124" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Rev Esp Anestesiol Reanim. 2020;67:572-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Director</span>" "titulo" => "Anestesia para reparación abierta de hernia inguinal con bloqueo ecoguiado en el plano del músculo transverso del abdomen en un paciente anciano de alto riesgo: caso clínico" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "572" "paginaFinal" => "574" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Anesthesia for open inguinal hernia repair with ultrasound-guided transversus abdominis plane block in a high-risk elderly patient: Case report" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0010" "etiqueta" => "Figura 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1433 "Ancho" => 1508 "Tamanyo" => 228583 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Vista ecográfica del bloqueo en el plano del músculo transverso del abdomen. La línea blanca discontinua representa la trayectoria de la aguja; la línea roja discontinua representa el plano del músculo transverso del abdomen.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "C. Kaya, C. Genc" "autores" => array:2 [ 0 => array:2 [ "nombre" => "C." "apellidos" => "Kaya" ] 1 => array:2 [ "nombre" => "C." "apellidos" => "Genc" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2341192920301530" "doi" => "10.1016/j.redare.2020.01.015" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192920301530?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935620300463?idApp=UINPBA00004N" "url" => "/00349356/0000006700000010/v1_202011270856/S0034935620300463/v1_202011270856/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2341192920301657" "issn" => "23411929" "doi" => "10.1016/j.redare.2020.05.011" "estado" => "S300" "fechaPublicacion" => "2020-12-01" "aid" => "1167" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2020;67:574-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Director</span>" "titulo" => "New evidence on the pharmacological management of neuropathic pain" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "574" "paginaFinal" => "576" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Nuevas evidencias sobre el manejo farmacológico del dolor neuropático" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:9 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "fuente" => "Source: adapted from Moisset et al.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a>" "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1714 "Ancho" => 2508 "Tamanyo" => 362669 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Proposal for a therapeutic algorithm for the pharmacological treatment of neuropathic pain in adults.</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">MME: morphine milligram equivalents; NP: neuropathic pain; SNRI: serotonin norepinephrine reuptake inhibitors.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "A. Alcántara Montero, C.I. Sánchez Carnerero" "autores" => array:2 [ 0 => array:2 [ "nombre" => "A." "apellidos" => "Alcántara Montero" ] 1 => array:2 [ "nombre" => "C.I." "apellidos" => "Sánchez Carnerero" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0034935620301456" "doi" => "10.1016/j.redar.2020.05.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935620301456?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192920301657?idApp=UINPBA00004N" "url" => "/23411929/0000006700000010/v1_202012131408/S2341192920301657/v1_202012131408/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2341192920301694" "issn" => "23411929" "doi" => "10.1016/j.redare.2020.07.005" "estado" => "S300" "fechaPublicacion" => "2020-12-01" "aid" => "1181" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2020;67:570-1" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Image of the month</span>" "titulo" => "Epileptic crisis and headache after a lumbar epidural steroid injection" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "570" "paginaFinal" => "571" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Crisis epiléptica y cefalea tras infiltración epidural lumbar con corticoides" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1160 "Ancho" => 2175 "Tamanyo" => 144511 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Cranial CT. Different slices showing pneumocephalus. Multiple air collections in basal cisterns, in bilateral frontal parasagittal, right temporal and intraventricular sulci, in both frontal horns, and in the right temporal horn (arrows).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "L. España Fuente" "autores" => array:1 [ 0 => array:2 [ "nombre" => "L." "apellidos" => "España Fuente" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0034935620301730" "doi" => "10.1016/j.redar.2020.07.001" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935620301730?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192920301694?idApp=UINPBA00004N" "url" => "/23411929/0000006700000010/v1_202012131408/S2341192920301694/v1_202012131408/en/main.assets" ] "en" => array:14 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Director</span>" "titulo" => "Anesthesia for open inguinal hernia repair with ultrasound-guided transversus abdominis plane block in a high-risk elderly patient: Case report" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "572" "paginaFinal" => "574" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "C. Kaya, C. Genc" "autores" => array:2 [ 0 => array:4 [ "nombre" => "C." "apellidos" => "Kaya" "email" => array:1 [ 0 => "cengiz.kaya@omu.edu.tr" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "C." "apellidos" => "Genc" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Department of Anesthesiology, School of Medicine, Ondokuz Mayis University, Samsun, Turkey" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Anestesia para reparación abierta de hernia inguinal con bloqueo ecoguiado en el plano del músculo transverso del abdomen en un paciente anciano de alto riesgo: caso clínico" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1620 "Ancho" => 2088 "Tamanyo" => 283013 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Cross section of the abdominal wall showing the muscles and surrounding nerves (T7-T12).</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Open inguinal hernia repair is a common surgical procedure.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> Transverse abdominis plane (TAP) block may be an option for patients at high risk of perioperative complications.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> TAP block involves injecting a local anaesthetic (LA) into the interfascial plane between the internal oblique and transverse abdominal muscles. Anatomically, the anterior branches of the lower thoracic spinal nerves (intercostal [T7-11], subcostal [T12] and iliohypogastric/ilioinguinal [L1] nerves) innervate the anterolateral abdominal wall. The anterior branches (T7-12) run through the neurovascular plane between the internal oblique and transverse muscles, and bifurcate into the cutaneous and anterior branches (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). The L1 root bifurcates into the iliohypogastric/ilioinguinal nerve branches, which contribute to the innervation of the inguinal region. The TAP block provides a certain degree of somatic block, but does not reach the sympathetic afferents, and therefore does not prevent visceral pain during abdominal surgery.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a> However, case reports on the use of TAP block plus sedation for anaesthesia in open gastrostomy, open appendectomy, emergency laparotomy and paediatric vesicostomy encouraged us to use this technique in surgical anaesthesia.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a></p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">We describe the case of a 77-year-old man, height 175<span class="elsevierStyleHsp" style=""></span>cm, weight 85<span class="elsevierStyleHsp" style=""></span>kg, high risk, who underwent open inguinal hernia repair with ultrasound-guided unilateral TAP block plus intravenous (IV) infusion of remifentanil. The patient suffered from coronary artery disease, hypertension, and congestive heart failure (NYHA class III). Labs were within normal limits, but the patient's electrocardiogram showed atrial fibrillation, and the echocardiography showed a left ventricular ejection fraction of 25%, pulmonary artery pressure of 40<span class="elsevierStyleHsp" style=""></span>mmHg, and moderate to severe tricuspid-mitral regurgitation. High-resolution chest CT scan showed diffuse tubular bronchiectasis and vitreous nodules in the lungs. The patient was classed as IV on the American Society of Anesthesiologists (ASA) physical status scale. Informed consent was obtained from the patient. After standard monitoring and before administering the block, infusion of 0.05–0.1<span class="elsevierStyleHsp" style=""></span>μg/kg/min IV remifentanil was started to allow verbal communication. The patient was placed in a supine position. The block was administered using a high-frequency linear ultrasound transducer (MyLab® Five, Esaote, Florence, Italy) placed between the subcostal margin and the iliac crest, at the level of the umbilicus, to visualise the external oblique, internal oblique and TAP muscles, as well as the peritoneal cavity (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>). The nerve block needle (100<span class="elsevierStyleHsp" style=""></span>mm, 21G short bezel; Stimuplex®, B. Braun, Melsungen, Germany) was inserted in plane in an anterolateral to posterior direction. After checking for flashback, 20<span class="elsevierStyleHsp" style=""></span>ml of 0.5% bupivacaine was injected. The surgical procedure began after evaluating the sensory block in the T10-L1 dermatomes. Intraoperative abdominal pain that occurred during hernial sac dissection was treated with remifentanil (0.025–0.05<span class="elsevierStyleHsp" style=""></span>μg/kg/min) and IV ketamine in divided doses (25<span class="elsevierStyleHsp" style=""></span>mg total). Intraoperative haemodynamic parameters were similar to preoperative values. The patient was admitted to the intensive care unit for postoperative monitoring, and 16<span class="elsevierStyleHsp" style=""></span>h later was transferred to the general surgery ward, with no sign of complications. No incidents have yet been reported (1 month after surgery).</p><elsevierMultimedia ident="fig0010"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">In ultrasound-guided unilateral TAP block, LA is administered in the mid-axillary line, providing anaesthesia to the lower abdominal wall from the midline to the midclavicular line. This technique is only useful for periumbilical and infraumbilical interventions, since the LA does not spread above T10. However, the spread of LA around the ilioinguinal/iliohypogastric nerve and the internal oblique muscle cannot always be predicted due to anatomical variations, and a separate ilioinguinal/iliohypogastric nerve block is sometimes required, particularly when the hernial incision includes the T12-L1 dermatome.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a></p><p id="par0020" class="elsevierStylePara elsevierViewall">Although few TAP block-related complications have been reported, some cases of intraoperative bradycardia in response to IV atropine have been published (0.5<span class="elsevierStyleHsp" style=""></span>mg). Other complications include intraperitoneal injection, colon and liver injury, seizures, ventricular arrhythmia, and transient paralysis of the femoral nerve.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a> Considering the brief analgesic effect (4–12<span class="elsevierStyleHsp" style=""></span>h) of a single injection of LA in the TAP block, adding dexamethasone to this LA, which we do not use in our clinical practice, could increase the quality and duration of analgesia, and reduce the opioid consumption and opioid-related complications.<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">5</span></a></p><p id="par0025" class="elsevierStylePara elsevierViewall">Therefore, our case has shown that open inguinal hernia repair can be successfully performed by administering IV remifentanil combined with unilateral TAP block. Ultrasound-guided TAP block is a safe, effective anaesthetic option in high-risk patients scheduled for lower abdominal surgery.</p></span>" "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:2 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Kaya C, Genc C. Anestesia para reparación abierta de hernia inguinal con bloqueo ecoguiado en el plano del músculo transverso del abdomen en un paciente anciano de alto riesgo: caso clínico. Rev Esp Anestesiol Reanim. 2020;67:572–574.</p>" ] 1 => array:2 [ "etiqueta" => "☆☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0010">This case report is an oral presentation delivered to the Regional Anaesthesia Congress, held from 27 to 30 April 2019 in Izmir, Turkey.</p>" ] ] "multimedia" => array:2 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1620 "Ancho" => 2088 "Tamanyo" => 283013 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Cross section of the abdominal wall showing the muscles and surrounding nerves (T7-T12).</p>" ] ] 1 => array:7 [ "identificador" => "fig0010" "etiqueta" => "Figure 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1433 "Ancho" => 1508 "Tamanyo" => 229326 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Ultrasound view of the block in the transverse abdominal plane. The dashed white line shows the trajectory of the needle; the dashed red line shows the plane of the transversus abdominis muscle.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Efficacy of ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing inguinal hernia repair" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "R. Venkatraman" 1 => "R.J. Abhinaya" 2 => "A. Sakthivel" 3 => "G. Sivarajan" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.2147/LRA.S93673" "Revista" => array:6 [ "tituloSerie" => "Local Reg Anesth" "fecha" => "2016" "volumen" => "9" "paginaInicial" => "7" "paginaFinal" => "12" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26848274" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Transversus abdominal plane block as a sole anesthetic technique for abdominal wall hematoma drainage" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "N. Varela" 1 => "M. Golvano" 2 => "P. Monedero" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.redar.2015.12.001" "Revista" => array:6 [ "tituloSerie" => "Rev Esp Anestesiol Reanim" "fecha" => "2016" "volumen" => "63" "paginaInicial" => "487" "paginaFinal" => "490" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26774971" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Transversus abdominis plane block: an updated review of anatomy and techniques" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "H.C. Tsai" 1 => "T. Yoshida" 2 => "T.Y. Chuang" 3 => "S.F. Yang" 4 => "C.C. Chang" 5 => "H.Y. Yao" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1155/2017/8284363" "Revista" => array:4 [ "tituloSerie" => "Biomed Res Int" "fecha" => "2017" "volumen" => "2017" "paginaInicial" => "12" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Transversus abdominus blocks instead of general anesthesia in a child" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "F. AlGhamdi" 1 => "M. AlSuhebani" 2 => "J.D. Tobias" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.4103/sja.SJA_433_19" "Revista" => array:6 [ "tituloSerie" => "Saudi J Anaesth" "fecha" => "2019" "volumen" => "13" "paginaInicial" => "377" "paginaFinal" => "380" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/31572089" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Dexamethasone added to local anesthetics in ultrasound-guided transversus abdominis plain (TAP) block for analgesia after abdominal surgery: a systematic review and meta-analysis of randomized controlled trials" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "D. Zhang" 1 => "C. Zhou" 2 => "D. Wei" 3 => "L. Ge" 4 => "Q. Li" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1371/journal.pone.0209646" "Revista" => array:5 [ "tituloSerie" => "PLOS ONE" "fecha" => "2019" "volumen" => "14" "paginaInicial" => "e0209646" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/30620730" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23411929/0000006700000010/v1_202012131408/S2341192920301530/v1_202012131408/en/main.assets" "Apartado" => array:4 [ "identificador" => "66474" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letter to the Director" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23411929/0000006700000010/v1_202012131408/S2341192920301530/v1_202012131408/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192920301530?idApp=UINPBA00004N" ]
Journal Information
Vol. 67. Issue 10.
Pages 572-574 (December 2020)
Share
Download PDF
More article options
Vol. 67. Issue 10.
Pages 572-574 (December 2020)
Letter to the Director
Anesthesia for open inguinal hernia repair with ultrasound-guided transversus abdominis plane block in a high-risk elderly patient: Case report
Anestesia para reparación abierta de hernia inguinal con bloqueo ecoguiado en el plano del músculo transverso del abdomen en un paciente anciano de alto riesgo: caso clínico
Visits
84
Department of Anesthesiology, School of Medicine, Ondokuz Mayis University, Samsun, Turkey
This item has received
Article information
These are the options to access the full texts of the publication Revista Española de Anestesiología y Reanimación (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail