To compare clinically and radiologically the results obtained using both a direct anterior approach (DAA) and posterolateral (PL) approach in total hip arthroplasty (THA).
Material and methodsMulticentric longitudinal prospective study in 80 patients (80 THA). Forty patients underwent total hip arthroplasty through DAA and 40 through a PL approach. The following clinical parameters were collected: anaesthesia, length of surgical incision, duration of the procedure, lower limb discrepancy, pain, complications, hospitalization time, Harris Hip Score (HHS) and subjective patient satisfaction. Radiological measures collected were acetabular tilt angle, acetabular component version, osteointegration and lower limb length.
ResultsPostoperative pain DAA 4 points; PL 4.3 points. Incision length DAA 14 cm, PL 15 cm. Mean hospital stay DAA 2.8 days, PL 3.4 days. HHS at 3 weeks, DAA 87.5 and PL 84 points; at 2 months DAA was 92 and PL 91 points. Femoral stem subsidence was noticed in 4 patients from DAA and 1 from PL. Malalignment was reported in 9 cases from the DAA group.
ConclusionsOur results show an initial advantage of the DAA group regarding functional recovery and pain that enabled shorter hospitalization time. This difference equalled out over two months following the procedure. Likewise, we detected a greater complication rate in the DAA group using standard cementless stems.
Realizar una comparación funcional y radiográfica de los resultados iniciales obtenidos con la utilización de los abordajes anterior directo y posterolateral en artroplastia total de cadera.
Material y métodoEstudio longitudinal prospectivo multicéntrico en 80 pacientes (80 artroplastias totales de cadera). 40 pacientes fueron intervenidos mediante abordaje anterior directo (AAD) y 40 pacientes mediante abordaje posterolateral (PL). Se recogieron los siguientes parámetros clínicos: anestesia, abordaje, longitud de la incisión cutánea, duración de la cirugía, discrepancia de longitud, dolor, complicaciones, tiempo de ingreso, escala funcional de Harris (HHS) y satisfacción de los pacientes. En cuanto a los parámetros radiográficos, se recogieron ángulo de inclinación acetabular, anteversión acetabular, integración del cotilo, integración y orientación del vástago y longitud del miembro inferior.
ResultadosDolor postoperatorio AAD 4 puntos; PL 4,3 puntos. Tamaño incisión AAD 14 cm; PL 15 cm. Duración media del ingreso hospitalario AAD 2,8 días; PL 3,4 días. HHS a las 3 semanas AAD 87,5 puntos, PL 84 puntos; 2 meses AAD 92 puntos, PL 91 puntos. Se detectó hundimiento del vástago femoral en 4 pacientes AAD y 1 PL y malalineación en 9 casos del grupo AAD.
ConclusionesNuestros resultados muestran que a pesar de una leve mejoría inicial del abordaje anterior directo en la recuperación funcional y dolor de los pacientes que permite una menor estancia hospitalaria. Esta diferencia se compensa aproximadamente a los dos meses postoperatorios. Asimismo se ha detectado un mayor índice de complicaciones en al AAD con el uso de vástagos no cementados estándar.
Total hip arthroplasty (THA) is one of the most common orthopedic operations. In the United States today approximately 300,000 THA are performed each year, and an exponential rise is expected toward the end of the decade.1 Many approaches have been described for THA, with the most used being the posterolateral (PL), the direct lateral and the anterolateral approach.2 At present there is a growing interest in the direct anterior approach (DAA). Some of its theoretical advantages is the possibility of reducing muscular damage directly attributed to the approach, which would lead to faster functional recovery, less postoperative pain and better biomechanics when walking which would not interfere with the abductor mechanism.3–5
The DAA uses the internervous plane described by Hueter in 1883,6 between the sartorious muscles, innervated by the femoral nerve and the tensor fasciae latae muscle (TFL), innervated by the superior gluteal nerve. This approach was popularized in the United States by Marius Smith Petersen in 1917.7
During the decade of the 1980’s interest revived in the DAA in THA following the publication of a series of 104 cases.8 One of the authors subsequently proposed a modification in the approach, consisting of entering over the TFL fascial sheath instead of medial to it.9
The aim of this study was to clinically and radiologically compare the initial results obtained using the DAA versus the PL approach with the use of a single type of standard cementless stem prosthesis.
Material and methodBetween January 2015 and December 2015 a longitudinal prospective study was conducted for clinical and radiographic comparison between the DAA and the PL approach for primary THA. The study was approved by the Ethics Committee of the centers involved and the patients who participated signed their informed consent. Inclusion criteria were patients with an age range between 21 and 70 with primary or secondary osteoarthritis to avascular necrosis and/or rheumatoid arthritis. Patients over 70 were excluded from the study as were those with THA secondary to hip fracture, THA secondary to dysplasia of the hip and/or previous operations in the hip to be operated on. The maximum age was 70 established by consensus between the study surgeons as the limit for cementless prosthesis referral.
The study comprised 80 patients upon whom 80 primary cementless THA were performed, 40 through DAA and 40 through PL. The mean age of the patients was 56.5 with a range from 25 to 70 years. Patients were not stratified according to their body mass index or body frame.
The following clinical parameters were collected: type of anesthesia, type of approach, length of skin incision, length of surgical procedure, discrepancy of postoperative length, pre and postoperative pain, complications (fractures, instability, infection, neurovascular complications, thromboembolism, wound complications), length of hospital stay, function Harris scale (Harris Hip Score [HHS])10 and subjective satisfaction of the patients (referring to their overall appreciation of the procedure and expectations regarding the same, on a scale from 1 to 10, where a result from 1 to 3 points was considered poor, 4–5 points satisfactory, 6–8 points good and 9–10 points excellent).
With regard to approaches, the DAA and PL approach were used. For the DAA a standard surgical table was used without any image intensifier. The patient was placed in supine position, and a skin incision was made 2–3 cm distal and lateral to the anterosuperior illiac spine to avoid wounding the cutaneous nerve of the thigh. Following this the interval between the Sartorius and the TFL muscles was dissected and arthrotomy was performed. The implants were inserted without the use of specific instrumentation.
For the PL approach the patient was placed in a semi-supine position and a straight incision was made centered in the union of the middle and posterior thirds of the trochanter muscle. The tendon was reflected from the pyramidal retracting it with a Hohmann type separator while the other hip balls were removed en bloc, together with the joint capsule to be reinserted according to the Pellicci et al.11 technique once the final components were implanted.
For preparation of the acetabular component “line to line” drilling of the same diameter as the final component was performed. The femoral component was prepared using compaction rasps. To check intraoperative hip stability tests with the articular balance were performed (with seating, internal and external rotation, and the combined internal rotation of 15° and flexion of 45°), push and pull technique with the limb extended and with flexion of the knee at 90°; length was confirmed bearing in mind preoperative and intraoperative measurement of the delta distance (distance from the proximal edge of the lesser trochanter to the center of rotation of the femoral head).12
The implants used were modular cementless Crown Cup (Exactech, Gainesville, FL, U.S.A.) with two routine supplementary fixation screws, a highly cross-linked polyethylene insert with 10° flap, Element femoral stem (Exactech, Gainesville, FL, U.S.A.) with a dual-tapered design and complete hydroxyapetite coating (Exactech, Gainesville, FL, U.S.A.) with a 32 mm metallic head of cobalt-chrome.
The visual analogue scale (VAS)13 was used to measure pre and postoperative pain on a scale from 0 (no pain) to 10 (maximum pain).
Prophylaxis antibiotic used was 1 g cefazolin, initiated prior to the skin incision and every 8 h during the first 24 h. In patients who were allergic to B-Lactam antibiotics 1 g of vancomycin was administered every 12 h for the first postoperative 24 h. For postoperative thromboembolic prophylaxis rivaroxabán was administered, 40 mg for 21 days.
All the patients were assessed preoperatively by the rehabilitation service so as to be informed about mobilization and ambulation techniques. A fast-track rehabilitation protocol was established which began the first day after surgery with seated exercises and walking with a walking frame or sticks depending on the functional capacity of each patient, unless clinically contraindicated. Clinical and radiographic follow-up was performed after 3 weeks and at 2, 6 and 12 months after surgery and in the following years. Patient satisfaction was based on subjective evaluation of the patients and was classified as excellent, good, standard or bad.
Radiographic measurementsThe radiographic technique was standardized, maintaining the center in pubic symphysis and the beam of the X rays at 110 cm from the table. In all patients radiographies in acetate in real size for preoperative planning were obtained, where the size of the components was calculated and the delta distance (taken from the proximal end of the lesser trochanter to the center of the prosthetic head).12 During the follow-up consultations the following radiographic measurements were taken: acetabular angle, acetabular anteversion, cup integration, integration and direction of the stem and length of the lower limb.
The appropriate acetabular angle was established as between 30° and 50°.14 For measuring the acetabular anteversion the Ackland technique was used, with an expected 0° to 15° of anteversion.15 Cup loosening was defined as a change of over 5° of slant in several radiographies, the rotation of screws or the progression of radiolucences in the DeLee and Charnley16 areas in several radiographies with symptomatic patients. In the femoral stem the integration based on the criteria of Engh17 was measured for cementless stems, while also assessing the migration or collapse and the appearance of the sign of the pedestal (comparing the distance of the stem shoulder to the lesser trochanter).18 To define stem orientation the traced line was used in the central axis of the femoral canal with the greater axis of the stem. Length was quantified in anteropostieor radiography of the pelvis comparing the distance from the center of the femoral head in the non operated hip up to the most proximal point of the lesser trochanter, with the distance from the center of the prosthetic head to the same point of the lesser trochanter on the operated side.
Statistical analysis was performed with an SPSS Statistics system (IBM, New York, U.S.A.), using the students t-test and Chi squared test for parametric (which analyze the population and its characteristics), and categorical variables (where each case is assigned a certain value of the result), respectively, considering a p value of <.05 as significant.
ResultsMinimum follow-up was one year, with a range of between 12 and 33 months and an average of 17.6 months.
No statistically significant differences were found in the demographic data in either group. The DAA group presented with a mean age of 56.1 years (range 31–70 years), with a higher percentage of males (23 cases, 57% of the group); in the PL group mean age was 57.2 years (range 25–70 years), also with a higher percentage of males (25 patients, 62% of the group). THA indications in the DAA group were primary osteoarthritis in 34 cases, avascular necrosis of bone in 4 and rheumatoid arthritis in 2. In the PL group indications were for primary osteoarthritis in 35 cases and avascular necrosis in 5. Spinal anesthesia was administered in all except 5 patients (3 DAA, 2 PL).
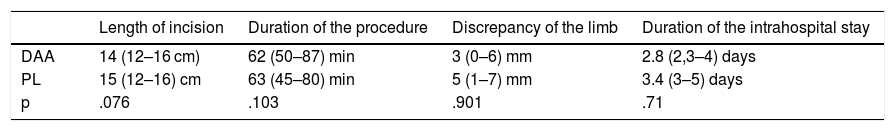
The results of the length of surgery, incision size, hospital stay and discrepancy of length are contained in Table 1. It is of note that the patients of the PL group had a hospital length of stay almost one day longer than the patients in the DAA group.
Results of the procedure.
| Length of incision | Duration of the procedure | Discrepancy of the limb | Duration of the intrahospital stay | |
|---|---|---|---|---|
| DAA | 14 (12–16 cm) | 62 (50–87) min | 3 (0–6) mm | 2.8 (2,3–4) days |
| PL | 15 (12–16) cm | 63 (45–80) min | 5 (1–7) mm | 3.4 (3–5) days |
| p | .076 | .103 | .901 | .71 |
DAA: direct anterior approach; PL: posterolateral approach.
To date no patients have been lost to follow-up.
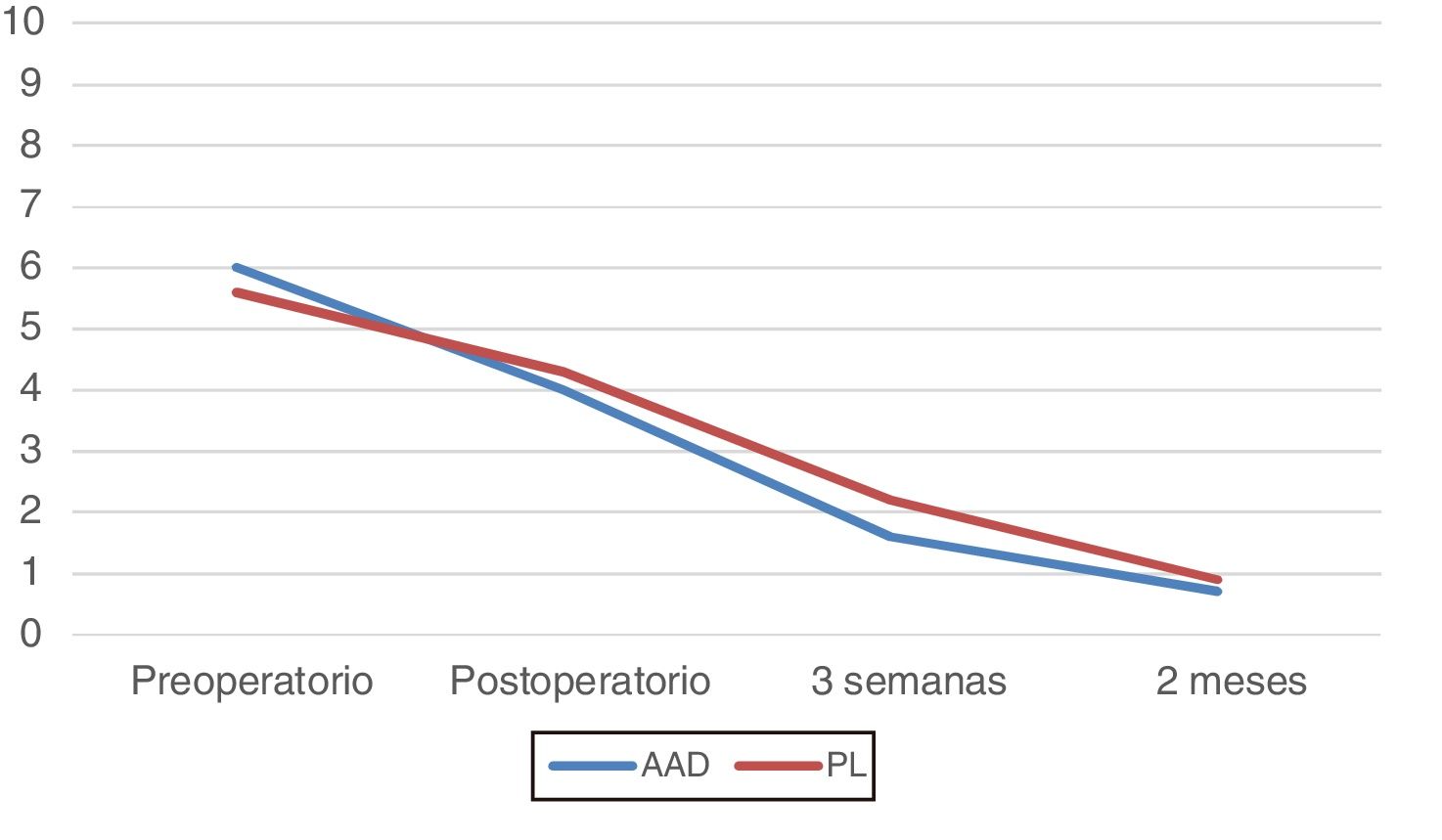
Functional resultsPain. Mean assessments of the patients were (Fig. 1):
- 1
DAA: preoperative 6 points; postoperative 4 points; 3 weeks 1.6 points; 2 months .7 points, which stayed the same until the last check-up control.
- 2
PL: preoperative 5.6 points; postoperative 4.3 points; 3 weeks 2.2 points; 2 months .9 points, which stayed the same until the last check-up control.
There were no statistically significant differences in our study, since only small differences showed up in favor of the DAA group during the initial periods.
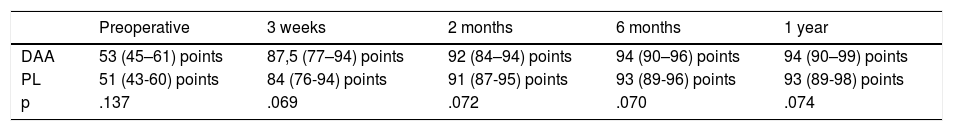
HHS. There were no statistically significant differences in our study in the preoperative or follow-up consultations (Table 2).
Functional results assessed with the Harris Hip Score (HHS).
| Preoperative | 3 weeks | 2 months | 6 months | 1 year | |
|---|---|---|---|---|---|
| DAA | 53 (45–61) points | 87,5 (77–94) points | 92 (84–94) points | 94 (90–96) points | 94 (90–99) points |
| PL | 51 (43-60) points | 84 (76-94) points | 91 (87-95) points | 93 (89-96) points | 93 (89-98) points |
| p | .137 | .069 | .072 | .070 | .074 |
DAA: direct anterior approach; PL: posterolateral approach.
Clinical complications. There were 5 cases (6.25%). Three were intraoperative calcar fractures during impactation of the femoral stem, which occurred in the DAA group. Surgical wound dehiscence also occurred and a subjectively unsightly scar. In one DAA group patient femoral cutaneous neuropraxia occurred which was recovered from without sequelae at the 3 month check-up. There were no cases of dislocation, infection, DVT, or TEP. No case required review surgery in the last follow-up control, and the cases are still being monitored.
Patient satisfaction. Out of the 80 patients in the study, 75 were classed as excellent (93.75%) and 5 as standard (6.25%), coinciding with the patients who had had complications.
Radiographic resultsAcetabular component. DAA: slant angle 42° (range 38°–47°) and anteversion 12° (range 3°–21°). PL: slant angle 45° (range 38°–51°) and anteversion 18° (range 7°–25°). In 3 cases non progressive radiolucent lines were detected (2 PL and 1 DAA) with no further symptoms.
Femoral stem. There were 5 cases of stem subsidence, 4 in the DAA group and one in the PL group, all detected in the check-up control at 2 months. The average subsidence was 2.3 mm (range 0–4 mm), and was non progressive. Two cases of pedestal were detected (1 DAA and 1 PL). Stem alignment was neutral in 71 cases, in the DAA group there were 7 varus cases and 2 valgus cases. All the cases were appropriately implanted on the basis of the Engh classification.
Patients who presented with radiolucent lines in the acetabulum and subsidence were closely monitored and to date there has been no drop in functional or pain scores.
The discrepancies described, although radiological, in 2 patients (1 DAA and 1 PL) were the detection of differences in length with the assessments up to 2 months. They disappeared after one year and there were no changes to the assessment of functional results or subjective patient assessments.
DiscussionThe aim of this study was to compare the initial clinical and radiologic results of the DAA approach versus the PL approach in THA. The results of our study show that although in the initial periods there is a minor difference in the results of the VAS and HHS in favour of the DAA, they are not statistically significant and even out after 3 months of follow-up. In 2009 Nakata et al.3 published a series of 195 THA using DAA or the miniposterior approach, and found that in the DAA group there was less need for external aid after 6 weeks, with the Merle d’Aubigne scale being the same in both groups after 2 and 6 months. In 2013 Barrett et al.19 published a series of 87 cases comparing the DAA and PL approaches, concluding that the DAA group presented with a higher ambulatory capacity and less difficulty in climbing upstairs, with the functional scores in both groups after 6 months being the same. They also reported a lower hospital stay in the DAA group, similarly to our study, which was almost one day less. This could be an economic factor to consider due to the expected exponential increase in THA in the short term.
However, studies also exist which do not coincide with these findings. In 2014 Poehling-Monaghan et al.20 published a series of 222 hips which had been operated on by DAA or PL, and they found no differences in hospital stay. In this study they also concluded that the PL group was less dependent on external aids for ambulation at 2 weeks and there were higher return to work rates than the DAA at 2 months.
Procedure duration was not statistically significant, and we could attribute it to the experience of the surgeons in using the two approaches. The learning curve of the DAA is long and there are studies which show differences in this aspect when the surgeons change for one approach to another.21–23
With regard to pain assessment, it seems that the same happens as with functionality, that the subjective perception is lower with DAA initially but that it evens out after 3 weeks and is not significant in subsequent control examinations.3,5 The discrepancy of length observed was lower in the DAA, and could be attributed to the patient being placed in supine position which enables a better intraoperative estimation on being able to palpate the anterosuperior iliac spines, hip balls and malleoli. This was published by Barnett et al.,24 but in their study they used a traction table and intraoperative fluoroscopy. The length discrepancy observed in the PL in our study entered into the pelvic compensation range, with no adverse results.
In our series no dislocations occurred, which is noteworthy when comparing both approaches. In the literature it has been calculated that there is a rate of almost 1% of dislocation in the PL approach if 32 mm heads are used, combined with an appropriate capsular closure and reinsertion of hip balls.10,21
Furthermore, the appearance of proximal fractures in the calcar region was detected during implantation of the femoral stem in the DAA approach, which is also reflected in our study. This could be attributed to the use of straight stems, to the difficult manipulation of the proximal femur during this approach and the learning curve. Our rate of 3.75% is similar to that reported in the use of straight stems, although there are studies published with a lower rate, of approximately 1%, with short and curved stems.21–24,26
With regards to wound complications, our study reported a lower rate of dehiscence than that published by Jewett y Collis25 (4.6% wound complications) or that of Barnett et al.24 (1%).
Regarding radiographic assessment, the orientation of the cup was similar in both approaches, with a greater dispersion in PL, which is also in keeping with the literature, probably secondary to the alteration of acetabulum observation in the lateral position which enables pelvic tilting.2,12,21–24 However, it should be pointed out that the articles which report lower dispersion with DAA use an image intensifier for implant insertion,21,22 which was not our case, although the reproducibility in orientation of the acetabulum is in our case is due to the routine use of the transverse ligament as anatomical reference for slant and anteversion. Regarding the femoral stem, in the DAA a tendency to significant varus was observed (7 out of 40 cases), probably for the previously mentioned reasons regarding handling of the proximal femur.
The main advantage of our study was that all the patients were operated on by hip surgeons experienced in both approaches, thus reducing the possibility of complications attributable to the learning curve. In the literature it is estimated that a learning curve of between 40 and 100 THA by anterior approach is required to eliminate these complications.21,22 the patients were not selected by weight or body frame.
The limitations of our study were the small number of patients and the randomization of them. The results obtained were short term and a long term follow-up could mark a difference regarding implant survival.
ConclusionsThe results obtained show that DAA has an initial advantage in functional recovery and pain for the patients and this gives rise to a shorter hospital stay. This difference is compensated for at approximately 2 months after the operation. No significant differences were found regarding the procedure, although a higher rate of complications in the DAA was detected with the use of standard cementless stems.
Level of evidenceLevel of evidence type 2. Comparative, prospective non randomized study.
FinancingNo financing was received for this study.
Conflict of interestsThe authors have no conflicts of interests to declare with regard to this study and the materials used.
Please cite this article as: Godoy-Monzon D, Buttaro M, Comba F, Piccaluga F, Cid-Casteulani A, Ordas A. Estudio comparativo radiológico y funcional del abordaje anterior directo versus abordaje posterolateral de cadera. Rev Esp Cir Ortop Traumatol. 2019;63:370–375.