Rice, the seed of monocot plant Oryza sativa, is nowadays a basic element in almost every culinary tradition throughout the world, mainly in Asia, Africa and South America, where it represents as much as 20% of the total calories ingested per day. The production of this cereal grain has become comparable to that of wheat and corn, due to several factors such as price, edibility and nutritional value. Rice belongs to the Poaceae family; therefore cross-reactivity is suitable between this grain and other constituents of the former family.
Despite its widespread consumption, case reports in the literature regarding rice allergy, in any of its forms, remain surprisingly scarce. Hitherto, two different routes have been argued which could lead to immediate rice hypersensitivity reactions: boiled rice ingestion and inhalation of both boiled rice vapours and/or raw rice powder.1
Moreover, three groups of allergens have been involved in rice allergy, a 33kDa Glyoxalase I showing a unique structure consisting of two tandemly repeated homologous domains with some well-conserved sequences, similar to Glyoxalase I plants2; two allergens which belong to the amylase inhibitor family of 14 and 16kDa, respectively; and Lipid Transfer Proteins (LTP), reported in an elegant work published in 2006 by Asero et al. in which they could demonstrate cross-reactivity between rice-LTP and apple/peach LTP in three cases of rice-induced anaphylaxis subsequent to ingestion of the former.
It remains elusive as to whether rice-LTP allergic potential dilutes subsequent to boiling process or by contrast this protein could form a macromolecular matrix during cooking procedures which could hamper its binding to specific IgEs, so digestion would facilitate hidden epitopes to be recognised by their specific antibodies.3 Likewise, Enrique et al. described three cases of patients with respiratory allergy to raw rice by inhalation who tolerated boiled rice ingestion.4
Kim et al. reported work-related rhinitis and conjunctivitis symptoms caused by occupational exposure to rice powder in the grain industry. They performed an IgE ELISA inhibition test which demonstrated cross-creativity between rice and several grass pollen extracts.5 Besides, Ory s 1, has elicited cross-reactivity with rye and Bermuda grass pollens in patients suffering from pollen allergy and shares significant sequence identity with the major pollen allergen of rye grass (Lol p 1; 65.5% identity) and Bermuda grass (Cyn d 1; 62.9% identity).6
A 36-year-old woman who had been working for two years in a pizzeria kneading pizza dough reported immediate rhinoconjunctivitis while manipulating pizza dough during the past six months. She attributed typical rhinoconjunctival symptoms due to a special flour (“oak semolina”) poured in the location where pizza dough was blended. Hygienic conditions at work place were appropriate and she did not have history of allergic rhinoconjunctivitis. Furthermore, she did not suffer from these symptoms on non-working days and holidays. In a successive visit, the patient indicated subsequent continuous sneezing and rhinorrhoea from April to June outside her work-place which limited her daily activities and sleep. The pizzeria where she works commonly uses rice powder, which is a flour variety known as oak semolina in Spain, frequently placed to enhance blending of the pizza dough and to ease its mixture. Firstly we performed skin prick testing against common aeroallergens [(D. pteronyssinus and Dermatophagoides pteronyssinus, Lepidoglyphus destructor, animal dander (dog and cat), storage mites (Tyrophagus putrescentiae, Euroglyphus maynei, Glycyphagus domesticus, Acarus siro) Alternaria alternata, Aspergillus fumigatus, Quercus sp., Populus sp., Willow sp., Elm sp., Birch tree, Ash tree, Holm oak, Acacia, Olea europaea, Platanus acerifolia, Plantago lanceolata, grass mix (Dactylis, Trisetum, Lollium, Phleum and Poa), Parietaria judaica, Artemisia vulgaris, Taraxacum officinalis, Cupressus arizonica)], flour battery (wheat, rye, corn, soy, oat, rice and barley), common grains (wheat, corn, oat, barley, rye) and prick-by-prick against oak semolina (rice powder flour) as well as wheat flour. Specific IgE (CAP Phadia, Sweden) was determined against D. pteronyssinus, D. farinae, L. destructor, rPhl p 1-5b, rPhl p 7-12, rPrup3, and rice flour; Besides, sIgE against Tri a 14 and wheat flour-α-amylases (Cm 3 and Cm 16) was determined by ADVIA-Centaur (Siemens). In order to discard rye flour cross-sensitisation to rice flour we performed a 2D-immunoblot essay. Microbiology department randomly selected seven flour samples and explored them by means of a high power field microscope, in order to rule out possible contaminants (i.e. storage mites and moulds). A fibre optic rhinoscopy was carried out in order to discard nasal polyps or structural abnormalities, both before and after nasal provocation test (NPT). An Anterior rhinomanometry was performed before and after NPT.
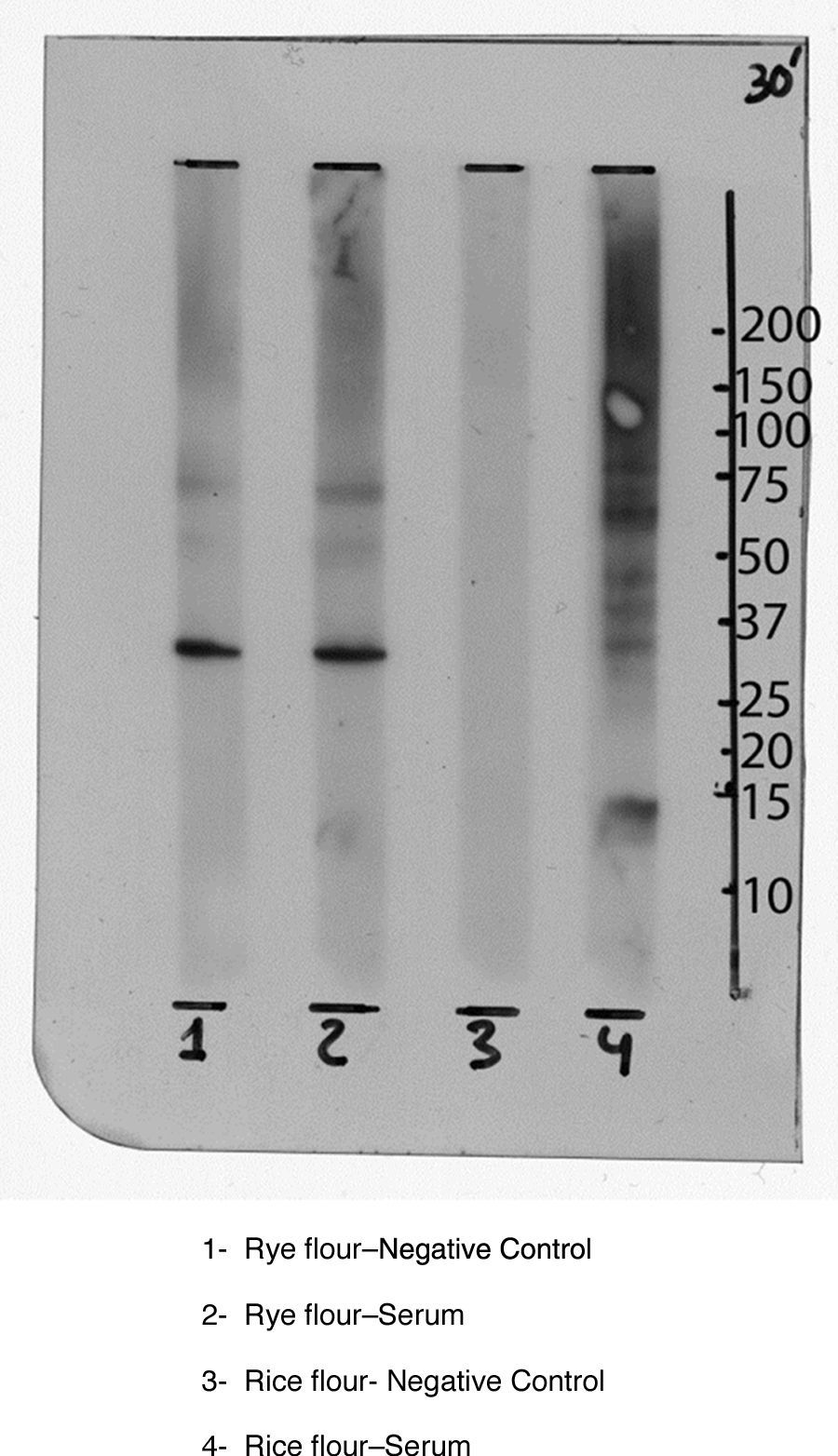
Skin prick test resulted positive against mites (D. pteronyssinus, D. farinae, L. destructor), storage mites (T. putrescentiae, E. maynei, G. domesticus, A. siro), pollens (Populus sp., Willow sp., Elm sp., Birch tree, Ash tree, Holm oak, Acacia, O. europaea, P. acerifolia, Dactylis, Trisetum, Lollium, Phleum and Poa) also rye and rice flour and negative against moulds, animal dander, alpha-amylase, enolase, papain and grains. Skin prick-by-prick resulted positive against rice powder flour and negative against wheat flour. Specific IgEs (sIgE) resulted as follows: D. pteronyssinus: 6.75kU/L; D. farinae: 4.85kU/L; L. destructor: 54.60kU/L; rPhlp1-5b: 14.30kU/L; rPhl7-12: 0.03kU/L; rice flour: 0.88 kU/L; rPrup3: 0.89kU/L. sIgE against Tri a 14 and wheat flour-α-amylases (Cm 3 and Cm 16) resulted both negative (0.0kU/L). Immunoblot essay did not reveal potential cross-reactive allergens among rye and rice flour (Fig. 1). Immunoblot essay performed with rye flour and rice flour did not demonstrate cross-sensitivity among the previous flours.
She did not complain about experiencing symptoms after eating boiled rice or the ingestion of prepared food.
As the recently published EAACI position paper on occupational rhinitis states,7 we performed a nasal provocation test in order to elucidate the culprit agent as the SEAIC Rhinoconjunctivitis Committee recently stated.8,9 We placed the patient in a 4m3 room resembling her work-place where she manipulated trays which contained oak semolina. It is of note that the patient was completely asymptomatic and the challenge test was carried out outside the pollen season. The patient was asked to pour the content included in one tray into the other during 30min. After 5min of handling rice flour, our patient suffered from intense sneezing, rhinorrhoea and itchy eyes. Fifteen minutes later an anterior rhinomanometry was fulfilled which measured severe obstruction of both nostrils, differing from the one carried out before the specific nasal provocation test. Nasal smear taken right after the specific challenge with rice powder presented 30% of eosinophils. As control, a nasal provocation test with wheat flour resulted negative, following the same procedure previously described. The patient showed normal spirometry volumes and negative bronchodilator challenge. Therefore, the final diagnosis was occupational rhinitis caused by rice flour in a patient suffering from persistent moderate rhinitis.
We report an unusual case of occupational rhinitis due to rice flour in a pizzeria worker. Prick testing against rice flour, specific nasal challenge and subsequent assessment by means of endoscopy and anterior rhinomanometry as well as cessation of symptoms following strict avoidance of “oak semolina” reinforce the noteworthy diagnosis. Cross-reactivity between Poaceae and rice, together with LTP potential implication, could constitute the reasons of rice sensitisation in this patient, according to former research about this topic. Therefore it would be suitable to assess LTP sensitisation in grain sensitised patients. Rye sensitisation observed in our patient could be due to alpha-amylase inhibitors which are considered main rice allergens, shared among both grains. For that reason for performing immunoblotting essays which discarded a potential rye flour implication and due to the fact that sIgE against alpha-amylase inhibitors were negative, we can conclude that both alpha-amylase and rye allergens were not involved in our patient's symptoms. Outwardly Glyoxalase I, another rice allergen might not be implicated in this case as there is no wheat or barley sensitisation. It is of note that while wheat could be suspected as an important allergen as it is one of the ingredients of the pizza dough, rice flour is the only kind of raw flour which is poured and directly handled in this pizzeria, as the pizza dough is pre-cooked and instrumentally mashed, avoiding direct hand contact. Moreover, both skin prick testing against wheat flour and sIgE against Tri a 14, a major wheat allergen, resulted negative, therefore discarding wheat flour as the culprit allergen in this case.
As has recently been described,9 nasal provocation testing with standardised allergens can generally be started at an initial concentration of 1:1000 and then increased by a factor of 10. In the case of less well-known and occupational allergens, endpoint titration should be performed to identify the initial dose. Regarding occupational allergens, the irritant concentration limit for each substance must also be considered. Nonetheless, we performed a use provocation test with rice flour in a room resembling that in which the patient works to simulate real workplace conditions, handling trays containing the factory's own rice flour. It remains elusive whether rice-LTP allergic potential dilutes subsequent to boiling process or by contrast this protein could form a macromolecular matrix during cooking procedures which could hamper its binding to specific IgEs, so digestion would facilitate hidden antigenic determinants to be recognised by their specific antibodies.
Despite its widespread consumption, case reports in the literature regarding rice allergy, in any of its forms, remain sparse. Hitherto, two different routes have been argued which could lead to immediate rice hypersensitivity reactions: boiled rice ingestion and inhalation of both boiled rice vapours and/or raw rice powder. We believe this to be an important case because of the fact that rice flour was a hidden allergen in this patient and also due to the circumstance that occupational rhinitis could lead to suffering from occupational asthma resulting in socio-economic disruption. Further assessment and investigation regarding rice hypersensitivity are required in order to straighten out the former hypothesis.
ContributorsDAA, JBE, MSPB, MRR, EMV and MAM were involved in data analysis and writing manuscript. DAA was involved in patient follow-up and pharmacologic advisory. JAGR carried out anterior rhinomanometry and nasal endoscopy. LJN performed skilled technical assistance and fulfilled component resolved diagnosis on the ADVIA platform.
Conflict of interestThe authors have no conflicts of interest to declare.
Funding sourceThis work was partially supported by a grant from Comunidad de Madrid S2010/BMD-2502 MITIC.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Note: This case report was partially displayed as oral communication in Reunión de Clausura XX Sesiones Interhospitalarias Sociedad Madrid-Castilla La Mancha de Alergología e Inmunología Clínica, Sigüenza (Guadalajara, Spain). June 3rd 2011.