Food allergy in school children ranges between 5.7 and 6.4% in Turkey. Studies emphasize the importance of improving school personnel's self-efficacy in managing food allergy and anaphylaxis. However, a brief and valid measurement tool for school personnel is not available in Turkey. The aim of this study was to determine the validity and reliability of the Turkish version of the School Personnel's Self-efficacy in Managing Food Allergy and Anaphylaxis (SPSMFAA-T) scale with teachers.
Patients or materials and methodsThis methodological study was conducted by 282 primary school teachers. Data were collected with a demographic characteristics form and SPSMFAA-T. The psychometric properties of the SPSMFAA-T were evaluated by content, discriminant, construct validity and internal consistency.
ResultsCronbach's alpha for the scale was 0.91 and item-total correlations were between 0.50 and 0.82 (p<0.001). The discriminant validity suggested that the scale successfully discriminated the teachers who had training on food allergy and anaphylaxis from the teachers who did not. The model fit indices of scale were determined to be the root mean square error of approximation (RMSEA) at 0.08, goodness of fit index (GFI) at 0.96, comparative fit index (CFI) at 0.99.
ConclusionsThe results supported that the SPSMFAA-T was a valid and reliable measurement tool to assess Turkish teachers’ self-efficacy levels to manage food allergy and anaphylaxis in school setting. The scale can be used in education programs to improve school personnel's skills to manage food allergy and anaphylaxis.
Food allergy (FA) is defined as an immunologic reaction to nutrients, and can lead to increases in the prevalence of diseases and life-threatening anaphylaxis. Food allergies are more common in children than in adults.1 The health surveys report that FA in children ranges between 4% and 18% in US2 and Europe,3 and between 5.7% and 6.4% in Turkey.4,5 Of FA and anaphylaxis cases, 18% occur in the school environment. Moreover, many children who do not have a known history of allergy experience their first anaphylaxis reaction at school.6–8
One study found that school personnel did not know the symptoms of FA, that very few schools had written policies on the management of FA, the school personnel trained for FA, and label reading, and that adrenaline injection was very little preferred in severe reactions.9 Studies have shown that there is not any adrenalin in schools that school personnel do not consider themselves adequate for performing adrenalin injection, and that training on the issue is inadequate.10,11 In Turkey, studies yielded similar results that teachers were not competent enough to recognize the symptoms of FA and anaphylaxis, that their adrenaline awareness was low, that they were not skillful enough to apply first aid, and that they were not aware of the school action plan regarding anaphylaxis management.12,13
Sasaki et al.14 demonstrated that of the school personnel with the highest self-efficacy on the use of the adrenalin auto-injector were school nurses and that the self-efficacy of other school personnel regarding the use of the adrenalin auto-injector could be increased by training. This result suggests that in schools where health professionals are not available, the training of school personnel and the development of their awareness, self-efficacy and skills are becoming an issue of great importance. Assessment of self-efficacy of school personnel on FA and anaphylaxis management by a validated measuring instrument is considered to contribute to the planning of health education programs. The School Personnel's Self-Efficacy in Managing Food Allergy and Anaphylaxis (SPSMFAA) was developed by a multidisciplinary team of experts, based on Bandura's self-efficacy scale, previous studies and clinical experiences.15
The responsibility for the management of FA and anaphylaxis lies primarily with teachers because schools in Turkey generally do not have school nurses or health workers. Additionally, there was not such a valid measurement tool with which to assess the self-efficacy of teachers. The main aim of the present study is to assess the cultural appropriateness and psychometric properties of the Turkish version of School Personnel's Self-efficacy in Managing Food Allergy and Anaphylaxis scale (SPSMFAA-T) for Turkish society.
Material and methodsStudy design and subjectsThis methodological study was conducted with teachers working in eight state and four private primary schools in the city center of Izmir, Turkey, between April 2017 and June 2017.
In scale analysis studies, it is suggested that the sample size should be a minimum of five-fold or ideally ten-fold the number of the items in the scale.16 In the present study, it was planned to include at least 80 teachers, which corresponds to 10 fold the total number of the items of the eight-item scale. In order to assess the relationships between the variables, all the teachers in the aforementioned schools who volunteered to participate in the study were included in the study. A total of 410 teachers were working at these schools. Of them, 282 agreed to participate in the study. The response rate was 71.2%. The valid response rate in the 282 participants was 100%.
Approval was conducted from the ethics committee of the university where the researchers work (approval no: 3241-GOA-2017/09-05) and written consent from teachers was obtained.
MeasurementsThe data were collected with demographic characteristics form and SPSMFAA-T. The SPSMFAA developed by Polloni et al.15 assesses the perceived self-efficacy of school personnel's (teachers, caregivers, health personnel, etc.) ability to manage food allergy and anaphylaxis in the school environment. Responses given to the eight items on the scale are rated on a five-point Likert scale ranging from 1 (I cannot do at all) to 5 (I certainly can do). The higher the score is, the higher the self-efficacy level is. In this study, the SPSMFAA was translated to Turkish using the back translation technique. To establish the content validity of the SPSMFAA-T, opinions of eight experts (specializing in public health, school nursing, pediatrics) were obtained. The content validity index (CVI) of the SPSMFAA-T was 100%, which suggested that there was a consensus among experts.17 The final version of the SPSMFAA-T was pre-tested with 20 teachers who were not included in the sample and this was seen to be efficient.
The demographic characteristics form was developed by the researchers and included items questioning the participants’ demographics (age, gender, etc.).
After the teachers were informed about the purpose of the study in the school setting, the teachers who volunteered completed the instruments. The researchers informed the participants that their responses would be kept confidential.
Statistical analysesData were analyzed using the SPSS 15.0 version and LISREL 8.0. p values <0.05 were considered statistically significant. The characteristics of the teachers were evaluated with the descriptive statistics (number, percentage, mean, standard deviation). Reliability was assessed with Cronbach's α reliability coefficient and item-total correlation with Spearman's correlation analysis. The acceptable reliability criterion was at least 0.70 for Cronbach's α and between 0.30 and 0.70 for the item-total correlations.18,19 The validity of the scale was assessed with the content validity, construct validity and discriminant validity. While the content validity was assessed with the content validity index (CVI), the construct validity was assessed with the confirmatory factor analysis (CFA), and the discriminant validity was assessed with the t-test to determine the difference between the SPSMFAA-T scores of the teachers who had training on food allergy and anaphylaxis and those of the teachers who did not. The CVI was computed by summing the percentage agreement scores of all the items to which the experts gave a rating of “being quite” or “very relevant”. The acceptable criterion for the CVI was at least 0.80.17 The multiple regression analysis was conducted to determine the factors affecting self-efficacy scores of the teachers.
ResultsThe participants’ mean age was 42.93±8.78, and 83% were female. Their mean length of service was 19.07±9.42 years. Of them, 11% had post-graduate education; 60% were working in a public school; 20% previously worked with a student with food allergy; 17% working with a student with food allergy now; 3% previously worked with a student with anaphylaxis; 14% previously had training on food allergy and anaphylaxis; and 81% previously received training on first aid.
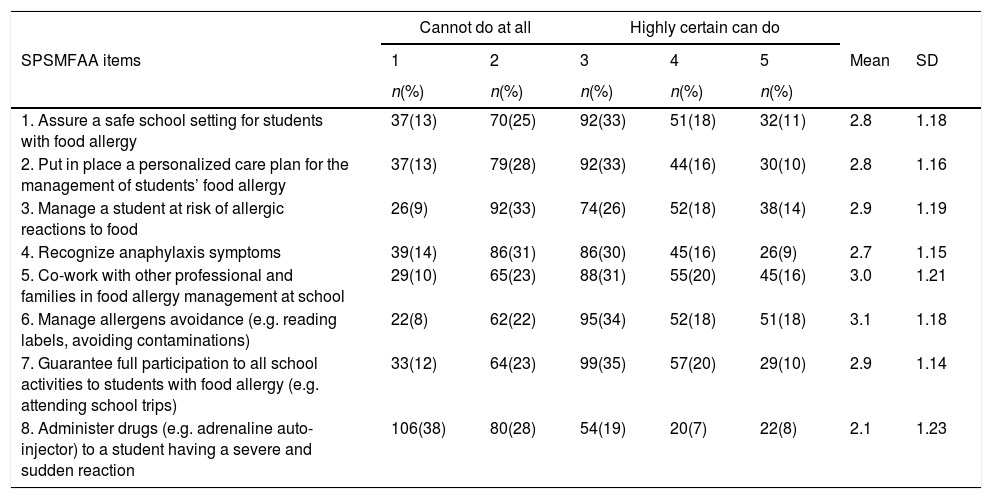
The distribution, mean, and standard deviation of the responses given to the items of the SPSMFAA-T by the teachers are given in Table 1.
Teachers’ self-efficacy in managing food allergy and anaphylaxis (n=282).
| Cannot do at all | Highly certain can do | ||||||
|---|---|---|---|---|---|---|---|
| SPSMFAA items | 1 | 2 | 3 | 4 | 5 | Mean | SD |
| n(%) | n(%) | n(%) | n(%) | n(%) | |||
| 1. Assure a safe school setting for students with food allergy | 37(13) | 70(25) | 92(33) | 51(18) | 32(11) | 2.8 | 1.18 |
| 2. Put in place a personalized care plan for the management of students’ food allergy | 37(13) | 79(28) | 92(33) | 44(16) | 30(10) | 2.8 | 1.16 |
| 3. Manage a student at risk of allergic reactions to food | 26(9) | 92(33) | 74(26) | 52(18) | 38(14) | 2.9 | 1.19 |
| 4. Recognize anaphylaxis symptoms | 39(14) | 86(31) | 86(30) | 45(16) | 26(9) | 2.7 | 1.15 |
| 5. Co-work with other professional and families in food allergy management at school | 29(10) | 65(23) | 88(31) | 55(20) | 45(16) | 3.0 | 1.21 |
| 6. Manage allergens avoidance (e.g. reading labels, avoiding contaminations) | 22(8) | 62(22) | 95(34) | 52(18) | 51(18) | 3.1 | 1.18 |
| 7. Guarantee full participation to all school activities to students with food allergy (e.g. attending school trips) | 33(12) | 64(23) | 99(35) | 57(20) | 29(10) | 2.9 | 1.14 |
| 8. Administer drugs (e.g. adrenaline auto-injector) to a student having a severe and sudden reaction | 106(38) | 80(28) | 54(19) | 20(7) | 22(8) | 2.1 | 1.23 |
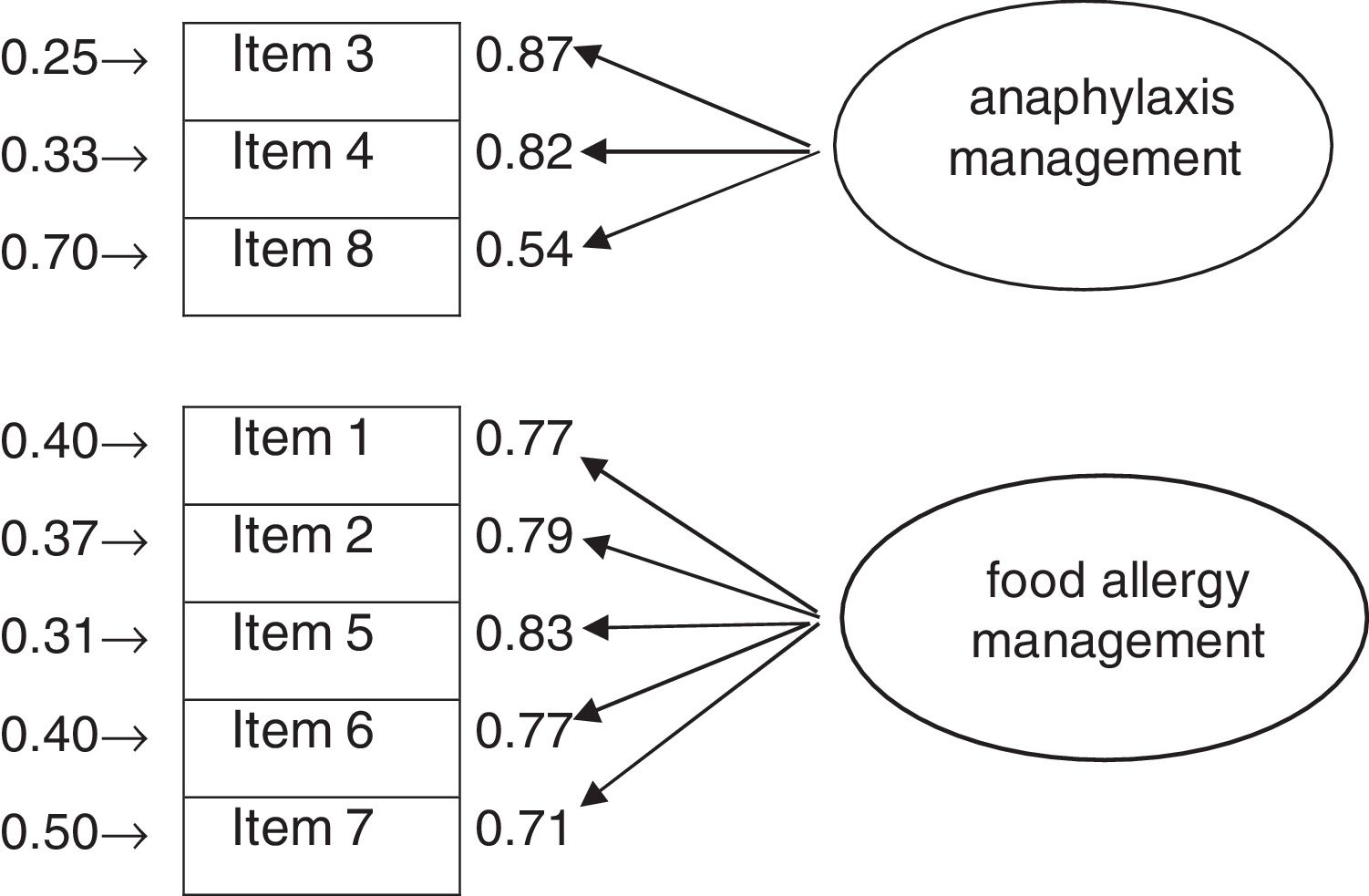
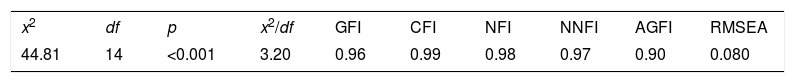
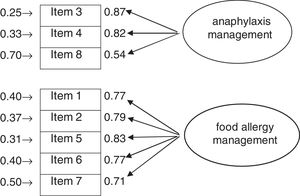
The CFA was applied to test the Turkish version of the two-factor original scale. The criteria defining the model fit are shown in Table 2. The two-factor model showed acceptable fit for most of the criteria (RMSEA=0.080, GFI=0.96, CFI=0.99, NFI=0.98, NNFI=0.97, AGFI=0.90, x142=44.81, x2/df=3.20, p<0.0010). The CFA results showed that the factor loadings of the factor 1 (anaphylaxis management) ranged from 0.54 to 0.87 and the factor loadings of the factor 2 (food allergy management) ranged from 0.71 to 0.83 (Fig. 1).
Model fit indices for confirmatory factor analysis.
| x2 | df | p | x2/df | GFI | CFI | NFI | NNFI | AGFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|
| 44.81 | 14 | <0.001 | 3.20 | 0.96 | 0.99 | 0.98 | 0.97 | 0.90 | 0.080 |
GFI: goodness of fit index; CFI: comparative fit index; NFI: normal fit index; NNFI: non-normal fit index; AGFI: adjusted GFI; RMSEA: root mean square error of approximation.
The discriminant validity of the SPSMFAA-T was investigated by examining whether the SPSMFAA-T could discriminate the teachers who had training on FA and anaphylaxis from the teachers who did not. The mean SPSMFAA-T score was 26.74±6.21 for the teachers who had training on FA and anaphylaxis and 22.18±7.48 for the teachers who did not have training on FA and anaphylaxis. The difference between the mean scores was significant (t=−3.608, p<0.001).
The total Cronbach's α of the eight-item scale was 0.91. Cronbach's α values of the anaphylaxis management and food allergy management subscales were 0.79 and 0.89, respectively. Item-total correlations ranged between 0.50 and 0.82 (p<0.001).
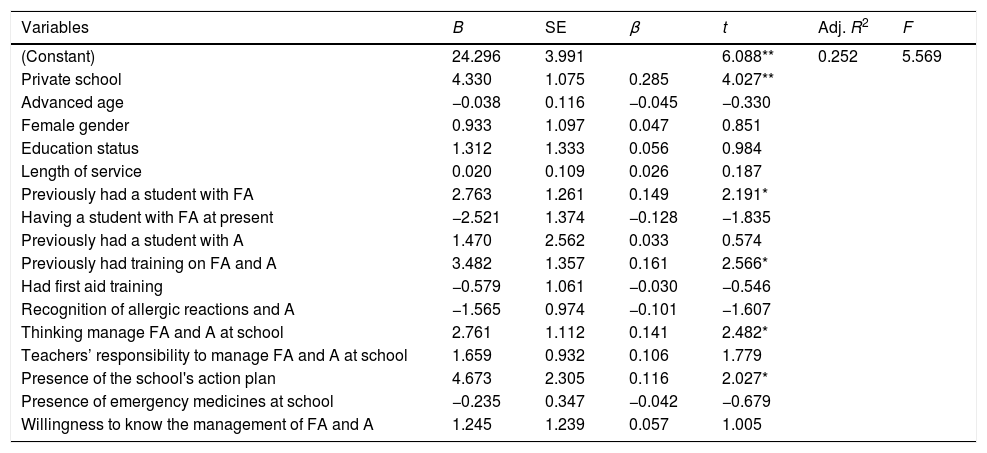
The results of the multiple regression analysis are shown in Table 3. According to the analysis, teachers who were working in a private school (β=0.285), previously worked a student with FA (β=0.149), previously had training on FA and anaphylaxis (β=0.161), thinking that he/she can manage FA and anaphylaxis at school (β=0.141) and had an action plan related to the management of FA and anaphylaxis in their school (β=0.116) showed increased self-efficacy scores in managing FA and anaphylaxis (R=0.502, F=5.569, p<0.001).
Multiple regression analysis of factors affecting teachers’ self-efficacy.
| Variables | B | SE | β | t | Adj. R2 | F |
|---|---|---|---|---|---|---|
| (Constant) | 24.296 | 3.991 | 6.088** | 0.252 | 5.569 | |
| Private school | 4.330 | 1.075 | 0.285 | 4.027** | ||
| Advanced age | −0.038 | 0.116 | −0.045 | −0.330 | ||
| Female gender | 0.933 | 1.097 | 0.047 | 0.851 | ||
| Education status | 1.312 | 1.333 | 0.056 | 0.984 | ||
| Length of service | 0.020 | 0.109 | 0.026 | 0.187 | ||
| Previously had a student with FA | 2.763 | 1.261 | 0.149 | 2.191* | ||
| Having a student with FA at present | −2.521 | 1.374 | −0.128 | −1.835 | ||
| Previously had a student with A | 1.470 | 2.562 | 0.033 | 0.574 | ||
| Previously had training on FA and A | 3.482 | 1.357 | 0.161 | 2.566* | ||
| Had first aid training | −0.579 | 1.061 | −0.030 | −0.546 | ||
| Recognition of allergic reactions and A | −1.565 | 0.974 | −0.101 | −1.607 | ||
| Thinking manage FA and A at school | 2.761 | 1.112 | 0.141 | 2.482* | ||
| Teachers’ responsibility to manage FA and A at school | 1.659 | 0.932 | 0.106 | 1.779 | ||
| Presence of the school's action plan | 4.673 | 2.305 | 0.116 | 2.027* | ||
| Presence of emergency medicines at school | −0.235 | 0.347 | −0.042 | −0.679 | ||
| Willingness to know the management of FA and A | 1.245 | 1.239 | 0.057 | 1.005 |
SE: standard error; FA: food allergy; A: anaphylaxis.
The results showed that most of the participating teachers never had a student with FA and that very few of them had a student who suffered anaphylaxis. The prevalence of FA is increasing not only in developed countries but also in Asian and African countries, which have developing economies and adopt western lifestyles.20 Because prevalence increases most in schoolchildren, it is important to determine teachers and other school employees’ self-efficacy on how to manage FA and anaphylaxis, especially in schools where health professionals are not available. In the present study, it was aimed to test the validity and reliability of the Turkish version of the SPSMFAA, a practical and valid measurement tool to assess school personnel's self-efficacy to manage FA and anaphylaxis.
For the psychometric testing of the SPSMFAA-T, first a multistage translation process of the scale was completed, and then its validity and reliability were assessed.18 The content validity of the scale was tested with the CVI. The scale was revised in line with the recommendation by a panel of experts after they reviewed and evaluated it. At least 80% compliance among experts was accepted as a criterion for CVI. In the present study, the results of the CVI analysis were above the determined criteria, which indicated that there was satisfactory agreement among experts and that the scale was appropriate for Turkish society.
According to the results of CFA, factor loads of scale items were higher than 0.30, which was similar to the factor load of the anaphylaxis management in the original study, but slightly higher than the factor load of the food allergy management.15 The results confirmed the two-factor structure of the original scale and demonstrated the relationship between the scale and its items. In the literature, it is recommended that CFI, GFI, NFI and AGFI should be higher than 0.90, RMSEA lower than 0.08, and x2/df between 0.2 and 0.5.21,22 In the present study, GFI, CFI, NFI and NNFI were greater than 0.90, x2/df was between 0.2 and 0.5, and RMSEA was 0.08. Of the fit indices, only the RMSEA was at the borderline. All the others were above the acceptable limits. Unfortunately, because the model fit indices were not given in the original study and there was no psychometric testing of the scale in a different culture in the literature, the results of the present study were not compared with those of other studies. These results confirmed the structure of the original scale and the relationship between the scale items and factors. In addition, the SPSMFAA-T successfully discriminated the teachers who previously had training on FA and anaphylaxis from the teachers who did not.
Cronbach's α, used to assess the reliability of the scale in a study, shows the relationship between the scale items and increases with strong correlations. The Cronbach's α (0.91) for the SPSMFAA-T was significantly higher than the generally agreed lowest limit value of 0.70. Unfortunately, this result was not compared with other results, because in the original study, no Cronbach's alpha value was specified for the overall SPSMFAA scale. This result was consistent with that (α=0.88) of the Food Allergy Self-Efficacy Scale for Parents (FASE-P), another tool developed to determine parents’ self-efficacy in managing FA.23 On the other hand, the Cronbach's alpha values (0.79 and 0.89) calculated for the subscales were very similar to the Cronbach's alpha values (0.75 and 0.85) of the subscales of the original SPSMFAA scale.15 As we expected, all the item-total correlations were higher than the proposed value (0.30–0.70).19 All these results showed that the scale had internal consistency in measuring the same targets.
The responses given to the items of the scale by the participants indicated that the teachers had high self-efficacy for the items “co-work with other professional and family in food allergy management at school” and “manage allergens avoidance”, and low self-efficacy for the items “recognize anaphylaxis symptoms” and “administer drugs to a student having a severe and sudden reaction”. Previous studies also showed that teachers had lower self-efficacy in anaphylaxis management.13,15 Evidence suggests that many cases of fatal anaphylaxis result from delayed onset of treatment, usually due to failure to recognize signs of allergy exposure, allergy symptoms, or early symptoms of anaphylaxis.14,24 Therefore, organizing programs to improve both self-efficacy and knowledge of school personnel regarding the management of FA and anaphylaxis will enable them to achieve this difficult task.14,15
This result showed that those teachers who were working in a private school, previously had a student with food allergy, previously had training on FA and anaphylaxis, and thought that he/she could manage FA and anaphylaxis at school, and whose schools had an action plan related to the management of FA and anaphylaxis had higher self-efficacy to manage FA and anaphylaxis. Other studies showed that self-efficacy of teachers who had students with FA was higher,15 that teachers working in private schools had more students with a history of acute allergy, and that these teachers were more aware of students with allergy.13 Another study showed that teachers’ knowledge of and attitudes toward FA and anaphylaxis, and their epinephrine administration skills could be improved through short-term training programs.25 These findings supported the view that teachers’ self-efficacy levels could be increased by improving their knowledge and awareness of and attitudes toward FA and anaphylaxis. In other words, that there was a relationship between the independent variables in this study and the teachers’ self-efficacy to manage FA and anaphylaxis confirms the validity and reliability of the scale. The scale can identify variables related to self-efficacy to manage FA and anaphylaxis.
The strength of the present study was that the teachers had different professional backgrounds. However, the study also had some limitations. The participants did not undergo a test–retest process. Convergent validity was not assessed. Besides, because there were no studies which carried out the psychometric testing of the scale in other languages, the results of this study were not compared with the results of studies from different cultures.
In conclusion, the present study results showed that the SPSMFAA-T was a valid and reliable measurement tool to assess teachers’ self-efficacy levels to manage FA and anaphylaxis. The SPSMFAA-T can be used by health professionals, researchers and clinicians to identify self-efficacy and influencing factors in health education programs to improve school personnel's skills to manage FA and anaphylaxis. It is also recommended that future studies should be performed in different socio-cultural groups and languages to carry out the psychometric testing of the SPSMFAA.
Ethics statementThis study was reviewed and approved by the Dokuz Eylül University Ethical Committee.
Financial supportThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors declare that they have no conflict of interest.