The instability in hip arthroplasty, or joint dislocation in its most dramatic form, is a complication that changes the outcome of this procedure, causing a decrease in the quality of life of the patients, and a loss of confidence in their relationship with the surgeon. If we discount failures due to infection, dislocation is the most frequent cause of a short to medium term revision, and the number of cases that require several operations to provide stability to the joint is not insignificant. Despite the frequency and severity of this complication there are few studies with a high level of scientific evidence on this subject. We have attempted to review the published literature and its level of evidence on the pathogenic origin, prophylaxis and treatment of this eventuality. As well as recording and summarizing the findings of each study in this review, we have added the evidence level of the corresponding literature reference.
La inestabilidad en las artroplastias de cadera o la luxación en su forma más dramática, es una complicación que altera la evolución de este procedimiento introduciendo una pérdida de bienestar en el paciente y una pérdida de confianza en su relación con el cirujano. Si no consideramos los fracasos por infección, la luxación supone la causa más frecuente de cirugía de revisión a corto y medio plazo y no es desdeñable el número de casos que precisan varias intervenciones para aportar estabilidad a la articulación. A pesar de la frecuencia y gravedad de esta complicación no son frecuentes estudios con alta evidencia científica en este tema. Hemos pretendido recoger la literatura publicada con su grado de evidencia acerca de la etiopatogenia, profilaxis y tratamiento de esta eventualidad. Para ello además de anotar y resumir los hallazgos de cada trabajo, hemos añadido el nivel de evidencia tras la cita bibliográfica correspondiente.
One of the most common complications of total hip replacement (THR)—and among those generating the greatest dissatisfaction for both surgeon and patient—is dislocation or instability of the THR. A good number of articles have been published on this subject. The purpose of this review article, however—not to disregard those articles1–4—is to analyse certain controversial aspects of this complication through the lens of scientific evidence. Because the problem areas and possible solutions have changed over time, obviously, we have reviewed articles published since the year 2000, primarily, although some key references prior to that date were included in the study.
We have examined and judged different authors’ statements as to whether, based on current criteria, they present scientific, clinical evidence for their assertions, attempting to discern which of them may offer sound support for resolution of the points under discussion.
To award the different studies a level of scientific evidence (SE), we used the basic concepts of Guyatt, formulated at McMaster University; criteria from the Journal of Bone and Joint Surgery, in its American version; and criteria from Clinical Orthopaedics and Related Research. These evidence levels have also been recommended recently by the Revista Española de Cirugía Ortopédica y Traumatología [Spain's Journal of Orthopaedic Surgery and Traumatology]. The type and level of SE for each article was awarded in relation to its main hypothesis or hypotheses and is shown at the end of its citation in the references.
As shown below, very few studies on this subject were awarded an SE level I or II, these being the ones that may be considered necessary and sufficient to validate an argument. Perhaps this is not all there is to it, however; perhaps SE means more than just randomised, prospective studies with a control group; meta-analyses; and a P of <.05. Well-designed, prospective studies with large cohorts painstakingly followed; data from arthroplasty registries or large-volume sources; and systematic literature reviews are valid tools when they are properly analysed.
In any case, the problem is not a simple one. It is a multifactorial complication, which means there is no simple approach to studying it. There is also a very wide variety of materials used. To complicate matters further, it is important to bear in mind that it takes more than 3720 primary THRs to detect a 2% effect on the factors involved in its dislocation.5 Another example of this conflict is a randomised comparative study in which 130 cases per group were required to detect a difference of 3 times in the incidence of dislocation, preventing a type II error (α 0.05 and β 0.8 using a historical rate of 1%).6 Thus, very high figures are required, which means there are not very many high-calibre studies.
In our review, along with studies that had large series, we also included articles in which an attempt was made to reach conclusions—even though, in terms of SE, the quality of the studies was not high enough to validate the conclusions. Comparing these 2 categories will enable us to outline a solution for the classical controversies—highly desirable information when what we are addressing is the best approach to and treatment for this complication.
IncidenceHistorically, the incidence of THR dislocation has ranged from 0.5% to 9.2% in patient series, as shown in a certain review (Table 1).7 The problem is the heterogeneity of population samples and study designs; for example, a study may consider only primary arthroplasty or it may count dislocations subsequent to both primary THR and revisions.8,9 In our country, an incidence of 2.97% was reported in a low-friction, cemented THR series.10 Of these, 33% were attributed to component malpositioning; 34% to soft tissue insufficiency; 26% to a combination of these 2 factors; and the remaining 7% to ill-defined causes—what Dorr et al.11 refer to as “postural” or “positional” causes in proposing this aetiological classification.
Incidence of dislocation according to various authors.
| Author | Year | Incidence of dislocation (%) |
| Charnley7 | 1972 | 1.5 |
| Eftekhar7 | 1976 | 0.5 |
| Ritter7 | 1976 | 1.4 |
| Fackler and Poss7 | 1980 | 2.4 |
| Robinson7 | 1980 | 4 |
| Ali Khan7 | 1981 | 2.1 |
| Woo and Morrey7 | 1982 | 3.2 |
| García-Cimbrelo10 | 1992 | 2.97 |
| Turner41 | 1994 | 4.5 |
| Paterno9 | 1996 | 6 |
| Ekelund45 | 1999 | 9.2 |
| Fender8 | 1999 | 5 |
| Jolles12 | 2002 | 1.5 |
| Phillips14a | 2003 | 3.9 |
| Mahomed18a | 2003 | 3.1 in primaries, 8.4 in revisions |
| Sharkey17 | 2004 | 0.1 in primaries, 1.4 in revisions |
| Gava15 | 2005 | 2.8 |
| Biedermann16 | 2005 | 2.4 in primaries, 4.6 in revisions |
| Hartman and Garvin19 | 2006 | Septic revisions×4 aseptic revisions |
| Azodi13a | 2008 | 2.5 |
| Blom7 | 2008 | 3.4 in primaries, 8.1 in revisions |
Fluctuations are also seen in recent series, with a certain reduction in the incidence of dislocations12,13 ranging from 2.5% to 3.9% in 2 studies with SE level II.13,14 In a series of cementless THRs in Spain, the incidence of dislocation observed was 2.8%.15 It seems clear that the percentage of dislocations is significantly greater following revision surgery than after a primary THR.16,17 In a SE level II study similar to the one cited above, the incidence of dislocation was 3.1% for primary surgery and 8.4% for revisions.18 If this revision surgery was done for an infection in the prosthesis, the incidence is multiplied by 4.19
ConclusionIn 2 SE level II studies, an incidence of 2.5–3.9% is reported for dislocation following primary THR13,14—figures that more than double following revision surgery.18
Significance of this complicationIt is the complication most frequently reported in the first 90 days post-THR.20 Between 1975 and 2005, it was the second most frequent reason for reintervention in THR, ranging from 11% to 15% of all reinterventions,21,22 but during 2005–2006, it achieved the dubious honour of being the main reason for reintervention in 22.5% of these cases.23 At a referral centre that takes THRs requiring revision surgery, reinterventions secondary to dislocation represented 9% of the total between the years 1986 and 1991, increasing to 35% between 1992 and 1995 and up to 42% between 1997 and 2001, thus representing almost half of all reinterventions.24
Mortality for patients who suffer at least 1 dislocation of their THR is significantly greater (P=.001) than for patients whose THR is stable, and this is true for both females (P=.002) and males (P=.02) as well as for patients who undergo THR secondary to rheumatoid arthritis (P=.008) or hip fracture (P=.03).25
The financial impact of this complication, when treated via closed reduction, is an increase of 10–20% over the cost of the primary THR, while revision of an unstable THR means a 150% increase in cost compared to the primary THR.26,27
ConclusionTwo SE level II studies show that dislocation is the most common complication in the first 90 days following prosthesis implantation20 and the main reason for reintervention in THR.23
“Instability” and “dislocation”It would be good to define these 2 concepts correctly, for they are sometimes erroneously used interchangeably. Dislocation is the complete loss of contact and relationship between the articular surfaces. The acting force, which derives from an excessive range of motion where joint surfaces remain in close relationship, overcomes the resistance provided by joint morphology and the restriction provided by the surrounding soft tissues. As with normal joints, this may result from a traumatic event delivering a strong force, or—as is typical in the circumstance we are addressing—it may be the culmination of unstable conditions in the arthroplasty, with previous dislocations that are potentially dislocatable, though never fully dislocated, or doomed to recurrent dislocation, more because of the instability than the force applied. Subluxation, on the other hand, is defined as any feeling of incomplete dislocation. This may occur with the hip flexed more than 90°, with or without internal rotation, and the knee higher than the hip in the transverse plane, or with the hip hyperextended, with or without external rotation, the knee extended, and the foot behind the hip in the frontal plane.28 This situation, which does not require unusual or extreme circumstances and can arise in the course of activities of daily living, is syncopal and transient and, as a rule, followed by the full restoration of normality.
Some authors29 state that, while THR has a 9% incidence of dislocation, 22.5% may show a certain degree of instability. In patients who have had epidural anaesthesia, an axial instability and subluxation of the prosthesis were detected on X-ray in 3% of cases within the first 6 months after surgery. Of those subluxations, 7% resulted in a dislocation.
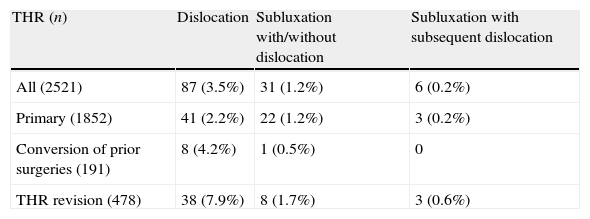
In an interesting though only SE level IV study by McGrory et al.,28 the incidence of subluxation was 1.2%, and occurring in 1.2% following primary arthroplasty; in 0.5% following conversion of prior THR surgeries; and in 1.7% following revision surgery (Table 2). Dislocations appeared in 3.5% of the total series, with an incidence of 2.2% following primary THR; 4.2% following conversion of prior surgeries to THR; and 7.9% following revision surgery. A closer look at the results of this study reveals that, in 81% of the subluxations, the THR was never completely dislocated; in 76% of these cases, the instability spontaneously resolved, while in the remaining 24% it persisted with 17% of these being revised, eventually, because of the instability. Of the 19% of subluxations that resulted in dislocation, 50% were revised. In summary, 13% of all cases of subluxation were surgically revised. From 1 to 109 months passed between the intervention and the first perceived subluxation episode, with an average of 27 months. The number of subluxation recurrences ranged from 1 to 20, with an average of 5.5 per hip.28
Incidence of unstable THR manifesting as dislocation and/or subluxation, from the McGrory et al. data.28
| THR (n) | Dislocation | Subluxation with/without dislocation | Subluxation with subsequent dislocation |
| All (2521) | 87 (3.5%) | 31 (1.2%) | 6 (0.2%) |
| Primary (1852) | 41 (2.2%) | 22 (1.2%) | 3 (0.2%) |
| Conversion of prior surgeries (191) | 8 (4.2%) | 1 (0.5%) | 0 |
| THR revision (478) | 38 (7.9%) | 8 (1.7%) | 3 (0.6%) |
THR: total hip replacement.
Returning to the subject of dislocation, the first episode occurred more than 2 years after surgery in 26% of cases,30 while this interval expanded to more than 5 years for 0.8% of cases.31 Some authors claim that progressive polyethylene wear in the acetabular core is the cause of this “late” instability.32,33 That is probably not the only reason for it, however; others who are concomitant, at least, should be added, such as reduced soft tissue tension and muscle tone as well as the changes in posture, coordination, and equilibrium that patients experience over time.
The cumulative risk for first dislocation is 2.2% in 1 year; 3% in 5 years; 3.8% at 10 years; and 6% at 20 years.34 Recurrence is 60% of primary THR dislocations7,35 and 70% of post-revision dislocations.7
ConclusionRegardless of interest in this subject, only an SE level II study can be the basis for sound knowledge. This study states that, in 0.8% of cases, episodes of late dislocation occur more than 5 years after implantation of the potentially unstable arthroplasty.31
Surgeon's experienceA 1997 article stated that, after adjusting the sample's demographic parameters, surgeons performing more than 50 THRs per year have a significantly lower incidence of dislocations than those performing no more than 5 per year (1.5% vs. 4.2%; P=.0001).36 Another study from that same year showed that the incidence of dislocations among the first 15 THRs performed is double the incidence seen after more than 30 have been implanted; from which point it then remains quite stable. The risk of dislocation is reduced to half for every 10 THRs performed per year.37
More recently, in 2001, Katz et al.38 also demonstrated that trend: the more THRs performed per year, the lower the incidence of dislocations. If 1–5 are performed per year, the incidence reaches 4.2%; for 6–10 per year, it is 3.4%; for 11–25 per year, 2.6%; for 26–50 per year, 2.4%; and if more than 50 are performed per year, the incidence of dislocation is 1.5%.
Two systematic literature reviews—the first in 2006 and the other, an SE level II, in 2007—confirmed the belief that the greater the surgeon's experience with hip replacement, the lower the risk of dislocation.39,40
This fact is also valid from the standpoint that the general experience acquired over time with this technique reduces the incidence of this complication. Epidemiological studies conducted using data from the Scottish National Arthroplasty Project 141 and from Medicare patients42—both SE level II—clearly demonstrated this reduction in the incidence of THR dislocations across very broad, relatively closed, and controllable population samples who were followed over a long period of time. In the first of these series, the incidence of dislocations dropped from 1.9% in 1996 to 0.5% in 2004,41 while in the second it fell from 4.21% in 1998 to 2.14% in 2007; the reduction in incidence seen during 2004–2007 was significant (P<.01) in comparison with that seen during 1998–2003.42
ConclusionThe SE level II studies cited affirm that more extensive experience on the part of the surgeon causes the incidence of post-THR dislocation to decrease40—a reduction also seen as general experience with this technique increases over time.41,42
Demographic considerationsHistorically, certain patients have been thought to be more at risk for dislocation of their THR. Taking into account the bias involved in the makeup of the population sample in these series, the incidence of dislocations has been observed to be higher in women than in men. For example, in a study with 561 patients, of whom 346 (61%) were women and 215 (39%) were men, there was a total of 25 dislocations—19 among the women (76%) and 6 among the men (24%).43 This difference has been shown to be significant in several studies (P<.02 and P=.007, respectively),34,44 one of them being an SE level II study.44
Age appears to be an unfavourable factor in the incidence. There is a significant difference (P<.003) between patients over 70 and patients under 70 years of age,34,44 one study being an SE level II,44 and also in populations over 80 years of age, with an incidence of 2.91%, compared with 1.48% for the total population (P=.005).12
Regarding indications for THR, there are 2 circumstances that carry a particular risk when compared with osteoarthritis. The incidence of dislocation in THR for a fracture is 14%, compared to 4% for osteoarthritis45—significantly greater (P≤.001) in SE level II studies.44,46 Another indication, such as the inflammatory arthritises, shows a 10% incidence of dislocation compared with 3% for osteoarthritis (P≤.007),34,47 the latter being an SE level II study.47 In another series,48 rheumatoid arthritis was also an unfavourable circumstance in this regard compared to other reasons for the intervention (P<.01).
Obesity has been cited as a predisposing factor in THR dislocation. Individuals whose body mass index is above 30kg/m2—the criterion for defining obesity—suffer 3.6 times more dislocations than those who are below this limit (P=.006), according to an SE level II publication.13 In another study with the same SE level, dislocation was 2.3 times more common in obese patients; sorting these patients by gender that figure is 3% for women and 1.8% for men,49 in keeping with the trend previously described. Similarly, regarding post-revision dislocation of the THR, the incidence of dislocation in obese patients is 19%, compared to 3% for the non-obese (P=.012).50
Another parameter to bear in mind is the patient's general condition pre-operatively. Patients classified ASA 3–4 suffer approximately twice as many dislocations as those classified ASA 1–2 (P≤.031),12,44,48 according to one of these SE level II studies.44
Alcohol represents an additional risk factor in connection with the intervention. There is a 23% incidence of dislocation associated with high consumption, compared to 5% for patients whose consumption is low (P=.00005).9
Mental and cognitive impairment has also been found to be an unfavourable factor in terms of the incidence of dislocation, this being 13% for patients with these impairments vs. 3% for healthy patients (P=.003)51; one SE level II study reported an incidence 2.5 times higher in the former than in the latter.52
Lastly, there is the very broad and diverse array of neuromuscular impairments; cases in which THR was performed on these patients are very few, and no negative impact of these impairments on susceptibility to THR dislocation could be found.53
ConclusionAccording to SE level II studies, women are more susceptible to THR dislocation,44 as are patients over 70 years of age,44 those with previous fractures,44,46 those with inflammatory arthritises,47 those whose body mass index is above 30kg/m2,13,49 those classified ASA 3–4 pre-operatively,44 and those who have mental impairments.52
Surgical approachThis is one of the aspects of this complication that is most discussed and appears regularly in the literature. Traditionally, it has been acknowledged that the posterior approach carries a much greater risk of dislocation than the other approaches. According to one systematic literature review,54 for instance, the posterior approach is the leader in frequency of this complication, with an average incidence of 3.23%, followed by the anterolateral approach with 2.18%, the transtrochanteric with 1.27%, and the direct anterior with 0.55%. Unfortunately, the studies from which these figures were taken do not have an adequate SE level, and various factors that introduce bias and distort the results most likely were mixed in with them. On the contrary, 2 SE level II studies exploring how surgical approach affects the incidence of dislocation conclude that the posterior approach is associated with no more dislocations than other approaches.55,56
As we have stated, this is a multifactorial problem. For example, analysis of the surgical approach in relation to pre-operative range of motion in the hip has confirmed an association between the posterior approach and patients whose range of motion in the hip is 115° or more. Patients who have that range of motion suffer dislocations at a rate of 5.6%, compared to 3.1% for patients with less range of motion (P=.007).57 The posterior approach is also less secure than the anterolateral for implanting a THR in cases where there has been a previous fracture. Compared to an 8% incidence of dislocations in these patients when a posterior approach is used, it is 2% with an anterior approach (P=.01),58,59 and it should be mentioned that Enocson et al. is an SE level II study.58 Therefore, in patients such as those described, surely it is better to choose an approach other than the posterior.
ConclusionAccording to SE level II studies, the posterior approach involves no greater risk of dislocation than other approaches,55,56 but this approach should be used with caution in cases where there has been a previous fracture.58
Minimally invasive techniqueThe debate between minimally invasive surgery and conventional surgery in this circumstance has been fully resolved. Counter to any given author who finds that there are more dislocations with a minimally invasive approach,60 there is a great abundance of literature confirming just the opposite—whether it is SE level I–II61–64 or of lesser calibre.65–67
ConclusionThe advantages and convenience of minimally invasive techniques in hip arthroplasty could be discussed; in view of the level I and II SE; however, no one can claim that these techniques render the patient more susceptible to dislocation.61–64
Arthroplasty design and friction coupleThis is another key point in the literature, and it is particularly difficult to analyse the results because none of the studies has a high enough SE level to be able to support any given opinion. Certain authors insist that this parameter has no effect on one way or the other on the incidence of dislocations.48,68,69 Others, however, point out that a friction couple with a diameter of 36mm is more stable than a 32-mm or 28-mm head and significantly more stable than a 22-mm head.70–72 In studying the dislocation-free survival of THRs with an articular couple diameter of 28mm and 32mm, Amlie et al. found a significantly greater 8-year survival rate (P<.001) for prostheses of larger head size.73 This corroborates the trend reported in the Norway Registry data: a 12-year, dislocation-free survival rate 4 times greater for THRs with a 36-mm head than for those with a 28-mm or 22-mm head.74
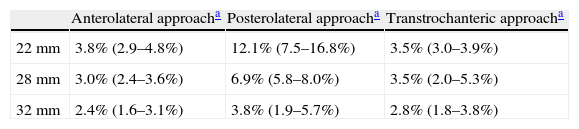
The combination of articular couple diameter and surgical approach is also of interest here. Morrey26 believes there is no connection between these factors and the incidence of dislocation. In contrast, Berry et al.34 found a significant difference in the incidence of dislocations in favour of the anterolateral compared to the posterior approach (P<.0001) and in favour of the 32-mm diameter couple compared to the 22-mm (P<.0001). Analysing how these 2 factors interact, they observed that the friction couple diameter is of no consequence if the approach is anterolateral or transtrochanteric, but with a posterior approach, a 28-mm or 32-mm head provides significantly greater stability than a 22-mm head (Table 3).
Analysis of the incidence of THR dislocations in relation to the articular couple diameter and the surgical approach used for their placement.
| Anterolateral approacha | Posterolateral approacha | Transtrochanteric approacha | |
| 22mm | 3.8% (2.9–4.8%) | 12.1% (7.5–16.8%) | 3.5% (3.0–3.9%) |
| 28mm | 3.0% (2.4–3.6%) | 6.9% (5.8–8.0%) | 3.5% (2.0–5.3%) |
| 32mm | 2.4% (1.6–3.1%) | 3.8% (1.9–5.7%) | 2.8% (1.8–3.8%) |
THR: total hip replacement.
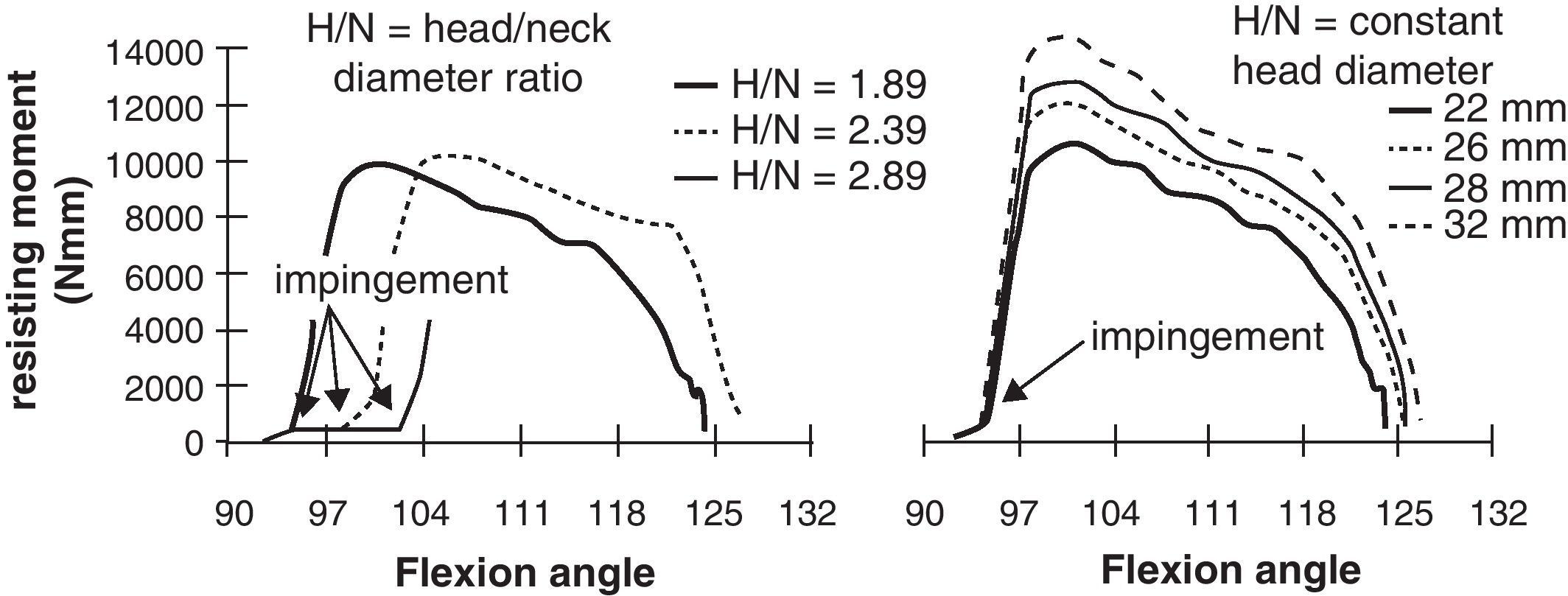
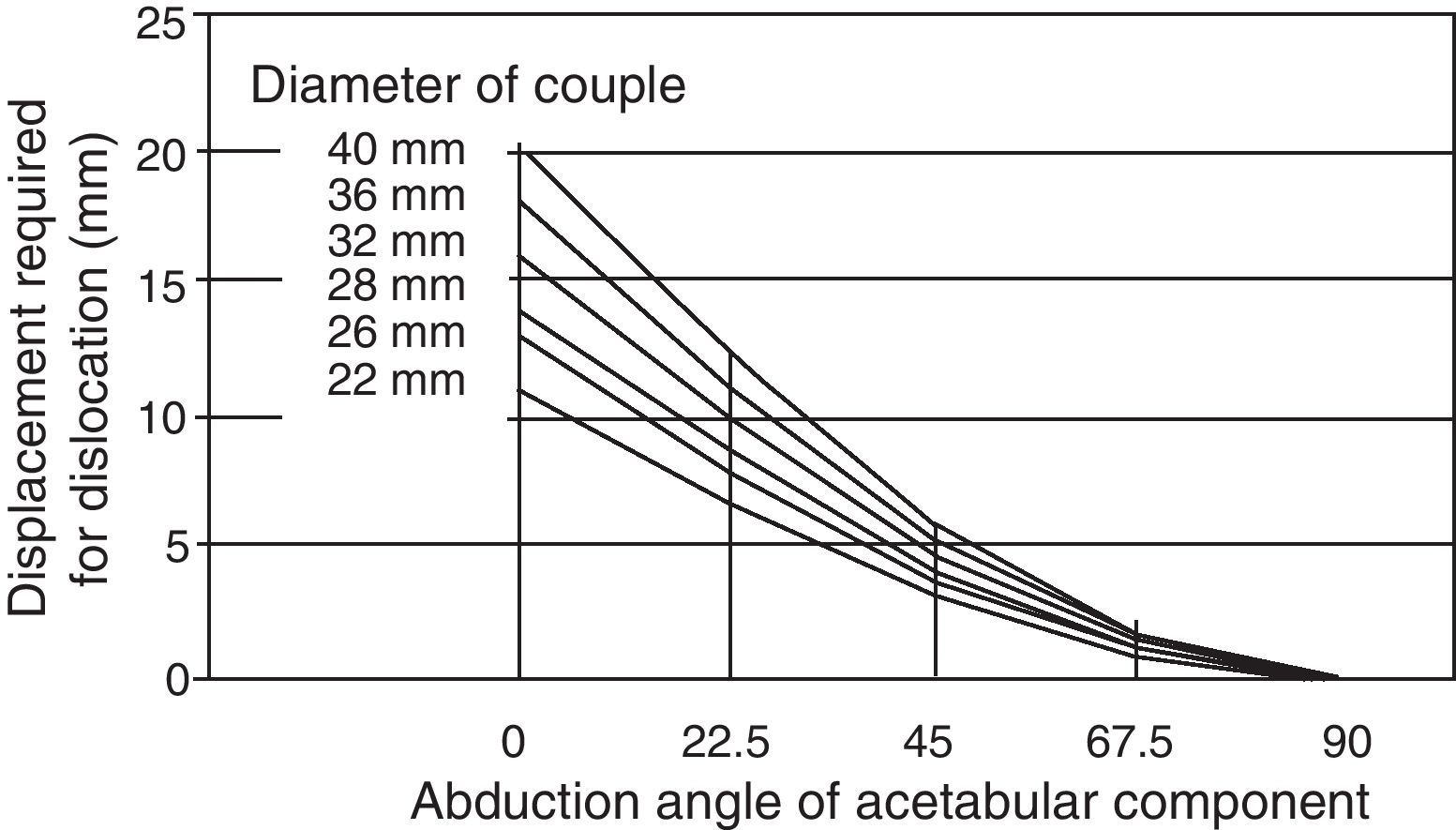
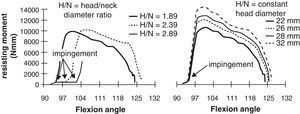
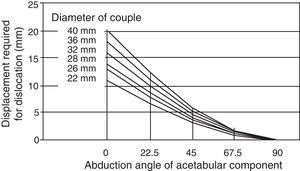
However, like many others, this is a retrospective study with a rather heterogeneous series, and it does not take into account the head diameter to femoral neck dimension ratio—another aspect that has been widely discussed. In effect, a wide circular neck cross-section resulted in 3 times the number of dislocations as a design with narrow trapezoidal neck cross-section.75 Femoro-acetabular impingement is the underlying mechanism causing a dislocation; the higher the head diameter to neck cross-section ratio, the more belatedly it occurs at higher degrees of flexion (Fig. 1). If this ratio remains constant, the resisting moment against dislocation is greater for a 32-mm head,76 which would explain the differences in the incidence of dislocation when exactly the same diameter head is used with all the different rod models.43
The greater the femoral head diameter to neck cross-section ratio, the later the femoro-acetabular impingement seen at higher degrees of flexion occurs. If this ratio remains constant, a large-head friction couple is better because it makes the resisting moment against dislocation greater.
The good performance of double-mobility or tripolar arthroplasties in terms of stability may also be due, at least in part, to this advantage of the high head diameter to neck cross-section ratio. While in conventional prostheses that ratio ranges from 2.29 to a maximum of 3.4, in tripolar prostheses it is as high as 4.7, which minimizes the chance of impingement of the femoral neck on the edge of the acetabular component.77 That is the theory, at least. In fact, in the literature, where a tripolar model has been used to treat an unstable THR, dislocation recurs in as many as 7–19%; an additional 21% incidence for other types of failures makes the results with these models considerably worse.78
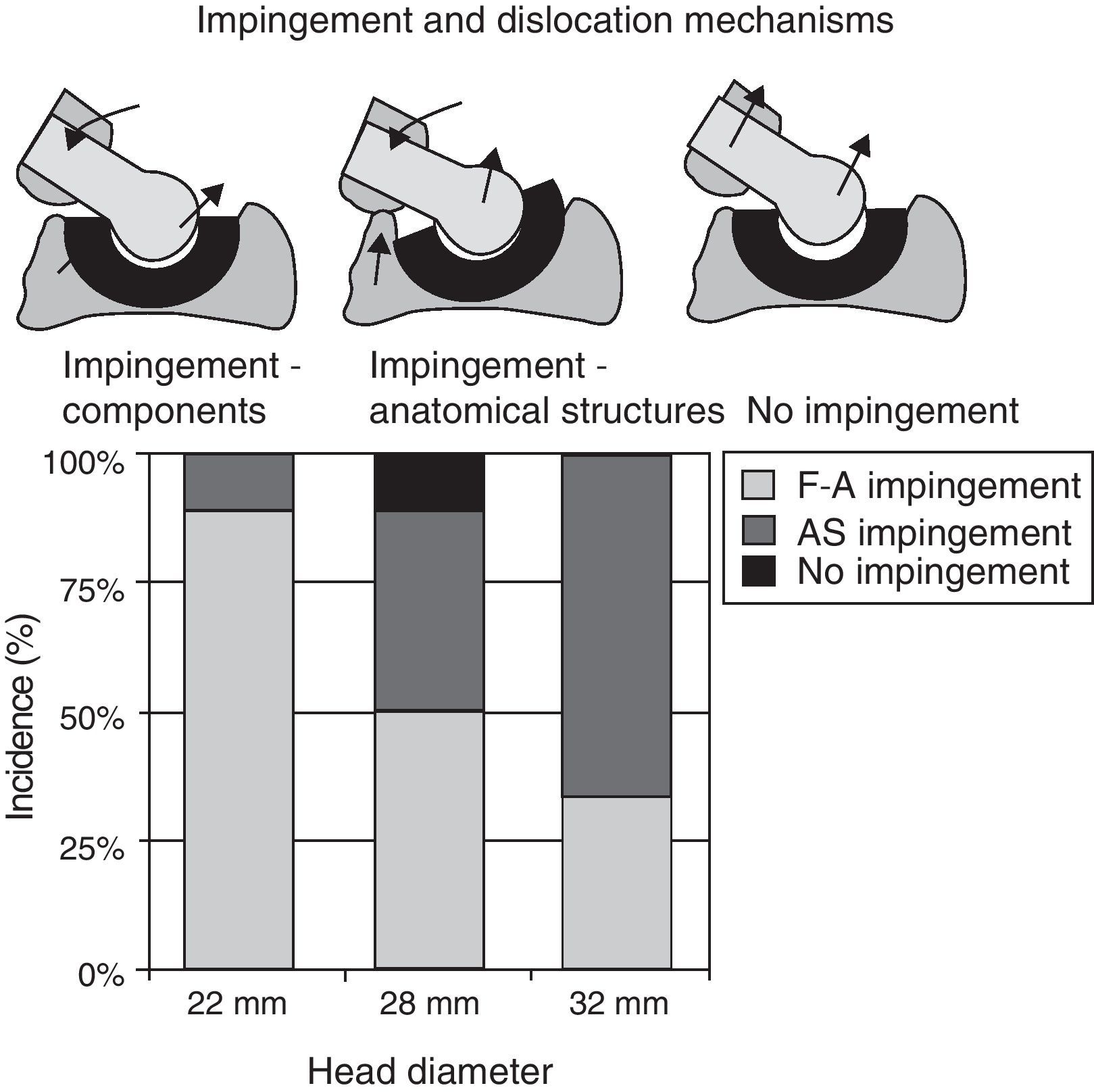
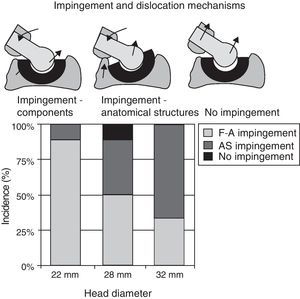
There are some limits to increasing the head diameter to neck cross-section ratio. On the one hand, resistance may be compromised in the neck so that it suffers a fatigue fracture, which is completely undesirable. On the other hand, as head diameter increases—leaving aside the tribological considerations that must be raised—the incidence of impingement between prosthetic components decreases, but the chance of impingement between anatomical structures increases; this being another way that THR dislocation may occur.79 In the Bartz et al. experimental study,5 the primary mechanism of dislocation in a THR with 22-mm head was impingement between prosthetic components; however, with a 32-mm head, the impingement was between anatomical structures—basically, the lesser trochanter and the ischium (Fig. 2).
On the subject of joint stability and femoro-acetabular impingement, consideration must be given not only to the parameters analysed so far but also to the design and outside dimensions of the acetabular component. It stands to reason that the more enveloping the acetabulum, the more stable the articular couple; however, there is less mobility, more cup-neck impingement, and greater compromise of the components-to-bone fixation. The risk of dislocation drops significantly if the edge of the acetabular component is elevated 15° in the assumed direction of dislocation.70,80 It is better for the edge to be flat with a wide bevel.81
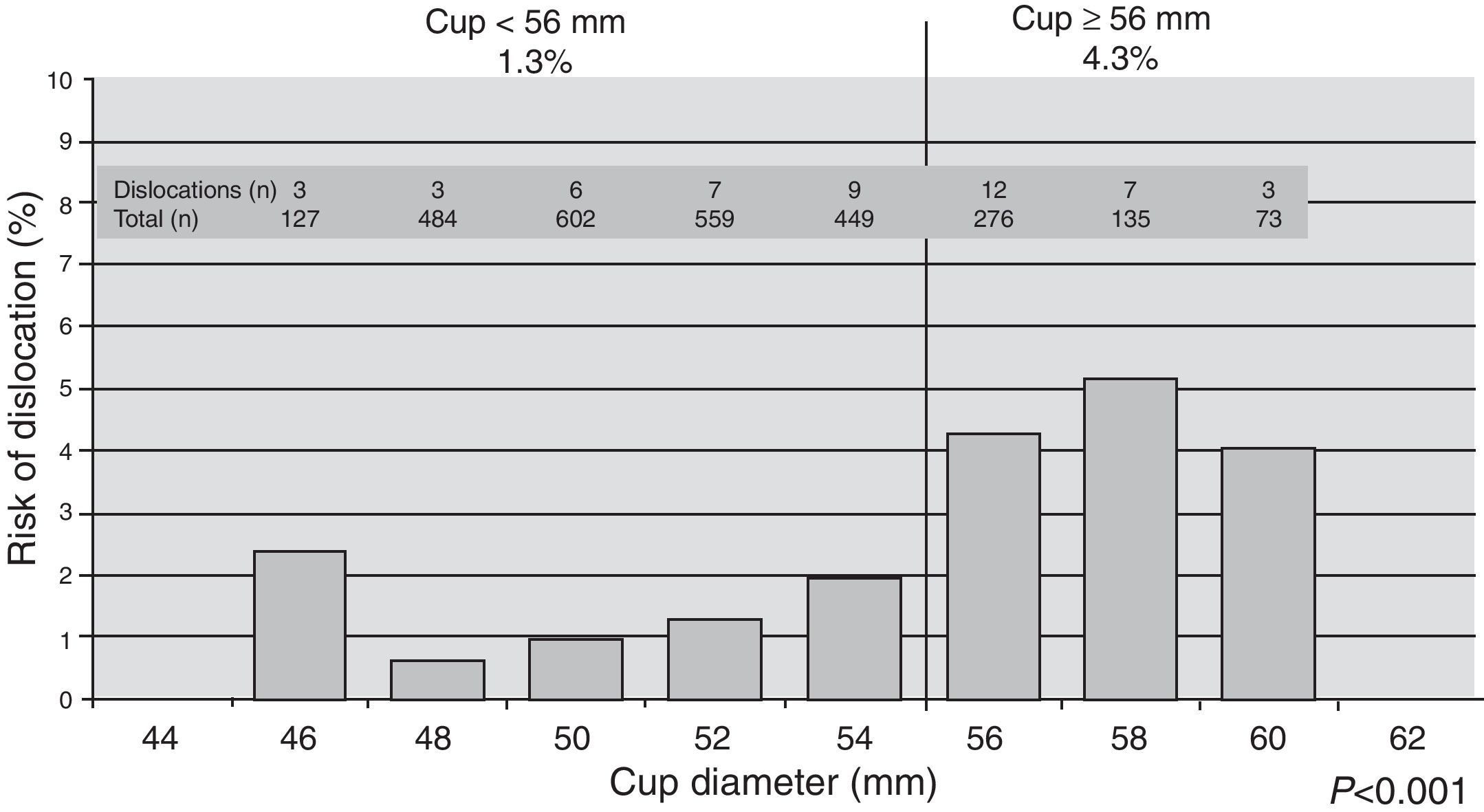
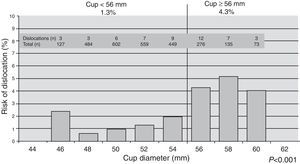
Regarding the outside diameter of the acetabular component, a classic 1998 study highlights that THRs with an acetabular component outside diameter of at least 62mm would suffer 3 times the dislocations of those with an acetabulum whose outside diameter was not more than 60mm (P=.043).82 This assertion is validated in an SE level II study showing that, for a 28-mm articular couple, the risk of dislocation is significantly higher when an acetabulum with outside diameter of at least 56mm is used (P<.001)—double that seen when the outside diameter is less than 56mm (Fig. 3).83
Influence of the outside diameter of the acetabular component on the incidence of THR dislocations.
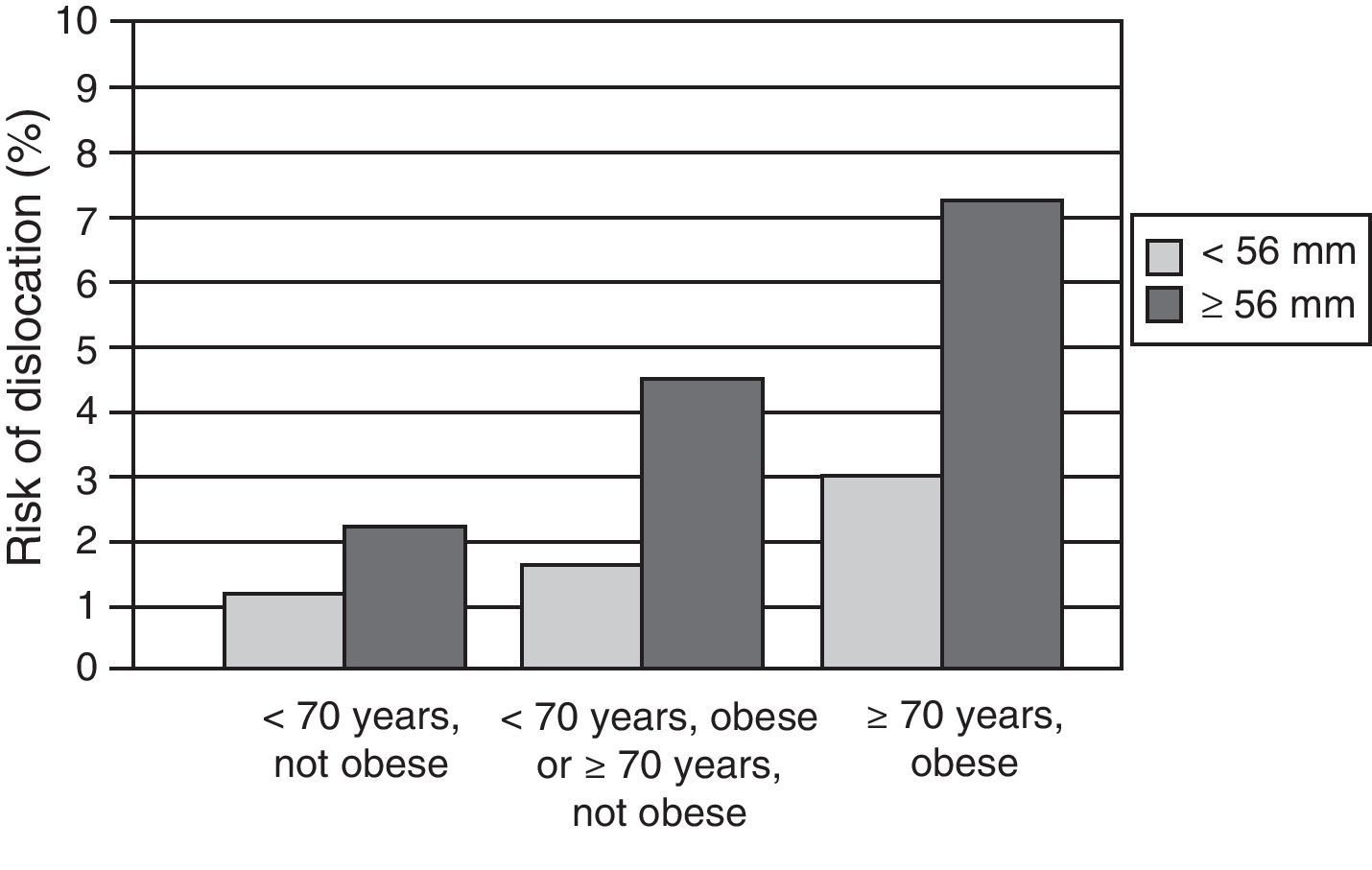
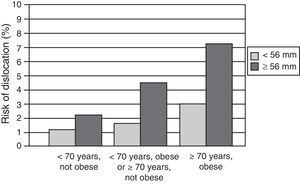
Relating this parameter to patient age and obesity status reveals that, when acetabular components with outside diameter of 56mm or more are used in patients over 70 years of age whose body mass index is above 30kg/m2, there are 12 times more dislocations, the incidence being 7.5% in these cases, compared to the 0.6% reported when an acetabulum smaller in outside diameter is used in patients under 70 years of age whose body mass index is less than 30kg/m2 (Fig. 4).83
Unfavourable combination in terms of the incidence of dislocations with a 28-mm-diameter head: acetabular component diameter of 56mm or more, patient over 70 years of age, body mass index of 30kg/m2 or more.
Although these aspects continue to be highly controversial, SE has been obtained through a single level II study showing that, with an articular couple 28mm in diameter, an acetabular component with outside diameter of 56mm or more favours impingement and dislocation. This situation is particularly dangerous in patients who are obese or over 70 years of age.83
Orientation of the componentsAlthough it seems obvious that the opposite is true, there are authors who argue that the orientation of the implant is of no consequence in terms of the chances of dislocation.9 It is not the only factor, of course, because dislocations may also occur in properly oriented THRs; however, gross malpositioning surely would have some effect. Biedermann et al. found that 93% of stable THRs in their series and—even more noteworthy—67% of unstable THRs16 were within a safe zone for cup placement of 15±10° of anteversion and 45±10° of abduction.
In their classic study, Lewinnek et al. showed that there is a 1.5% incidence of THR dislocation when the acetabulum is placed within a safe zone of 15±10° of anteversion and 40±10° of abduction, while the incidence is 6.1% when it is not placed within these limits.84 Likewise, other authors report a significant increase in this incidence when abduction of the acetabulum is 50° or more (P=.001) or when anteversion is 5° or less or 20° or more (P=.02).15 If the cumulative acetabular and femoral anteversion are less than 40° or more than 60°, there is a 7 times greater risk of dislocation.12 In an SE level II study, there was a significant increase in dislocations (P<.02) with abduction of the cup and/or greater ante- or retroversion of the acetabular component and/or greater ante- or retroversion of the femoral component.44 Generally speaking, component malpositioning is the major cause of dislocation found in the literature—if not its appearance, then its recurrence.85
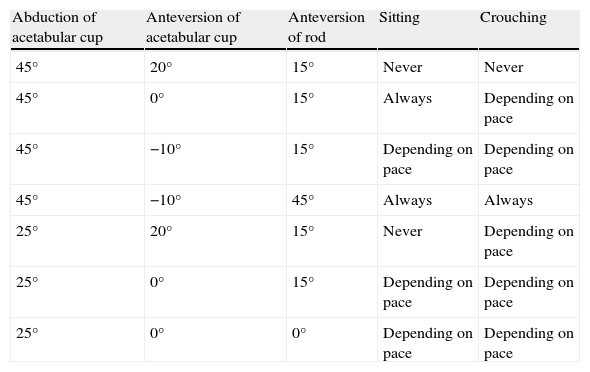
Daily activities may prove to be destabilizing to the prosthesis, depending on how its components are oriented. In an experimental study, Barrack et al.86 checked the stability of the prosthesis during different activities, such as sitting down and crouching, according to how the prosthetic components were placed. There was no risk of femoro-acetabular impingement with these activities when the acetabulum was at 45° of abduction and 20° of anteversion and when the rod was at 15° of anteversion. If, however, with the acetabulum at 45° of abduction, the cup was at 10° of retroversion and the femoral rod at 45° of anteversion, then impingement always occurred when these activities were attempted. With a different component orientation, the occurrence of impingement during these activities is variable, depending on the pace at which the activity in question is performed (Table 4).
Femoro-Acetabular impingement in different activities according to orientation of the prosthetic components.86
| Abduction of acetabular cup | Anteversion of acetabular cup | Anteversion of rod | Sitting | Crouching |
| 45° | 20° | 15° | Never | Never |
| 45° | 0° | 15° | Always | Depending on pace |
| 45° | −10° | 15° | Depending on pace | Depending on pace |
| 45° | −10° | 45° | Always | Always |
| 25° | 20° | 15° | Never | Depending on pace |
| 25° | 0° | 15° | Depending on pace | Depending on pace |
| 25° | 0° | 0° | Depending on pace | Depending on pace |
Impingement occurs between prosthetic components or anatomical structures in most daily activities involving hip flexion, while in activities that involve extension of the hip, impingement may occur with the acetabulum at 45° of abduction and 20° of anteversion. The cup must not, by any means, be allowed to extend more than 5mm in front of or behind the bony anatomical acetabulum, whether because of incorrect positioning or because of excessive size or outside diameter.87 So it is very important to accommodate the specific range and sequence of movements for each activity.
Improper orientation of the acetabular cup may cancel out the advantage of using a large-diameter articular couple (Fig. 5).88
Excessive abduction of the acetabular cup cancels out the advantage of a large articular couple over a small one in terms of stability.
Computer-assisted surgery guarantees a placement that is more accurate and reproducible with less variability in the orientation of prosthetic components. On a positive note, a systematic literature review reveals that there is a significant reduction (P=.03) in the incidence of dislocations for THRs performed with surgical navigation—1.03%, down from a 2.49% incidence with conventional THR procedures.89 It is acknowledged, then, that better orientation of the arthroplasty is possible with navigation, with fewer cases outside the safe zone; as it turns out, however—paradoxically and despite all of this—the incidence of dislocations in navigated THR is similar to that seen in non-navigated procedures, as verified by 2 SE level II studies.90,91
Another option complementary to orientation is modularity. An anteverted modular neck prevents anterior femoro-acetabular impingement in those activities mentioned that involve hip flexion, while a retroverted neck prevents posterior impingement in activities involving hip extension. One or the other neck may be chosen for use, depending on the orientation of anatomical elements in the transverse plane, the patient's priority activities, and the direction in which there is risk of dislocation. In fact, the use of an anteverted or retroverted neck is reported in 27.8% of female patients and 21.6% of male patients, reducing the incidence of dislocation to 0.7%.92
Modularity does not appear to be effective in reducing the incidence of dislocation in THR revisions, however.93
ConclusionThe proper orientation of prosthetic components results in a reduced incidence of dislocations, according to an SE level II article.44 Two other studies, also SE level II, demonstrate that navigation facilitates precise orientation and reduces the number of extreme cases outside the safe zone but does not reduce the number of dislocations.90,91
Constituent materials for the articular coupleClarke et al.,94 in a combination experimental and clinical study, consistently report that the force required to separate the articular components in a metal–metal couple is 24N, compared to the 1.9N required to separate a ceramic–polyethylene couple. Their explanation for this is that the metal–metal interface has a stronger adhesive force owing to the interposition of a thin film of lubricating fluid. This finding translates clinically to a 0.9% incidence of THR dislocation for a metal–metal couple 28mm in diameter, compared to 6.2% for a ceramic–polyethylene couple of the same diameter.
In contrast, other studies95–97—two of which are SE level II95,97—show no advantage of metal–metal contact over metal–polyethylene or ceramic–ceramic.
On this subject, one question remains: could dislocation of a metal–metal, large-head prosthesis be indicative of a tissue reaction to the metal? The extensive soft tissue swelling seen in these cases could be a cause of dislocation of the prosthesis.98
ConclusionTwo level II studies provide SE that the constituent materials of the articular couple make no difference in the higher or lower incidence of dislocations.
Soft tissue reconstructionAs previously mentioned, one of the causes of a THR dislocation is the loss of tension in periarticular soft tissues. Whatever may alter this tone increases the risk of dislocation. A loose greater trochanter increases this risk significantly (P<.001).70
It is also important to remember that a larger-diameter couple cannot compensate for the instability due to a deficient hip abductor mechanism.99
However, the critical point in this section—the point that closes the circle as to which approach causes more dislocations—is that, at the end of the procedure, the elements through which the hip has been accessed be repaired, specifically and particularly in the case of a posterior approach. Here, a serious discrepancy arises that continues to this day, as yet unresolved.
On the one hand, there are authors who find that repairing is unquestionably superior to abstaining, with dislocations ranging from 4% to 6.2%, if the posterior elements mentioned are not repaired, and 0–2.2% if they are repaired,44,100,101 2 of these studies being SE level II.44,101 The advantage of repairing is also appreciated in 2 systematic literature reviews,102,103 where an 8 times higher incidence is reported for a posterior approach without repair, whereas, with repair, the incidence is similar to that for the anterolateral and direct lateral approaches.103
The experimental efficacy of repairing the posterior elements has been demonstrated in a study by Elkins et al.104 It has also been possible, through an ultrasound study, to confirm that the repair retains its integrity 3 months after the procedure.105
The controversy remains alive; however, thanks to an SE level II study showing that repairing the posterior elements has no effect on the incidence of dislocations, this being 12% without repair and 14% with repair.58
ConclusionGiven the contradictory results from different high-calibre studies with sufficient SE level, there can be no verification of a correlation between dislocations and reconstruction of the soft tissues damaged through the surgical approach.
The efficacy of preventionAs previously mentioned, there is a greater or lesser risk of prosthesis dislocation with daily activities depending on how they are carried out. In this regard, an SE level II study confirmed the efficacy of an educational program prior to the arthroplasty surgery, the incidence of dislocations being 2.8 times lower in patients who followed it than in those who did not (0.8% vs. 2.1%).106 So risky situations must be avoided—among them, having impromptu sex. There are published guides on positions for enjoying sexual activity safely starting in the third post-operative month.107,108
The use of mobility restrictors, abductor cushions, seat elevators, and the like is usually indicated and encouraged during the first 6 weeks to limit flexion to less than 90°, limit rotation to less than 45°, and limit adduction; however, these have been shown in 2 SE level II studies to be completely ineffective.6,109 Abduction splints have also been revealed to be ineffective in preventing recurrence following closed reduction of a THR dislocation.110
ConclusionPre-operative education instructing the patient how to carry out daily activities is effective in reducing the risk of dislocation,106 but the use of hip mobility restrictors has been shown to be ineffective.6,109
Efficacy of the treatmentThe efficacy of treatment is closely tied to the cause of the dislocation. The “postural” or “positional” dislocations described by Dorr et al.11 respond well to closed reduction, 45% of cases being resolved without recurrence. In the remaining 55% of cases, there is a recurrence requiring subsequent surgical treatment. Although closed reduction should be the treatment of choice in all cases, its efficacy in the other 3 categories is rather limited, surgery being required in 71% of cases where component malpositioning is detected and in 83% of cases in each of the other 2 categories, with approximately 1/3 of cases included in the last 3 categories requiring more than 1 intervention.111
When there is dislocation of a THR performed for previous fracture or rheumatoid arthritis, the risk of revision is higher than it is with a THR for osteoarthritis (P<.001 and P=.006, respectively). The frequency is also significantly higher (P<.001) if a 22-mm head is used instead of a 32-mm head and if an uncemented cup is implanted instead of a cemented cup (P=.02).112
Many methods have been proposed for resolving a THR dislocation that is recurrent and cannot be stabilized using conservative measures.113 It is necessary to stress that dislocation recurs in 60% of primary arthroplasties and at a rate of 70% when it happens in a revision. Of the dislocations that occur in primary THRs, 33% end up being re-operated; following a revision, that figure rises to 50%. After surgical revision of an unstable prosthesis, it becomes stable in 70% of cases, if it was a primary THR that dislocated, and in 50% of cases, if the dislocation happened following a revision.
Among the treatment options, soft tissue reconstruction and retensioning prevents recurrence in 47% of the cases in which it is done, whereas, if augments and restrictors are placed in the acetabulum, another dislocation is prevented in 82% of cases.114 Making use of the modularity of prosthetic components achieves stability in 45–77% of cases115,116 and in 71% of cases where a constrained acetabular component is used.117
The efficacy of constrained acetabular components is under discussion.118 Using them offers a rate of 17.5% for dislocations and 29% for recurrences when they are used in recurring dislocations.117 These absolutely unacceptable figures have been improved to 1.2% with a particular model of this type of acetabular component119; in a systematic literature review, however, the figure for dislocation of a constrained arthroplasty is 10% of cases.120
It should be clear to readers that treating an unstable THR with recurring dislocation simply by implanting a constrained acetabular component—without correcting the other reasons for the instability—results in a 16% failure rate due to dislocation of the implant.121
Replacing the components—especially when there is an obvious error in orientation—prevents recurrence in 67% of cases where there is a definite reason for the dislocation and in only 50% if the cause of the dislocation is unknown.114
Whatever the case may be and whatever the treatment used, stability is achieved in 95% of THR dislocation cases.122
ConclusionIn terms of treating recurrent dislocation, the advantage of one type of treatment over any other type cannot be established; it depends on a host of factors—in particular, the fundamental cause of the instability. What can be said regarding treatment is that there is only evidence that there is no evidence.123
Dislocation in other types of hip replacementsThe figure reported by Carrothers et al. for dislocations in resurfacing prostheses is 0.1%, and it appears that women are particularly susceptible to this complication, for all the patients who suffered it were female (P=.004).124
For partial prostheses, the incidence of dislocations reported in a systematic literature review was similar to that for THR.125 In the case of a cemented Thompson prosthesis, dislocation occurs in 3.3% of patients and appears more frequently with an anterior approach than with a posterior approach (P=.005).126
Conversion of these partial prostheses to a THR carries a 22% risk of dislocation—higher than the 10% rate of dislocations following revision of a THR (P<.02), in a comparative study.127
ConclusionThere is no SE sufficient to recommend a treatment regimen in these cases.
Change in clinical results following a dislocationThe patient with an unstable hip scores lower on the Harris evaluation system and is also very worried about the future of his/her arthroplasty.28
The score obtained on the WOMAC or SF-12 scale after a non-recurring dislocation in a primary THR is similar to that for a THR without this complication; however, the THR patient without dislocation tends to have a better quality of life, and patients whose implants dislocate tend to be less satisfied with their THR.128
One series analysed the Oxford Hip Score at a mean evolution of 5 years. In this study, the scores were 17.4 for the control group without dislocation; 26.7 for a non-recurring dislocation treated by closed reduction; 27.2 for non-operated recurring dislocation; 34.5 following successful surgical revision; and 42 following failed surgical revision. On the EuroQol-5 questionnaire,35 it was also found that patients undergoing revision for THR dislocation have more health problems.
ConclusionEven though, to a greater or lesser extent, dislocation compromises the results of a THR, there is no SE that demonstrates this.
Final considerationsWhat has been published in SE level I or II articles may be summarized as follows:
- 1.
THR dislocation occurs at a rate of 2.5–3.9%.
- 2.
The incidence is higher in revisions than in primary THRs.
- 3.
It is the most common complication in the first 90 days after the surgery.
- 4.
It is the primary reason for re-intervention on a THR.
- 5.
There is a late form of dislocation occurring 5 years or more after the implantation in 0.8% of cases.
- 6.
The surgeon's experience is a factor in the incidence of dislocations.
- 7.
Historically, a reduction of its incidence is observed.
- 8.
The risk of dislocation is greater in women, patients over 70 years of age, cases of previous fracture and inflammatory arthritises, obese patients, individuals classified ASA 3–4 pre-operatively, and patients with mental impairments.
- 9.
The posterior approach, in and of itself, does not result in more dislocations than the other approaches.
- 10.
The posterior approach is dangerous in cases with previous fracture.
- 11.
There is no higher incidence of dislocations when minimally invasive approaches are used.
- 12.
A large-diameter acetabular component increases the incidence of dislocations because it favours femoro-acetabular contact. This situation is particularly dangerous in patients who are obese and over 70 years of age.
- 13.
Proper orientation of the prosthetic components reduces the risk of dislocation.
- 14.
Navigation helps with accurate placement of the arthroplasty but does not reduce the incidence of dislocations.
- 15.
The constituent materials of the articular couple are not a factor in dislocation.
- 16.
Repairing the posterior elements is controversial in terms of clinical results.
- 17.
Pre-operative education instructing the patient how to carry out daily activities is effective in reducing the risk of dislocation.
- 18.
The use of restrictors or methods of reducing mobility in the operated hip are not effective in preventing dislocation.
- 19.
There is no SE by which efficacy can be established for different ways of treating THR instability.
- 20.
There is no SE indicating that THR instability compromises clinical results.
Evidence Level V.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Fernández-Fairen M, et al. Inestabilidad de la artroplastia total de cadera. Una aproximación desde los criterios de la evidencia científica. Rev esp cir ortop traumatol. 2011;55(6):460–475.