Anaphylaxis is an acute multisystemic and potentially fatal reaction, resulting from the rapid release of inflammatory mediators. Its exact prevalence is unknown. In children, foods are the most significant triggers for IgE-mediated anaphylaxis.
ObjectivesTo characterise the cases of anaphylaxis evaluated in an Allergy Division of a Central Paediatric Hospital.
Material and methodsA review of all cases of anaphylaxis evaluated from 2001 to 2009. Anaphylaxis was defined according to Sampson's 2006 criteria.
ResultsSeventy-three children had anaphylactic reactions (47 male), of which 64% had history of atopy. Age at time of reaction ranged between 17 days and 15 years old (median: four years). Food was the most frequently identified cause (n=57), followed by drugs (n=8), hymenoptera venom (n=2), and cold (n=1). In five cases there was no identifiable cause. Among foods, cow's milk was the culprit agent in 27 children. The most severe reaction was a cardiorespiratory arrest. The most frequent symptoms were respiratory and cutaneous in 51 cases. Hypotension was present in nine cases. There were no fatalities. Most acute reactions were treated with corticosteroids and/or antihistamines. Adrenaline was used in only about one quarter of children.
ConclusionsThe most important causes of anaphylaxis in our study were foods, and the most common symptoms were respiratory and cutaneous. The prevalence of anaphylaxis was higher in males and, in two thirds of patients there was a history of atopy. Despite being the primary and most important treatment for anaphylaxis, adrenaline is still used in only a minority of these cases.
Anaphylaxis is an acute multisystemic and potentially fatal reaction, resulting from the rapid release of inflammatory mediators by mast cells and basophils, and occurs when a susceptible person is exposed to a certain agent. The severity of the reaction can vary from mild to life threatening and can be rapidly progressive.1,2
The earliest description on record of a fatal allergic reaction is related to Menes, a first dynasty pharaoh, who died in 2621BC, presumably from an anaphylactic shock caused by a bee sting.3 Its name comes from the Greek: a (against) and phylaxis (immunity, protection), and was proposed in 1902 by Portier and Richet.4
According to the latest nomenclature proposed by the World Allergy Organization, it can be classified as: allergic (immunological reaction involving IgE, IgG or immune complexes) and non-allergic (where the mechanisms involved are not immune) (Table 1).5 Although it may appear that IgE-mediated anaphylaxis occurs upon a first exposure to a food, drug, or insect sting, there must have been a prior, and probably unwitting, sensitisation from a previous exposure.1 The patient, however, may not remember an uneventful sting or be aware of “hidden” allergens in foods.
Types anaphylaxis.
| Examples | |
| Allergic | |
| Foods | Milk, egg, peanut, fish, shrimp, cereals |
| Drugs | penicillin, cephalosporins, anesthetics |
| Hymenoptera venom | Bee, wasp, polistes |
| Vaccines | Specific immunotherapy, tetanus toxoid, vaccines containing egg |
| Latex | Gloves, balloons, condoms |
| Non-allergic | |
| Drugs | NSAIDs (aspirin, nimesulide, ibuprofen), muscle relaxants, gammaglobulin |
| Radiological contrast media | |
| Preservatives | Sulphites |
| Physical | Exercice, cold |
| Idiopathic | Unknown cause |
The definition of anaphylaxis has only become consensual since 2006, following the completion of the Second Symposium on the Definition and Management of Anaphylaxis,6 allowing the standardisation of diagnostic criteria and comparison of epidemiological data between different countries. The prior absence of a consensual definition contributes to explaining the significant variation in the reported lifetime frequency of anaphylaxis in different countries, ranging from 0.02% to 0.5%.7 Its exact prevalence is unknown, being estimated that 1 in 1333 people in the United Kingdom have suffered an episode during their lifetime.8 In children, foods (mainly cow's milk, egg, wheat, peanut, and fish) are the most often involved triggers for IgE-mediated anaphylaxis. Other allergens include drugs (mainly beta-lactam antibiotics), hymenoptera venom, and administration of specific immunotherapy. Non-IgE triggers include NSAIDs, radiological contrast media, exercise, and cold.9 Several reports suggest that almost 20% of all episodes of anaphylaxis are idiopathic.10
In 5% to 20% of cases of anaphylaxis, a biphasic reaction can occur, the severity of which may be equal to or higher than the initial reaction, and is generally more refractory to standard treatment. This second reaction can occur between 1 and 72h (generally 8–12h) after the first one.11,12
ObjectivesTo characterise the cases of anaphylaxis evaluated in an Allergy Division of a Central Paediatric Hospital and to compare the data with other published studies on this subject.
Material and methodsA retrospective study of all cases of anaphylaxis in children under 18 years of age evaluated in the Allergy Division of Centro Hospitalar do Porto, EPE – Hospital Maria Pia, Portugal, in the period from 2001 to 2009. Anaphylaxis was defined according to Sampson et al.6 (Table 2). For grading the severity of anaphylactic reactions, three categories were defined: Mild, when there was no respiratory or cardiovascular involvement; Moderate, when respiratory symptoms were present, but without cardiovascular involvement; and Severe, when there was shock/hypotension or cardiovascular collapse.
Clinical criteria for the diagnosis of anaphylaxis.
| Clinical criteria for the diagnosis of anaphylaxis |
| Anaphylaxis is highly likely when any one of the following three criteria are fulfilled |
| 1. Acute onset of an illness (minutes to several hours) with involvement of the skin, mucosal tissue, or both and at least one of the following: |
| a. Respiratory compromise (e.g. dyspnoea, bronchospasm, stridor, hypoxia) |
| b. Cardiovascular compromise or associated symptoms of end-organ dysfunction (e.g. hypotension, collapse, syncope, incontinence) |
| 2. Two or more of the following that occur after exposure to a likely allergen for that patient (minutes to several hours): |
| a. Involvement of the skin or mucosal tissue (e.g. generalized hives, itch, flushing, swelling) |
| b. Respiratory compromise (e.g. dyspnoea, bronchospasm, stridor, hypoxia) |
| c. Cardiovascular compromise or associated symptoms of end-organ dysfunction (e.g. hypotension, collapse, syncope, incontinence) |
| d. Persistent gastrointestinal symptoms (e.g. crampy abdominal pain, vomiting) |
| 3. Hypotension after exposure to known allergen for that patient (minutes to several hours) |
| Infants and children: low systolic BP (age-specific) or greater than 30% decrease in systolic BP |
| Adults: systolic BP of less than 90mm Hg or greater than 30% decrease from that person's baseline |
The diagnostic work up of all children with anaphylaxis evaluated included (1) detailed clinical history, with special emphasis on the events surrounding the episode, the clinical manifestations, the severity of attacks, the response to treatment, and evolution; (2) physical examination; (3) skin tests with the suspect allergen and intradermal tests for drug and hymenoptera venom allergy; (4) specific IgE determination by fluorescence enzyme immunoassay (Unicap®, Phadia, Sweden); (5) other specific tests, such as ice cube test for cold-induced anaphylaxis, and complement and basal tryptase levels determination when necessary to exclude other causes.
As this is a descriptive study, qualitative variables such as sex, symptoms, culprit agent, as well as results of tests are described in frequency and percent. Quantitative variables, such as age, are expressed with medians.
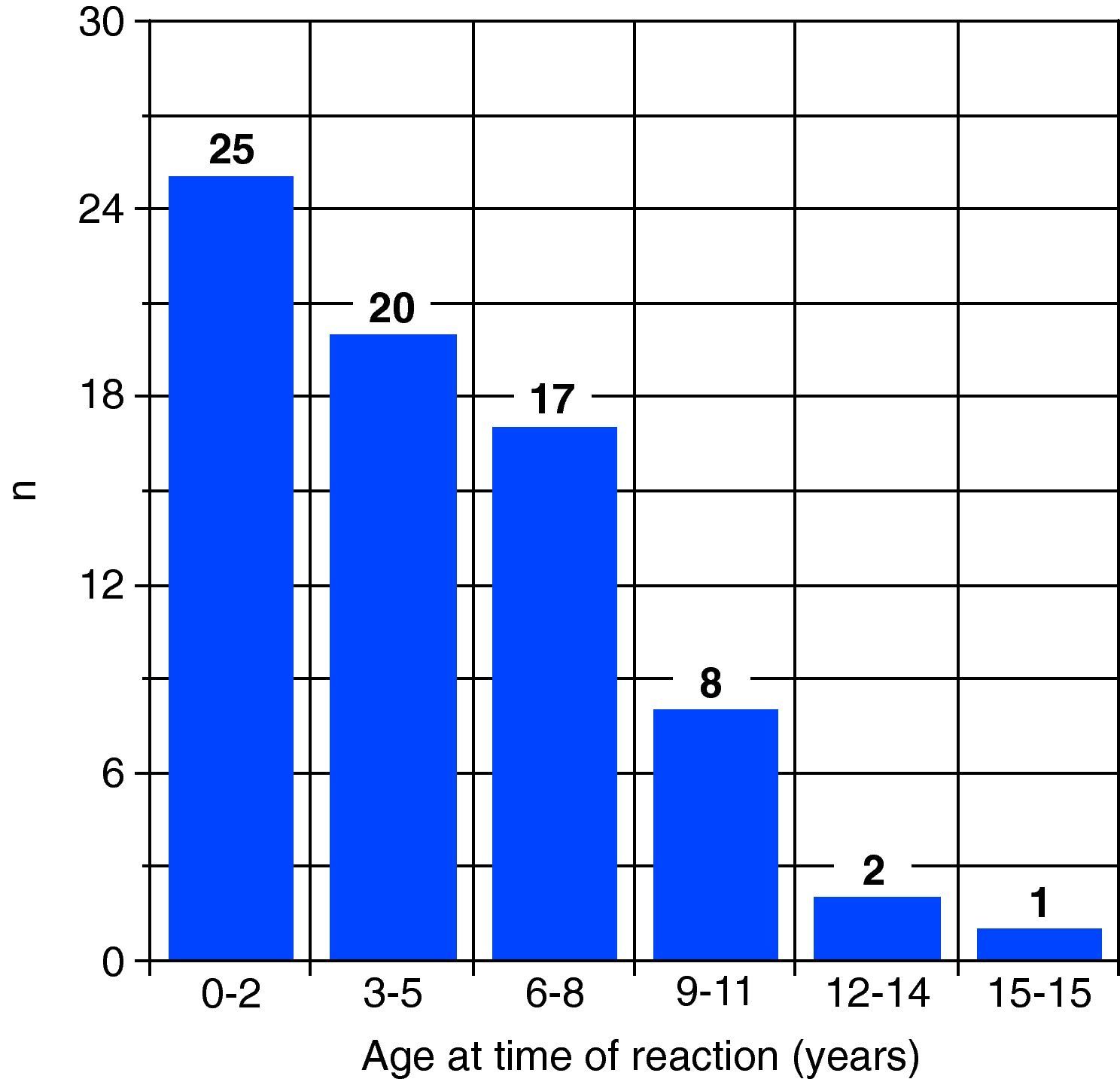
ResultsDuring the study period, 73 children were consulted for anaphylactic reactions (47 ♂), of whom 64% had a personal history of atopy. The age at the time of the reaction ranged between 17 days and 15 years old, with a median of four years (Fig. 1). At least 21 of these children had one or more previous episodes of allergic reaction to the agent that caused the anaphylaxis.
Foods were the most frequently identified cause (n=57), followed by drugs (n=8), hymenoptera venom (n=2) and cold (n=1). In five cases it was not possible to identify a causal agent after extensive study, and the anaphylaxis was therefore classified as idiopathic. Food anaphylaxis presented at an earlier age than both drug and hymenoptera venom induced anaphylaxis (median ages 3 years, 5.5 years and 8 years, respectively). Children with idiopathic anaphylaxis had a median age of five years. Among the foods, cow's milk was the culprit agent in 27 children. Fish, shrimp and mollusc allergy were responsible for 13 cases; cereals and nuts for eight; egg for five; and fruits for four. All drug-induced anaphylactic reactions were attributed to beta-lactams and gentamicin (Table 3). The skin tests and/or specific IgE for the culprit allergen were positive in all cases of anaphylaxis due to foods and to hymenoptera venom. The ice test cube was positive in the child with history of cold-induced anaphylaxis.
The most severe reaction was a cardiorespiratory arrest in a milk-allergic child. The most common symptoms were respiratory and cutaneous in 51 cases (of which 17 also had gastrointestinal involvement). Hypotension occurred in nine cases, with respiratory and/or gastrointestinal and/or cutaneous manifestations. Ten children had gastrointestinal and cutaneous symptoms, and two had respiratory and gastrointestinal symptoms. There were no fatalities in our series. According to the grading system described above, the majority of the reactions were classified as moderate (53 cases, 72%), with the remaining ones equally divided as mild and severe (10 cases, 14% for each). Median age of children with severe reactions was lower than those with moderate and mild reactions (1.25 years for severe reactions vs. 4 years for moderate and for mild reactions).
Most reactions were treated in the emergency department with corticosteroids, antihistamines, or both. Aerosolised salbutamol and ipratropium bromide were also used in reactions with respiratory symptoms. Adrenaline was used in the treatment of the acute episode in only one quarter of the children.
DiscussionAnaphylaxis is diagnosed with high likelihood based on clinical criteria, and there is no gold standard test. In recent years, objective criteria have been proposed for its diagnosis, allowing the comparison of data from different populations and a greater knowledge of the triggering factors, risk factors and other data essential for proper monitoring of these patients.
According to recent reports, the incidence rate of anaphylaxis is increasing, particularly during the first two decades of life.9,13,14 The largest published study of anaphylaxis in paediatric patients included 117 children, and was done at the Royal Children's Hospital in Melbourne, Australia.15 In that article, the median age at diagnosis was 2.4 years, and foods were the most frequent precipitating factor, accounting for 85% of cases. Among foods, peanuts and cashew were the most frequently involved.
Another study from Israel, which reviewed the clinical files of all children who were admitted to the Schneider Children's Medical Center of Israel with a diagnosis of anaphylaxis over a 12-year period, was recently published.16 During the study period, 92 children with anaphylaxis (50 males), aged 14 days to 18 years (mean: 7.4 years) were hospitalised. The main causes were foods (43%), mainly milk and nuts, drugs (22%), and hymenoptera venom (11%). In five children, the cause could not be identified. There was history of atopy in more than half of children.
In a questionnaire-based survey done to Paediatricians in Germany regarding episodes of anaphylaxis in infants and children below 12 years of age, 103 cases were reported. Median age was five years, and 58% were boys. Foods were the most common causal allergen (57%), followed by insect stings (13%), and specific immunotherapy (12%).17 However, since this study was done before the current definition of anaphylaxis was proposed, several cases not currently considered as such were included, which difficult the analysis and possibly explains the relatively high number of cases attributed to insect stings and specific immunotherapy. Another limitation lies in the fact that the suspected aetiological agent of anaphylaxis was reported by the physicians in the questionnaire, and was not proven by allergy tests in the majority of cases.
Ours is the largest European study published to date using the current definition of anaphylaxis, with 73 children studied. Similarly to most studies published in the literature, the most frequently involved agents in anaphylaxis in children are foods, mainly cow's milk.16,18,19 Also in agreement with previous studies,8,20 the prevalence of anaphylaxis until adolescence was higher in males. Atopy was also present in two thirds of the children in our study. According to the literature, atopic individuals have a higher predisposition to anaphylactic episodes, and dominate series of all causes of anaphylaxis.16,18,21,22 A possible explanation is that the extracellular cytokine milieu associated with atopic diseases may account for the increased risk of atopic individuals to an anaphylactic reaction.23 It should also be noted that several studies have reported an association of anaphylaxis with several gene groups, including genes that affect the anatomic barrier, and genes associated with the innate and adaptive immune systems.24 Idiopathic anaphylaxis is a diagnosis of exclusion and therefore extensive labwork and testing are required to rule out possible culprit allergens and the numerous diseases that may appear as idiopathic anaphylaxis (such as a carcinoid syndrome, cutaneous or visceral mastocytosis, deficiency of C1 esterase inhibitor, among others).25 In our study, five cases (7%) were classified as idiopathic after full diagnostic work-up.
The existing grading systems for severity of anaphylaxis are based on outdated definitions of anaphylaxis, which included some systemic hypersensitivity reactions currently not considered as anaphylaxis. For our grading on the severity of anaphylactic reactions, we defined three categories (mild, moderate and severe), detailed in the “Material and methods” section. The most common symptoms were respiratory and cutaneous and, according to the grading system described, the majority of the reactions were classified as moderate. It is probable that a selection bias is present in this population, since mild cases of anaphylaxis are more frequently underdiagnosed, and therefore not referred to an allergy division for study and follow-up. Also, hypotension sometimes goes undocumented, especially in infants and young children, which may explain the relatively low number of cases classified as severe.26
The primary and most important treatment for anaphylaxis is adrenaline, at a dose of 0.01mg/kg of a 1mg/mL (1:1000) dilution to a maximum dose of 0.3mg in a child, which can be repeated if necessary.27–32 Despite being recommended in all anaphylaxis management guidelines as the mainstay of treatment for anaphylaxis, adrenaline is still used in only a minority of these cases, meaning that three-quarters of these children did not receive adequate treatment. Even after the complete resolution of symptoms, a period of observation at the Hospital for a minimum of 8 or 10h is recommended, in order to monitor the recurrence of symptoms and a possible biphasic reaction.12,28,33
A recent review has shown that food allergy, particularly in cases of severe reactions such as anaphylaxis, has a very significant impact on the quality of life of children and their parents. The burden of responsibility and the constant vigilance needed to avoid allergens, as well as the uncertainty associated with the possibility of accidental exposures, are major contributing factors.34
In a study by Ferreira and Alves,35 which used a multiple-choice questionnaire to evaluate the practical knowledge of diagnostic and therapeutic aspects of anaphylaxis among general practitioners in Portugal, the authors found a percentage of correct answers ranging from 36% to 46% regarding the diagnostic questions, and from 18% to 22% regarding the anaphylaxis treatment. This lack of knowledge and misconceptions about the treatment of an anaphylactic reaction among the medical community constitute a major concern since this can be a life-threatening condition. There is an urgent need to increase knowledge and awareness regarding the treatment of anaphylaxis and the importance of referring the patient to an allergist for appropriate follow-up. The complete study of all cases of anaphylaxis is required in order to allow to identify the cause, and to help prevent future reactions. In cases of food allergy, the child and the parents must be clearly informed about dietary restrictions, including foods with known cross-reactivity, the possibility of its presence as a “hidden allergen”, and instructed to always read the food labels to avoid possible untoward reactions.36,37 Parents of children considered to be “at risk” of anaphylaxis are advised to inform schools of their children's allergies and what to do in case of a reaction. An adrenaline (epinephrine) auto-injector should be prescribed to all patients with a history of anaphylaxis, according to the recommendations of the European Academy of Allergy and Clinical Immunology29 and the American Academy of Allergy Asthma and Immunology,36 with detailed instructions on how to proceed in the event of future reactions. Specific immunotherapy with hymenoptera venoms is effective in preventing future episodes of anaphylaxis caused by these agents.24,38,39 Oral desensitisation is effective for many foods, and can be proposed in certain cases of food induced reactions.9,24,40–42 For anaphylaxis triggered by a drug, if that drug is indispensable for treatment (such as chemotherapic agents) and there is no alternative drug, a tolerance induction protocol can generally be used to obtain temporary tolerance.24,43,44
In conclusion, the most important causes of anaphylaxis in our study are foods, particularly cow's milk, and the most common symptoms were respiratory and cutaneous. The prevalence of anaphylaxis was higher in males and, in two-thirds of the patients there was a history of atopy. Adrenaline was used in only one quarter of the children, meaning that the majority of the cases did not meet the recommended standards of care with regard to administration of intramuscular adrenaline. There is an urgent need to increase knowledge and awareness regarding the treatment of anaphylaxis and its follow-up among the general medical community.
Conflict of interestThe authors have no conflict of interest to declare.