In recent years, the number of studies regarding newly-diagnosed food allergies after liver transplantation has been increasing. In this study, we aimed to investigate the frequency, aetiology, risk factors, and severity of IgE-mediated food allergies after liver transplantation in children.
MethodsPaediatric patients who underwent liver transplantation at Inonu University Faculty of Medicine, Organ Transplantation Institute were included in the study.
ResultsForty-nine paediatric patients were enrolled in the study; 26 (53.1%) were female, the median age at transplantation was five years, and median follow-up time after transplantation was 16 months. Six patients (12.2%) developed IgE-mediated food allergies after transplantation; four had urticaria and/or angio-oedema and two developed anaphylaxis after food intake. Patients with and without IgE-mediated food allergies were similar in terms of sex, age at transplantation, comorbid atopic disease, immunosuppressant therapy with tacrolimus, and blood tacrolimus level (p>0.05 for each). Serum total IgE levels ≥100IU/mL (p=0.02) and peripheral eosinophilia (p=0.026) were more common in the patients who developed IgE-mediated food allergies. In five of the six patients who developed IgE-mediated food allergies, reaction occurred within the first year after transplantation; the risk of developing a reaction was 2.7 times higher within the first year after transplantation than in subsequent years (95% CI, 1.546–4.914; p=0.026). No Epstein–Barr virus or cytomegalovirus infections were detected in any of the patients who developed IgE-mediated food allergies after liver transplantation.
ConclusionThe risk of developing IgE-mediated food allergies is approximately three times higher within the first year after transplantation than in subsequent years.
In recent years, the number of studies regarding the development of food allergies after solid organ transplantation has increased.1–3 These allergies can manifest in a wide spectrum, ranging from mild to life-threatening reactions, such as urticaria and anaphylaxis. Food allergies that develop after solid organ transplantation are most common after liver transplantation.2–5 While the pathogenesis is not well understood, tacrolimus, which is used in long-term immunosuppression to prevent tissue rejection, is thought to contribute to the development of food allergies. Tacrolimus affects intestinal barrier function and changes its permeability.6,7 As a result, food allergens permeate the intestinal barrier, facilitating susceptibility to food allergens. Tacrolimus also disrupts the Th1/Th2 balance towards IL-4, IL-5, and IL-13, the main mediators of allergies.8 However, recent studies have shown that the use of tacrolimus is not the only cause of food allergy after liver transplantation; young age at transplantation and the presence of comorbid atopic disease facilitate its development.9 The development of IgE- and non-IgE-mediated food allergies during the follow-up of paediatric patients who underwent liver transplantation has been reported in several studies. In the current study, we aimed to determine the frequency of IgE-mediated food allergy, the severity of the allergic reactions, and the risk factors in children who underwent liver transplantation.
Materials and methodStudy populationPaediatric patients who underwent liver transplantation at Inonu University, Faculty of Medicine, Organ Transplantation Institute between January 2008 and January 2013 were included in the study. The patients’ charts were reviewed and the data were collected after the study was approved by the ethics committee of Inonu University.
The patients who underwent liver transplantation were monitored regularly at the organ transplantation institute and paediatric gastroenterology clinic. During patient follow-ups after transplantation, blood immunosuppressant levels, complete blood cell counts, and liver function tests were examined regularly. In addition, the results of viral serology examinations, including Epstein–Barr virus (EBV) and cytomegalovirus (CMV), of all of the patients prior to liver transplantation were recorded. A questionnaire designed to evaluate the patients’ food allergies and other allergic diseases was prepared by an expert and completed during face-to-face interviews with the patients. The questionnaire included questions about patient demographics, the cause of liver failure, the duration of failure prior to transplantation, the age at liver transplantation, donor and donor affinity, donor history of allergic disease, chronic immunosuppressant therapy, symptoms of food allergy after transplantation, and the onset of symptoms after transplantation. The patients were questioned regarding symptoms of both pre- and post-transplant allergic disease. Patients who indicated IgE-mediated food allergy symptoms or who were diagnosed with IgE-mediated food allergies prior to the liver transplantation were excluded from the study.
DefinitionsPatients who described symptoms of allergic diseases (asthma, allergic rhinitis, atopic eczema, IgE-mediated food allergy, and drug allergy) were further examined in the allergy clinic to confirm the diagnosis. The peripheral blood eosinophil counts of all of the patients were measured. Skin prick tests and/or determination of serum-specific IgE levels were performed in patients who described IgE-mediated food allergy symptoms, and pulmonary function tests were performed in patients who described asthma symptoms. Oral provocation tests with food and drugs were performed on patients whose diagnoses of IgE-mediated food or drug allergies were still suspicious despite medical history and skin test results.
IgE-mediated food allergySensitivity in the skin prick test and/or serum-specific IgE levels in patients with early-type reactions such as urticaria, angio-oedema, and anaphylaxis after food intake were defined as IgE-mediated food allergy. Oral provocation tests with food were performed in patients whose diagnoses were uncertain or when needed. Eleven patients had a positive history and six patients were confirmed with IgE-mediated food allergies by oral provocation test. Serological testing for EBV and CMV was performed in patients who were diagnosed with food allergies.
The diagnosis of asthma was established according to the Global Initiative for Asthma10 guidelines; allergic rhinitis was diagnosed according to the Allergic Rhinitis and its Impact on Asthma11 guidelines, and atopic eczema was diagnosed according to the Hanifin and Rajka criteria12 based on medical history and clinical features.
Drug allergyPositive skin tests in patients who described early or late reactions after drug intake or reactions in oral drug provocation tests were defined as drug allergy.
Skin prick testing was performed using the prick reagent Alyostal® (Stallergenes, Antony, France) and prick-to-prick testing was performed with fresh foods. The investigated food allergens were cow's milk, hen's egg, banana, potato, lentil, beef, peanut, fish, and wheat. Histamine chloride and sodium chloride (0.9%) were used as positive and negative controls, respectively. Specific IgE against foods was measured by ImmunoCAP assay.
EosinophiliaPeripheral eosinophil percentage ≥4% was defined as eosinophilia.
Informed consent was obtained from the parents of all the participants. The study was approved by the Ethics Committee of Inonu University (approval number: 184/2013).
Statistical analysisStatistical analysis was performed using Statistical Package for Social Sciences 15.0 software (SPSS Inc., Chicago, IL, USA). A descriptive analysis was used for the characterisation of the patients. Qualitative variables were described as frequency and percentage. Quantitative variables were expressed as median. Comparisons between groups were conducted using Pearson's chi-square test (Fisher's exact test when needed) and the Mann–Whitney U test. A two-sided p<0.05 was considered statistically significant.
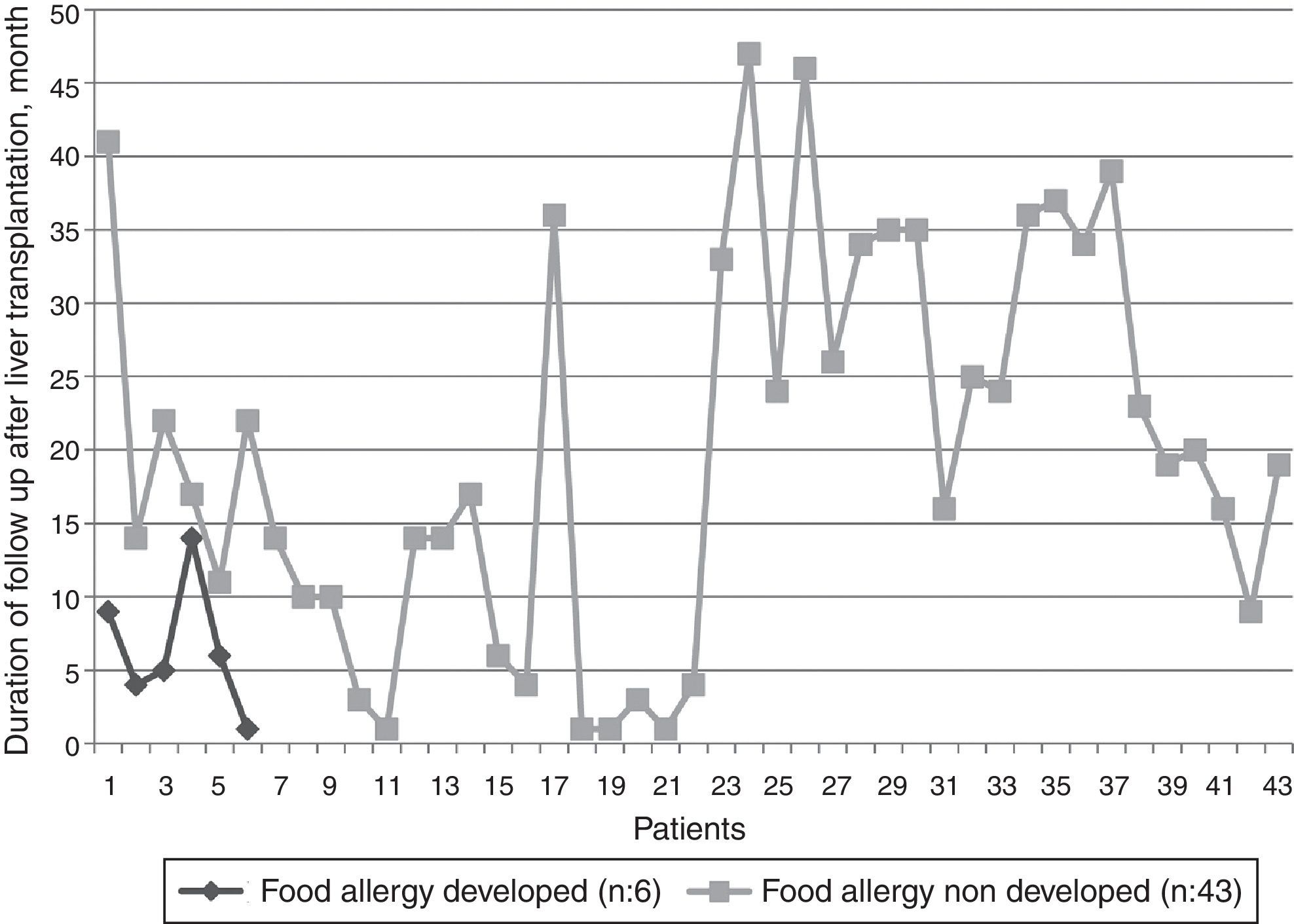
ResultsDemographicsForty-nine children were enrolled in the study; 26 (53.1%) were female and 23 (46.9%) were male. The median age and the age at transplantation were seven years (range: 1–17 years), and five years (range: 0.3–16.5 years), respectively. The most common reason for liver transplantation was acute fulminant hepatitis. Thirty-six patients (73.5%) received organs from living donors. The median follow-up period after transplantation was 16 months (range: 1–47 months). The duration of follow up of all the patients is shown in Fig. 1. Tacrolimus was the most common long-term immunosuppressive agent used after liver transplantation. Asthma was the most common comorbid atopic disease (Table 1). Peripheral eosinophil counts were measured in all patients, and serum total IgE levels were examined in 43 patients (87.8%). Twelve patients (24.5%) had serum total IgE levels >100IU/mL, and peripheral eosinophilia was present in 14 patients (28.6%).
Demographics of children who underwent liver transplantation (n: 49).
| Variable | n (%) |
|---|---|
| Age, median (min–max) | 7 (1–17) |
| Male | 23 (46.9) |
| Median duration of liver disease, months (min–max) | 4 (1–120) |
| Median age at the time of transplantation, years (min–max) | 5 (0.3–16.5) |
| Median duration of follow up, months (min–max) | 16 (1–47) |
| Type of transplantation | |
| Cadaveric organ | 13 (26.5) |
| Living related | 33 (67.4) |
| Living non-related | 3 (6.1) |
| Indication of liver transplantation | |
| Acute fulminant (viral, drug, toxic) | 19 (38.8) |
| Cholestatic liver disease | 10 (20.4) |
| Chronic hepatitis B | 1 (2) |
| Metabolic* | 8 (16.3) |
| Idiopathic | 8 (16.3) |
| Other† | 3 (6.2) |
| Chronic immunosuppressant regiment | |
| Tacrolimus | 36 (73.5) |
| Cyclosporine | 5 (10.2) |
| Tacrolimus & Everolimus | 4 (8.2) |
| Tacrolimus & Mycophenolate mofetil | 4 (8.2) |
| Co-existing atopic disease | |
| Asthma | 6 (12.2) |
| Allergic rhinitis | 2 (4.1) |
| Atopic eczema | 3 (6.1) |
| Drug allergy | 1 (2) |
| Acquired IgE-mediated food allergy after liver transplantation | 6 (12.2) |
Six patients (12.2%) developed IgE-mediated food allergies after transplantation: allergy to eggs in two patients, peanuts in one patient, bananas in one patient, cow's milk in one patient, and potatoes in one patient. Four patients developed urticaria and/or angio-oedema and two had anaphylaxis after food intake (Table 2). After avoidance of the culprit foods, there was no reported reaction.
Some data of the cases who developed IgE-mediated food allergy after liver transplantation.
| Variable | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
|---|---|---|---|---|---|---|
| Sex | F | F | M | F | F | F |
| Age of transplantation | 8 months | 10.5 years old | 7 years old | 10 months | 9 months | 17 years old |
| Indication of LTx | Giant cell hepatitis | Hepatitis B | Wilson's disease | Cholestatic | Cholestatic | Congenital hepatic fibrosis |
| Type of liver transplantation | Living related | Cadaveric | Cadaveric | Living related | Living related | Living non-related |
| Duration of reaction after LTx | 14 months | 4 months | 5 months | 8 months | 1 month | 6 months |
| Causing food | Hen's egg | Banana | Peanut | Hen's egg | Cow's milk | Potato |
| Type of reactions | Anaphylaxis | Urticaria, angio-oedema | Urticaria, pruritus | Angio-oedema | Anaphylaxis | Urticaria |
| Co-existing atopic disease | No | No | No | No | Atopic eczema | No |
| Atopic disease in donor | No | NA* | NA | No | No | No |
| EBV serology, pre transplant | Negative | NA | Negative | Negative | NA | Negative |
| EBV serology, after transplant | Negative | NA | Negative | Negative | NA | Negative |
| CMV serology, pre transplant | Negative | Negative | Negative | Negative | Negative | Negative |
| CMV serology, after transplant | Negative | Negative | Negative | Negative | Negative | Negative |
| Total IgE, at the time of reaction, IU/l | 539 | 7 | 18.2 | 463 | 480 | 306 |
| Peripheral eosinophil count, mm3 (%) | 700 (6.7) | 200 (3.9) | 400 (4.6) | 390 (4.9) | 450 (5.2) | 100 (1.1) |
| Immunosuppressant regiment | Tacrolimus | Tacrolimus | Tacrolimus | Tacrolimus | Tacrolimus | Cyclosporine |
| Serum level of immunosuppressant agent at the time of reaction, ng/ml | 9.9 | 7.1 | 9.8 | 8.9 | 6.1 | 127 |
* NA: not available.
Analysis of the risk factors showed similarities in sex (p=0.198), age at transplantation (p=0.602), comorbid atopic disease (p=0.588), immunosuppressant therapy with tacrolimus (p=1.0), and blood tacrolimus level (p=0.502) between the IgE-mediated food allergy group and the no allergy group. Serum total IgE levels ≥100IU/mL (p=0.02) and peripheral eosinophilia (p=0.026) were more common in the patients who developed IgE-mediated food allergies. In five of the six patients who developed IgE-mediated food allergies, the reaction occurred within the first year after transplantation; the risk of developing a reaction was 2.7 times higher within the first year after transplantation than in subsequent years (95% CI 1.546–4.914, p=0.026) (Table 3). No EBV or CMV infections were detected in the patients who developed IgE-mediated food allergies after liver transplantation.
Comparison of children who developed food allergy or not after liver transplantation.
| Variable | Food allergy developed (n: 6, %) | Food allergy not developed (n: 43, %) | p-Value | Odds ratio (95% CI) |
|---|---|---|---|---|
| Female | 5 (83.3) | 21 (48.3) | 0.198 | |
| Median age at the time of transplantation, years, (min–max) | 7.1 (0.3–10.8) | 5.9 (0.8–16.1) | 0.602 | |
| Time interval after transplantation<1 year | 5 (83.3) | 13 (30.2) | 0.020 | 2.7 (1.546–4.914) |
| Immunosuppressant agent, only with tacrolimus | 5 (83.3) | 31 (72.1) | 1.0 | |
| Co-existing atopic disease (excluding of food allergy) | 2 (33.3) | 8 (18.6) | 0.588 | |
| Total IgE≥100IU/ml | 4 (66.7) | 6/37 (16.2) | 0.020 | 4.1 (1.629–10. 373) |
| Eosinophilia, pre transplant (≥4%) | 1 (16.7) | 6 (14) | 1.0 | |
| Eosinophilia, post transplant (≥4%) | 4 (66.7) | 8 (18.6) | 0.026 | 3.5 (1.542–8.327) |
| Serum tacrolimus level, median (min–max), ng/ml | 8.9 (6.1–9.9) | 8.1 (5.8–13.2) | 0.502 |
Our study showed that IgE-mediated food allergy is common in paediatric patients who have undergone liver transplantation, and that the risk of developing reactions is greater within the first year after transplantation than in subsequent years. It was also determined that the use of tacrolimus as an immunosuppressant agent and tacrolimus blood levels were not associated with IgE-mediated food allergies, but peripheral eosinophil and serum total IgE levels were significantly higher in patients who developed IgE-mediated food allergies. Previous studies have reported that the incidence of IgE- and/or non-IgE-mediated food allergy after liver transplantation ranges from 8.5% to 37.6%.1,5,9 It was reported in these studies that patients mostly developed allergic reactions to eggs and milk. In our study, 12.2% of the patients developed IgE-mediated food allergies after transplantation, and the food that caused allergic reactions most often was eggs.
Studies have shown that food allergies occur mostly within the first year after transplantation.1,3,13 In our study, the reactions occurred within the first year in five of the six patients who developed IgE-mediated food allergies after liver transplantation. Our study also showed that the risk of developing a reaction is 2.7 times higher within the first year than in subsequent years.
Serum total IgE levels and peripheral eosinophil counts have been shown to be elevated in patients who developed food allergies after liver transplantation.9,13 In a prospective study conducted by Özbek et al.13 three of six patients who developed food allergies had serum total IgE levels >100IU/ml. In the study by Wisniewski et al.9 while the peripheral eosinophil count exceeded 1000eos/dL at least once in 70% of patients who developed food allergies after liver transplantation, this value exceeded 1000eos/dL in 30% of patients without food allergies. In our study, six patients developed food allergies after liver transplantation; four of those patients had eosinophil counts >4% and four had total IgE levels >100IU/ml. Furthermore, the presence of eosinophilia and serum total IgE levels >100IU/mL in patients who underwent liver transplantation increased the risk of food allergy development by 3.5 and 4.1 times, respectively, in our study. Although high IgE levels and eosinophilia are the risk factors for development of IgE-mediated food allergy after liver transplantation, food allergies can also develop after liver transplantation in patients who have normal IgE levels and eosinophil counts.
The severity of IgE-mediated food allergies after liver transplantation can manifest over a wide spectrum.2,4,5 In the study by Noble et al.2 four of 12 patients who developed food allergy reactions after liver transplantation had anaphylaxis. In our study, two of six patients developed anaphylaxis.
Özbek et al.13 reported that the use of tacrolimus as an immunosuppressant agent and EBV viraemia were associated with food allergies that developed after liver transplantation. On the other hand, Wisniewski et al.9 reported that the use of tacrolimus was not the only cause of food allergy after liver transplantation and that food allergy was not associated with EBV or CMV viraemia. In our study, no association between the use of tacrolimus and food allergy was found, and EBV infection was not detected in the patients who developed food allergies.
Our study has several limitations. First, because it is partly a retrospective study, some laboratory data are missing. Second, it has a limited number of patients. Third, because the serum total IgE levels prior to transplantation were not studied, post-transplant serum total IgE levels might have been overestimated. For these reasons, our conclusions regarding the positive findings (e.g., time of presentation, IgE level, and eosinophil count) of the study results are limited.
In conclusion, IgE-mediated food allergy after liver transplantation is not rare. The risk of developing an IgE-mediated food allergy is approximately three times higher within the first year after transplantation than in subsequent years. Therefore, patients who undergo liver transplantation should be closely monitored for food allergies, especially in the first year after transplantation.
Conflict of interestNo competing financial interests exist and there is no conflicts of interest statement for each author.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.