Background. Treatment of gastric varices (GV) implies a number of several difficulties and sometimes entails complications. The best endoscopic success rate was attributed until now to the use of tissue adhesives(N-Butyl-2-Cyanoacrylate) and band ligation.
Aim. To assess the therapeutic efficacy and safety of cyanoacrylate injection compared to band ligation in patients with acute GV hemorrhage.
Material and methods. Thirty-seven patients with upper gastrointestinal bleeding from GV were included in the study, treated with cyanoacrylate injection (GVO)-19 patients or band ligations (GVL)-18 patients. They were followed up for overall results, complications and survival rate.
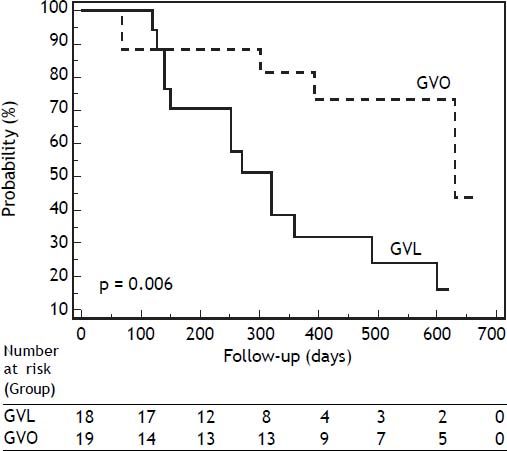
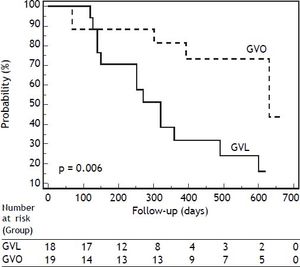
Results. The mean age of the study group was 60.22 ± 9.34 years, with a male/female ratio of 21:16. The mean follow-up period was 427.26 ± 214.16 days in the GVO group and 406.21 ± 213.23 days in the GVL group (p = 0.76). Initial hemostasis was achieved in all patients treated with cyanoacrylate and in 88.88% from the GVL group (p = 0.43). Rebleeding occurred in 72.22% of the GVL group and in 31.57% of the GVO patients (p = 0.03). Patients in the GVO group had a significantly larger rebleeding-free period(p = 0.006). No difference was found in survival rates(p = 0.75). The Child Class (p = 0.003 for Class C) and treatment method (p = 0.01) were independently associated with the rate of rebleeding. No differences were found regarding the rate of complications.
Conclusion. The use of cyanoacrylate in acute GV bleeding had better results when compared with band ligation in terms of controlling the hemorrhage and recurrence of bleeding. The overall survival rate was not influenced by the method used for the treatment of complicated GV.
Variceal hemorrhage is responsible for up to 10% of upper-GI bleedings.1 Among patients with cirrhosis, mortality due to bleeding from varices reaches 10-30%.2,3 Rebleeding may appear if no therapeutic intervention is performed and it has the highest rate during the first 6 weeks, requiring a reliable secondary prophylactic strategy.4 Gastric varices (GV) are less common than esophageal varices (EV), yet they may be present in up to 20% of patients with portal hypertension, and 4 to 65% of gastric varices will bleed over a period of 2 years after the diagnosis.5,6 The prognosis of GV is poorer, as they are associated with more severe blood loss, a higher rebleeding rate and consequently, a higher mortality rate.4,7 The best treatment for acute bleeding from GV is still under evaluation. One of the alternatives of endoscopic treatment is the injection of sclerosing agents or, more recently, tissue adhesives such as N-Butyl-2-cyanoacrylate (GVO), which appears to have a higher success rate than other sclerosing substances. The other therapeutic option would be band ligation (GVL), which is considered the optimal endoscopic treatment in case of EV hemorrhage, but the efficacy of band ligation in gastric varices bleeding is still uncertain. On the other hand, both methods involve complications and/or technical difficulties, which have to be considered carefully when making a therapeutic decision. There are few studies comparing band ligation with tissue adhesives and the results seem to be in favor of GVO.8,9
Our aim was to assess the therapeutic efficacy and safety of cyanoacrylate injection compared to band ligation in patients with acute GV hemorrhage as a complication of liver cirrhosis of different etiologies.
Material and MethodsStarting with January 2010 and until December 2012, 37 patients with liver cirrhosis and gastrointestinal bleeding from GV were included in the study (in our department, about two hundred and forty upper gastrointestinal hemorrhages from varices are admitted every year). The inclusion criterion in this study was the gastrointestinal bleeding form gastric varices in cirrhotic patients. Patients presented in the emergency room of the Regional Institute of Gastroenterology and Hepatology, Cluj-Napoca, for acute gastrointestinal bleeding or they were already admitted to this institute for cirrhosis decompensation, when they developed gastrointestinal hemorrhage. They all underwent emergency endoscopy (in the first 12 h), and they all received one of the above mentioned treatment method: GVL or GVO, using an adaptive biased-coin randomization.
During the study period, there were 59 patients admitted in our department for GV bleeding. Twenty-two patients were excluded from the study for the follow-ing reasons:
- •
Previous endoscopic treatment (4 patients), surgical treatment (1 patient), or transjugular intrahepatic portal systemic shunt for GVH (1 patient).
- •
Heart failure, uremia, chronic obstructive pulmonary disease, malignancies (other than hepatic), terminal illness of any major organ system (11 patients).
Five cases with concomitant large EV, but without stigmata of recent bleeding, were also excluded from this study, because the source of bleeding could not be specified precisely. The variceal bleeding of non-cirrhotic etiology was considered outside the inclusion criteria of this observation.
Liver cirrhosis was diagnosed based on clinical, biochemical, and imaging findings of portal hypertension and hepatic failure. At the time of enrollment, the severity of liver disease was established according to the Child-Pugh classification.10
GV bleeding was diagnosed using the following criteria:
- 1.
Clinical signs of bleeding (hematemesis, melena, coffee ground vomiting, or hematochezia).
- 2.
Endoscopic visualization of oozing or spurting, adherent blood clots, white nipple signs, or erosions from or on the GV.
- 3.
Presence of distinct large GV with red-color signs and no other identifiable source of bleeding.11–13
The classification of gastric varices was based on the criteria elaborated by Sarin, et al.5 gastro-esophageal varices (GOVs) are associated with esophageal varices along the lesser curve (type 1, GOV1), or along the fundus (type 2, GOV2). Isolated gastric varices (IGVs) are present in isolation in the fundus (IGV1) or at ectopic sites in the stomach or the first part of the duodenum (IGV2).
Vasoactive drugs (terlipressin or somatostatin analogs) were started before diagnostic endoscopy. All patients received antibiotic prophylaxis (Cephotaxime 1g/day or Norfloxacine 400 mg/day i.v.) according to the guidelines.13
The procedures for the endoscopic control of varieal bleeding were performed in the retroflexed position, using an Olympus GF-Q165 endoscope (Olympus Optical Co. Ltd, Tokyo, Japan) and a 23-gauge disposable injection needle (EIS 01943, Top Co.).
Intravariceal injections with N-butyl-2-cyaoacrylate Glubran (GEM S.r.l., Viareggio, Italy) were used. The injections were performed on actively bleeding varices and/or those with stigmata of the bleeding. Each injection contained dilutions of 0.5 mL cyanoacrylate and 0.5 mL Lipiodol (Guerbet Laboratory, Aulnay-Sous-Bris, France), the total dose of 1.0 mL cyanoacrylate given at a time being necessary for an effective therapy. Following the injection, the needle together with the scope were withdrawn, the needle being cut without any risk of damage. After each procedure, the endoscopist checked for the effectiveness of the injections by gently touching the varices newly treated with cyanoacrylate with a blunt catheter. A hard fill was considered as a sign of an effectively obliterated vessel.
Ligation was performed using an Olympus GF-Q165 endoscope (Olympus Optical Co. Ltd, Tokyo, Japan). No more than 6 rubber bands were applied in each session. The bleeding site was ligated first, and then the other large varices were also ligated. All the endoscopists implied in this study were equally trained in both therapeutic procedures.
Data were also collected regarding age, vital signs, blood transfusions, causes of portal hypertension, grade and size of the varices, ascites, concomitant hepatocarcinoma.
Clinical evaluations, liver function tests and serum alpha-fetoprotein measurements were performed every 3 months. After obliteration of gastroesophageal varices, endoscopy was performed every 6 months to detect recurrence of varices. Initial hemostasis was defined as cessation of bleeding for more than 5 days. The definition of rebleeding was recurrence of hematemesis or melena and the bleeding source from gastric varices proven by emergency endoscopy. The clinically significant rebleeding was defined as upper GI hemorrhage occurring 5 days after the endoscopic treatment or as active hemorrhage that occurred after endoscopic treatment in patients presenting with stigmata of recent hemorrhage. Only those who had a 3 g/dL drop in hemoglobin levels and required blood transfusion of 2 or more units were considered to have rebleeding.11 Patients who presented with insignificant bleeding such as scanty tarry stool and clear aspirates from a nasogastric tube but who did not need blood transfusions were not considered to have rebleeding. Endoscopy was performed in order to identify the cause and to control the bleeding. In patients presenting with both esophageal varices and gastric varices, the origin of the bleeding from gastric varices was determined based on the aspect of varices, depending on whether the ulcers on the GV were coated with blood clots or not. In case of recurrent varices or rebleeding from varices, repeated sessions of treatment, the same as the original one, were performed. Transfusion of blood was considered necessary in case of hemoglobin concentrations lower than 7 g/dL, or in order to keep hemodynamics stable when a patient bled actively. The data on the need of blood transfusions were recorded for the patients included in this study during hospitalization. Complications were defined as any special event that required active treatment or prolonged hospitalization. Treatment failure in the acute setting was defined as death or other events that required the change of therapy in patients exhibiting one of the following criteria: fresh hematemesis or naso-gastric aspiration of ≥ 100 mL of fresh blood more than 2 h after the start of a specific drug treatment or therapeutic endoscopy; development of hypovolemic shock; 3 g-drop in Hb within any 24 h period if no transfusion is administered.11 All patients were recommended treatment with beta blockers for the prophylaxis of a new episode of rebleeding 5 days after the control of bleeding. We used nonselective beta-blockers (propranolol) for the secondary prophylaxis of bleeding in all patients, except for one patient from the GVL group who received Carvedilol.
A complete, comprehensive and clear informed consent was provided to and signed by all patients, after a detailed discussion regarding the procedure, complications and treatment alternatives with the patients or their relatives, considering the risks associated with the procedure. This study was approved by the Ethics Committee of our hospital and it was performed in full accordance with the Declaration of Human Rights (Helsinki, 1975) and with its further revisions.
We used for the statistical analysis the MedCalc® 9.3.9.0. software and SPSS software version 15.0 (SPSS Inc. Chicago, IL, USA). The continuous variables were tested for normality of distribution using Kolmogorov-Smirnov test. The variables with normal distribution were presented as median ± standard deviation (SD). The variables with non-normal distribution were presented as medians and 95% confidence interval (95% CI). The Student’s t test, χ2 test, and Fisher’s exact test were used to assess the differences between both groups with respect to clinical data and variceal recurrence and rebleeding in case of variables with normal distribution. The Mann-Whitney U test was used for the comparison of continuous variables with non-normal distribution. KaplanMeier estimation was applied to represent the time of first occurrence of recurrent bleeding from gastroesophageal varices or the time of occurrence of other events or death. The Log rank test was used to compare the survival curves and the variation of rebleeding episodes. Risk factors for recurrent bleeding were assessed using univariate analysis and Cox proportional hazard regression. All p values were 2-tailed. A p value < 0.05 was considered significant.
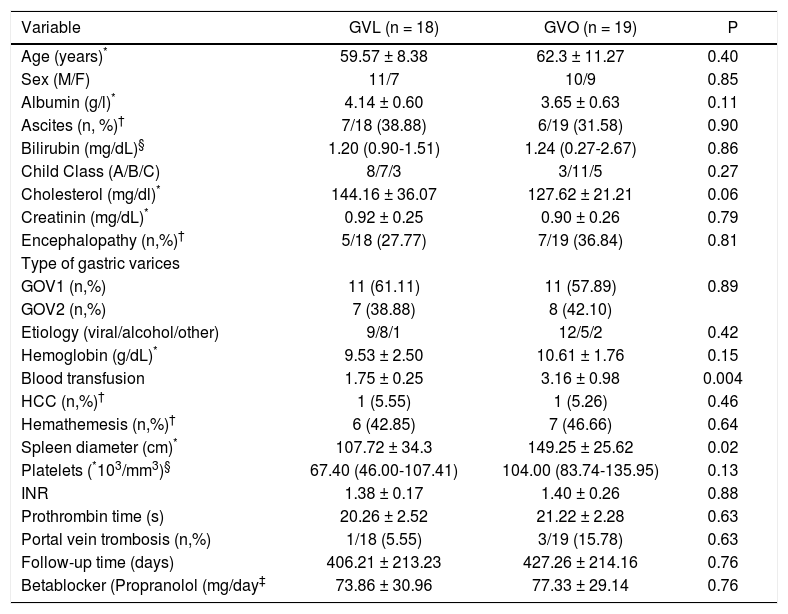
ResultsDuring the study period, 37 patients with GV bleeding meeting the inclusion criteria were enrolled from our unit. Of these, 19 were treated with cyanoacrylate, while 18 patients were treated with band ligation. Two patients presented associated hepatocellular carcinoma (HCC), one from each group (GVO, respectively GVL). Sixteen patients in the GVO group and fifteen in the GVL group had concomitant EV or had prior EV. The type of gastric varices was distributed as follows: among the GVO group, 11 (57.89%) patients were GOV1, 8 (44.44%) patients were GOV2, and no patient had isolated gastric varices. Among the GVL group, 11 (61.11%) patients were GOV1, 7 (38.88%) patients were GOV2 and no patient had isolated gastric varices. The characteristics of both groups are shown in table 1.
Characteristics of the study group.
| Variable | GVL (n = 18) | GVO (n = 19) | P |
|---|---|---|---|
| Age (years)* | 59.57 ± 8.38 | 62.3 ± 11.27 | 0.40 |
| Sex (M/F) | 11/7 | 10/9 | 0.85 |
| Albumin (g/l)* | 4.14 ± 0.60 | 3.65 ± 0.63 | 0.11 |
| Ascites (n, %)† | 7/18 (38.88) | 6/19 (31.58) | 0.90 |
| Bilirubin (mg/dL)§ | 1.20 (0.90-1.51) | 1.24 (0.27-2.67) | 0.86 |
| Child Class (A/B/C) | 8/7/3 | 3/11/5 | 0.27 |
| Cholesterol (mg/dl)* | 144.16 ± 36.07 | 127.62 ± 21.21 | 0.06 |
| Creatinin (mg/dL)* | 0.92 ± 0.25 | 0.90 ± 0.26 | 0.79 |
| Encephalopathy (n,%)† | 5/18 (27.77) | 7/19 (36.84) | 0.81 |
| Type of gastric varices | |||
| GOV1 (n,%) | 11 (61.11) | 11 (57.89) | 0.89 |
| GOV2 (n,%) | 7 (38.88) | 8 (42.10) | |
| Etiology (viral/alcohol/other) | 9/8/1 | 12/5/2 | 0.42 |
| Hemoglobin (g/dL)* | 9.53 ± 2.50 | 10.61 ± 1.76 | 0.15 |
| Blood transfusion | 1.75 ± 0.25 | 3.16 ± 0.98 | 0.004 |
| HCC (n,%)† | 1 (5.55) | 1 (5.26) | 0.46 |
| Hemathemesis (n,%)† | 6 (42.85) | 7 (46.66) | 0.64 |
| Spleen diameter (cm)* | 107.72 ± 34.3 | 149.25 ± 25.62 | 0.02 |
| Platelets (*103/mm3)§ | 67.40 (46.00-107.41) | 104.00 (83.74-135.95) | 0.13 |
| INR | 1.38 ± 0.17 | 1.40 ± 0.26 | 0.88 |
| Prothrombin time (s) | 20.26 ± 2.52 | 21.22 ± 2.28 | 0.63 |
| Portal vein trombosis (n,%) | 1/18 (5.55) | 3/19 (15.78) | 0.63 |
| Follow-up time (days) | 406.21 ± 213.23 | 427.26 ± 214.16 | 0.76 |
| Betablocker (Propranolol (mg/day‡ | 73.86 ± 30.96 | 77.33 ± 29.14 | 0.76 |
Both groups were comparable regarding age, gender, etiologies of portal hypertension and severity of liver disease. The size of esophageal varices and gastric varices before performing endoscopic therapy was also similar between both groups. The mean follow-up period was 427.26 ± 214.16 days in the GVO group and 406.21 ± 213.23 days in the GVL group (p = 0.76). The dose of propranolol for the secondary prevention of bleeding did not differ in the two subgroups.
Initial hemostasis was achieved in all the patients treated with cyanoacrylate and in 88.88% of the patients treated with band ligation; in the two patients who could not achieve hemostasis by band ligation the use of balloon tamponade was necessary. The team attentively manipulated the scopes and there was no damage to the equipment during the use of cyanoacrylate.
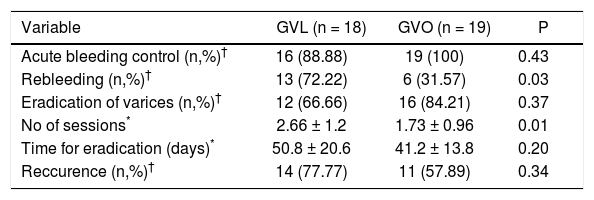
The results of the initial hemostasis are presented in table 2. The rebleeding rate was significantly higher in the GVL group as compared with the GOV group: 72.22% vs. 31.57%, p = 0.03. The probability of rebleeding from GV is shown in figure 1. The results showed that the patients who received treatment with tissue adhesive had a significantly larger rebleeding-free period when compared to patients treated with band ligation (p = 0.006). The rebleeding rate was higher in the GVL group regardless of the GOV type subgroup. Two patients in the GVO group were treated later using transjugular intrahepatic porto-systemic stent shunts. Blood transfusion requirements were significantly higher in the GVL group compared to GVO group (3.16 vs. 1.75 units, respectively) (p = 0.004).
The results of hemostasis and of endoscopic treatment of varices.
| Variable | GVL (n = 18) | GVO (n = 19) | P |
|---|---|---|---|
| Acute bleeding control (n,%)† | 16 (88.88) | 19 (100) | 0.43 |
| Rebleeding (n,%)† | 13 (72.22) | 6 (31.57) | 0.03 |
| Eradication of varices (n,%)† | 12 (66.66) | 16 (84.21) | 0.37 |
| No of sessions* | 2.66 ± 1.2 | 1.73 ± 0.96 | 0.01 |
| Time for eradication (days)* | 50.8 ± 20.6 | 41.2 ± 13.8 | 0.20 |
| Reccurence (n,%)† | 14 (77.77) | 11 (57.89) | 0.34 |
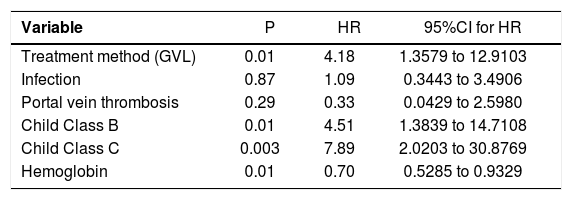
Factors associated with rebleeding in univariate analysis were treatment method, level of hemoglobin and the severity of the disease as expressed by Child class as the results of Cox proportional hazard regression showed (Table 3). The patients with Child class C of severity had a 7.8-fold higher probability to experience a new episode of rebleeding, and those from Child class B a 4.5-fold higher probability. Patients who were treated with band ligation had a 4.1- fold higher probability to rebleed as compared to those treated with cyanoacrylate. A decrease of hemoglobin with 1 g/dL determined a 30% higher probability of rebleeding.
Cox proportional-hazards regression of risk factors for rebleeding.
| Variable | P | HR | 95%CI for HR |
|---|---|---|---|
| Treatment method (GVL) | 0.01 | 4.18 | 1.3579 to 12.9103 |
| Infection | 0.87 | 1.09 | 0.3443 to 3.4906 |
| Portal vein thrombosis | 0.29 | 0.33 | 0.0429 to 2.5980 |
| Child Class B | 0.01 | 4.51 | 1.3839 to 14.7108 |
| Child Class C | 0.003 | 7.89 | 2.0203 to 30.8769 |
| Hemoglobin | 0.01 | 0.70 | 0.5285 to 0.9329 |
HR: hazard ratio. 95% CI: 95% Confidence Interval.
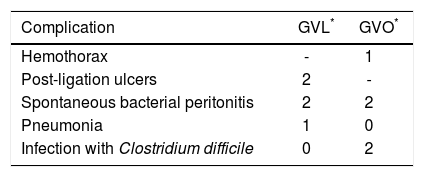
Regarding the complications in the GVO group, one patient presented intense thoracic pain after injection, but the suspicion of pulmonary embolism was refuted by CT scan or angiography. An extravasation of contrast in the left pleura and around the spleen was seen during the investigation for the thoracic pain. The pleural effusion was probably represented by a hemothorax, but the volume was clinically and radiologicaly insignificant. No drain puncture or special treatment was needed, except for the usual therapy for the complicated cirrhotic disease, the symptoms and the pleural effusion resolved conservatively.
Other common complications reported, besides rebleeding from the ulcers which developed after band ligation in 2 cases (11.11%), were infections, spontaneous bacterial peritonitis (4 patients), pneumonia (1 patient) and digestive infection with Clostridium difficile (2 patients). Three of the infections were reported in the GVL group and 4 cases complicated with infections were part of GVO group (Table 4).
The mortality in the two studied groups was not significantly different, even if the rate of rebleeding was lower in the group treated with cyanoacrylate. There were two patients who died in each group, because of hepatic failure and variceal bleeding (p = 0.75). The method used for treatment did not influence the development of encephalopathy or ascites (p = 0.76, p = 0.57).
DiscussionThe results of our study showed that the treatment of bleeding from GV with cyanoacrylate is more efficient than band ligation even if there are no significant differences in mortality. Bleeding is commonly more severe and difficult to control in case of gastric varices rupture as compared to bleeding from the esophageal site. Moreover, the treatment of gastric variceal hemorrhage is still challenging, as the sclerosants used for control of the bleeding from a gastric source have disappointing results, as opposed to treatment of esophageal varices bleeding.6 Sclerotherapy in gastric variceal bleeding is associated with a higher incidence of complications, such as gastric ulcerations and perforation and recurrent bleeding rates range between 37% and 53%.5,7 The most appropriate therapy for the bleeding from gastric varices is still under debate, even if most of the studies confirmed that injection of tissue adhesive gives better results than to sclerotherapy and band ligation. However, the glue therapy is not an easy technique to perform, as it requires experience and sometimes entails important complications, making the decision of the therapeutic approach of bleeding gastric varices still difficult. Our study aimed to assess the results of the first Romanian series of patients treated with Glubran using the comparison with a group treated with band ligation.
Variceal band ligation has already taken the first place in the treatment and prevention of esophageal variceal bleeding and rebleeding since it proved to be more efficient. This technique can also be performed in gastric bleeding, since banding in both retro-flexed and non-retroflexed positions can be performed. Band ligation in gastric pathology is indicated in actively bleeding varices. Most of the studies reported four bands as being sufficient to apply in one session.8
The rate of hemostasis using band ligation in acute hemorrhages has been reported to be 83-100%.12–14 Other authors reported a control rate of acute bleeding of 100 % in 18 patients for a combination between ligation and sclerotherapy (1-9 ligations plus 1% polidocanol injected in the surrounding submucosa).13–15 This combination between ligation and sclerotherapy is unlikely to be accepted for the management of acute bleeding because of the risk of iatrogenic complications, the need for greater technical skill and the increase in procedure time.
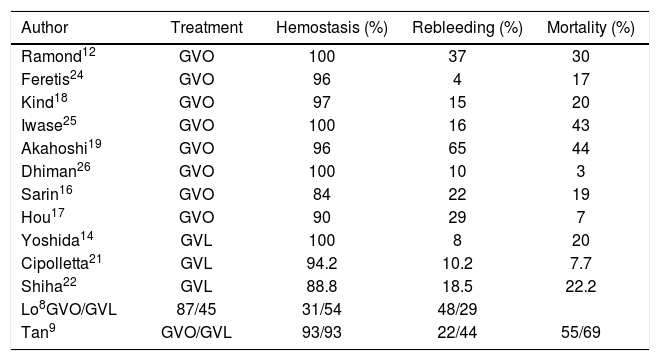
When comparing the two treatment methods, GVO proved to be superior to band ligation for acute GV bleeding with higher initial hemostasis and lower rebleeding rates.8,9 As shown by Lo et al, on 26 patients with active bleeding and 34 with stigmata of recent hemorrhage, initial hemostasis was significantly better in the cyanoacrylate group (87 vs. 45%).8 In most series, the initial hemostasis by cyanoacrylate is at least 90%.9,16–19 The rebleeding rate of GVO is approximately 22-37%.9,16,17 The GVO is more effective in achieving variceal obturation, with a higher initial hemostasis and less need for surgery than sclerotherapy.16,20 A randomized controlled trial demonstrated higher cumulative survival rate of GVO compared to band ligation.8 In another important study in terms of the number of patients enrolled and a large proportion of patients with IGV1, hemostasis was achieved in over 90% of patients, with both methods.9 The authors attributed the better efficacy of GVL, as compared to the data reported in other studies, to a greater number of bands used (4-5 vs. 1-2 bands). There was no difference in bleeding-related mortality in both mentioned trials. This study is important, as it is one of the largest controlled studies on patients with gastric variceal hemorrhage9 and illustrates how a good technique can significantly influence the outcomes of hemostasis particularly for GVL. On the other hand, the evidence for the use of GVL for acute gastric variceal bleeding is mixed. There were initially a number of case series showing that band ligation was safe and effective for acute GV bleeding,14,21–23 but later randomized controlled trials demonstrated that band ligation had lower initial hemostasis and higher rebleeding rates.8,9 The rebleeding rate at the 2nd and 3rd years was 63 and 72% respectively for patients undergoing band ligation.8 As mentioned before, there is only one study showing the same efficacy for the two methods. A review of the data in literature regarding the comparison of endoscopic outcomes and mortality related to the occlusion and ligation of bleeding GV is presented in table 5.
Outcomes of hemostasis, rebleeding and mortality after endoscopic treatment of GV bleeding (GVO and GVL), as reported in previous articles.
| Author | Treatment | Hemostasis (%) | Rebleeding (%) | Mortality (%) |
|---|---|---|---|---|
| Ramond12 | GVO | 100 | 37 | 30 |
| Feretis24 | GVO | 96 | 4 | 17 |
| Kind18 | GVO | 97 | 15 | 20 |
| Iwase25 | GVO | 100 | 16 | 43 |
| Akahoshi19 | GVO | 96 | 65 | 44 |
| Dhiman26 | GVO | 100 | 10 | 3 |
| Sarin16 | GVO | 84 | 22 | 19 |
| Hou17 | GVO | 90 | 29 | 7 |
| Yoshida14 | GVL | 100 | 8 | 20 |
| Cipolletta21 | GVL | 94.2 | 10.2 | 7.7 |
| Shiha22 | GVL | 88.8 | 18.5 | 22.2 |
| Lo8GVO/GVL | 87/45 | 31/54 | 48/29 | |
| Tan9 | GVO/GVL | 93/93 | 22/44 | 55/69 |
GVO: gastric variceal occlusion (using cyanoacrylate). GVL: gastric variceal ligation.
Our study has similar results in terms of the initial hemostasis, when compared to the studies existing until now in literature: for GVO, the success rate was 100%, while the rate of control using band ligation was 88.88%. Regarding the type of gastric varices, GOV2 type was met in 42.1% of GVO group and 38.8% in the GVL group with no significant difference between the two groups regarding the distribution of gastric varices. On the other hand, the study enrolled prospectively and consecutively all the patients with bleeding from gastric varices, the therapy in this pathology not having a standard of care as yet.
The results regarding the efficacy of glue were compared not only to band ligation but also to other sclerosants. Most of the results for the use of cyanoacrylate in gastric variceal bleeding come from Japan, USA and Europe, who report initial hemostasis rates of more than 90%.18,19,25,26–28 Oho, et al. performed a non-randomized prospective study on 53 patients with acute gastric variceal bleeding. Glue achieved significantly better hemostasis (93 vs. 67%).20 In a retrospective study, Ogawa, et al. also found significantly better hemostasis with glue29 and Sarin, et al. also confirmed a better hemostasis (89 vs. 62%) with glue when compared with alcohol.16
The recurrence of gastric varices in our study was higher compared to other reports: 77.7% in the GVL group and 57.8% in the GVO group, maybe because of a subjective opinion of the operator. The rate of recurrence for the treatment with cyanoacrylate in another study was of 22.58%.9 The reported rate of rebleeding published in previous studies is 18-31% for the use of tissue adhesive. Our results showed a rebleeding rate of 31.57% in this group, while after band ligation there was 72.22% rebleeding rate, values higher than the percentage reported in some studies that also analyzed band ligation as a treatment option.9
In our study group, the factors associated with the possibility of rebleeding were the level of hemoglobin, the severity of the disease as expressed by Child class and the method used for bleeding control, with a significantly higher rate of control in the group treated with cyanoacrylate. Other studies reported HCC as having a significant influence on the occurrence of rebleeding.17 In our observation, there was only one patient in each group having HCC and it is difficult to obtain statistical significance with such a low prevalence. Regarding the severity of the disease in the two study groups and the chances of rebleeding, even if the level of hemoglobin was not different, the amount of transfusions was significantly higher in the GVO, suggesting a more severe hemorrhage in the subgroup treated with cyanoacrylate, which makes the obliteration method more efficient considering the significantly better results in this group in terms of controlling the bleeding and preventing the rebleeding. This advantage might also have an impact on mortality in a larger study group.
A number of complications have been reported in association with cyanoacrylate injection. Common complications associated with GVO are pyrexia and abdominal pain/discomfort. Severe complications after GVO are mostly associated with systemic thromboembolic phenomena such as cerebral, pulmonary (5%, non-fatal), coronary, portal vein embolization and splenic infarction.30–33
In our study group, no thrombotic event occurred. In the GVO group, one patient presented intense thoracic pain after injection, but the suspicion of pulmonary embolism was not confirmed by CT scan or angiography. An extravasation of contrast in the left pleura was revealed during the investigation and it was interpreted as hemothorax, with a favorable evolution without any special intervention addressed to this complication.
For the band ligation, the most frequent complication is rebleeding from ulcers caused by ligation, which occurred in two study patients, representing a percentage of 14.28%, similar to the data reported in literature. On the other hand, band ligation is limited by the technique and the difficulties related to the position of varices.
Another frequent complication in these patients is infection. It has been documented that 35-60% of cirrhotic patients with variceal hemorrhage will develop bacterial infection.34 In our study, both groups had an important prevalence of infection, with no significant difference between them. The similar rate of infection in both groups does not seem to be related to the procedure, but rather to the bleeding itself.
Even in the presence of an important influence on the rebleeding rate for the two types of treatment, the survival rate was not different in the two study groups (2 patients died in each group). One patient in our study group died because of the recurrence of bleeding and the decompensation of the disease in this context. Liver failure was the cause of death for the other patients lost in our study. The mortality rate reported in other studies was up to 43% in GVO group and 69% in GVL group (Table 5), higher than our results, but our study included fewer patients and the results might be influenced by this variable.
Our research has some strengths: it is the first report, to our knowledge, on data of patients treated with Glubran in Romania, with results being followed up for more than one year. An important aspect is that all patients received treatment at the time of the acute event. On the other hand, we are aware of the study limitations, the most important being the small number of patients included in both groups and the short time tracking for the assessment of long-term outcomes.
In conclusion, the results of this study stand as a good evidence for the efficacy of tissue adhesives in the management of acute gastric variceal bleeding and their superiority when compared with band ligation. The rebleeding rate is significantly influenced by the use of tissue adhesives, but the technique requires some skill and care in order to prevent damage to the equipment. As the complications are rare and the success rate and long-term results are good, the technique seems to be recommendable for the bleeding of gastric varices. Nevertheless, the overall survival rate is not influenced by the method used for the control of GV bleeding. Considering the various endoscopic approaches and at the same time the combined therapies reported more frequently lately, further studies are needed to establish the best treatment for acute bleeding from gastric varices.
Conflict of InterestStatement regarding the conflict of interest: None declared.