The worldwide obesity epidemic contributes to the increasing incidence of a number of diseases, as nonalcoholic fatty-liver disease (NAFLD) and its most severe form, the nonalcoholic steatohepatitis (NASH). Data on the prevalence of NASH has varied from 18.5%4to 69%43 in obesity, an unacceptable wide range. The aim of our study was to evaluate how prevalence of NASH is influenced by the different diagnostic histological criteria. Consecutive assessment of 325 obese patients referred for bariatric surgery (BMI ≥ 35 kg/m2), 146 of whose were submitted to histological analysis of the liver allowed the evaluation of the prevalence of NAFLD. Steatohepatitis was diagnosed histologically using 3 types of criteria: a) broad criteria, where steatosis was associated with at least 2 of the following parameters: any degree of lobular inflammatory infiltrate, hepatocellular ballooning and perisinusoidal/ perivenular fibrosis; b) restricted criteria, where the hepatocellular ballooning was of moderate or severe intensity; c) ultrarestricted criteria, which required perisinusoidal and/or perivenular fibrosis. NAFLD was present in 111 (76%) of the patients, and the prevalence of NASH was 25.3% when ultrarestricted criteria were used, 41.1% with restricted criteria and 55.5% with broad criteria. In conclusion, more accurate definition of the criteria for histological diagnosis of NASH should be required, so that further clinico-pathological studies may define the long-term progression of the disease and evaluate therapeutic strategies.
Obesity, which is defined as Body Mass Index (BMI) ≥ 30kg/m5, has grown in epidemic proportions throughout the world.1-2 Clinical findings of liver alterations consistent with nonalcoholic fatty-liver disease (NAFLD) are common in the obese.3-6 This phenomenon has been described as a liver disease with a broad spectrum of presentation ranging from a simple steatosis to steatohepatitis,7 the condition which has the greatest impact on the disease’s progression and which can evolve into cirrhosis and hepatocellular carcinoma.8-12
NAFLD is frequently associated with severe obesity (defined as BMI > 35 kg/m2) and can be found in 74 -96% of liver biopsies in this population.13,14 Nonalcoholic Steatohepatitis (NASH) was described by Ludwig (1980)15 as being histologically similar to alcoholic hepatitis, although less aggressive. It is very common in the obese and is characterized by inflammation of the parenchyma, hepatocellular ballooning on zone 3 and/or fibrosis in addition to macrovesicular steatosis.16,17
Histology of the liver plays a fundamental role in establishing not only the presence but also the type and intensity of the inflammatory process and the fibrosis. These findings, together with steatosis, are needed for steatohepatitis to be diagnosed.17-19 There is divergence among pathologists, however, as to the histological findings required for the diagnosis of NASH.18-20-21 Many studies have endeavored to define the prevalence of NASH;22 the range of methodologies used and populations studied, however, has led to heterogeneous results.23,24 Our aim was to evaluate how prevalence is influenced by the use of escalating restrictiveness to the criteria for histological diagnosis of NASH in obese bariatric patients.
Patients and methodsIn this transversal study, 325 patients referred for bariatric surgery in a center for surgical treatment of obesity were assessed consecutively during three years. Patients were of both sexes, had BMI ≥ 35 kg/m2 and had been referred for surgery due to failure to respond to clinical treatment or due to other medical and/or physical conditions that compromised their quality of life. None of the patients presented a previous history of liver disease, and all underwent extensive clinical and biochemical assessment by a multidisciplinary team. Information concerning alcohol use was supplied by the patient or the patient’s family members; male patients with a daily intake of ethanol > 30 g or females with a daily intake > 20 g were considered alcoholics.
The following exclusion criteria were used: biopsies unsuitable for histological analysis, positive serology for HCV, use of medication that causes steatohepatitis25 and suspected liver disease indicated by histology.
Demographic data and anthropometric measurements such as sex, age, weight, height and BMI, calculated as weight (kg) divided by height2 (m) were obtained during preoperative visits.
Patients were assessed for the presence of the following comorbidities: (1) fasting glucose ≥ 110 mg/dL or diabetes mellitus type 2 or if there was a previous history of diabetes and/or the use of hypoglycemics or insulin (according to the criteria established by the American Diabetes Association - ADA, 2002)26 (2) central obesity (BMI ≥ 30 Kg/m2); (3) high blood pressure (HBP) if arterial pressure ≥ 130/85 mmHg or pharmacologically treated, as assessed by a cardiologist; (4) triglyceride levels ≥ 150 mg/dL or current use of fibrates; and (5) HDL-cholesterol < 40 mg/dL (men) and < 50 mg/dL (women). The 5 components of the metabolic syndrome were available, and 3 or more of the criteria were needed for the diagnosis according to ATP III.27
Serological tests for HCV and HBV were performed on all the patients. Studies to exclude other liver diseases such as hemochromatosis, a1pha-antitrypsin deficiency, Wilson’s disease or autoimmune disease were only requested if the liver biopsy was suggestive of these conditions.
This study was approved by the Ethical Committees of the hospitals in which the surgeries were performed. Patients gave their informed written consent.
Histological Analysis. The biopsied fragment was fixed in formol-saline (10%), then embedded in paraffin and processed with the following stains: hematoxilineosin; Masson’s trichrome, silver salts for impregnation of reticulin fibers and Perls.
Histological assessment was carried out by two hepatopathologists who were unaware of the patients’ clinical and laboratory data. The degree of macro and microvesicular steatosis was classified from 0 to 4 according to intensity: 0+ (0-10%), 1+ (10-25%), 2+ (25-50%), 3+ (50-75%), 4+ (> 75%). The other markers such as hepatocellular ballooning, lobular and portal inflammatory infiltrate, ductal metaplasia, nuclear vacuolation, Mallory’s hyaline and excess iron were semiquantified from 0 to 4 as follows: 0 = absent; 1 = scarce or a very small number of cells; 2 = moderate;
3 = marked; 4 = very marked.28 Fibrosis was classified according to its location as perivenular, perisinusoidal, septal and portal, and within each of these categories it was graded from 0 to 4 according to its intensity.29 All these markers together compound the Consensus of Fatty Liver Disease of the Brazilian Society of Pathology.28,29
Steatohepatitis was diagnosed histologically using three types of criteria: (a) broad criteria, in which the presence of steatosis associated with at least two of the following parameters is considered sufficient for diagnosis: lobular inflanmatory infiltrate (mononuclear and/or polymorphonuclear); any degree (including mild) of hepatocellular ballooning; or perisinusoidal/perivenular/ septal fibrosis (NASH 1). (b) restricted criteria, which involve the same parameters as described in (a); hepatocellular ballooning, however, must be of moderate to more marked intensity (NASH 2). (c) ultrarestricted criteria, which require that perisinusoidal and/or perivenular fibrosis be present, as well as steatosis, with or without the other parameters (NASH 3).
The final histological diagnosis of the study sample was made as follows: compatible with normal liver, without NAFLD; pure steatosis and steatohepatitis. The presence of pure steatosis or steatohepatitis defined the group of patients with nonalcoholic fatty-liver disease.
Statistical analysis. The quantitative variables are shown as the average and standard deviation. Qualitative or categorical variables are expressed as a number and percentage.
The Chi-square and Fisher exact tests were used to compare the categorical variables. The two-tailed t test was used to compare the continuous variables. The results of the analysis were considered significant for p < 0.05. The data were analyzed using the SPSS version 10.0 statistical package.
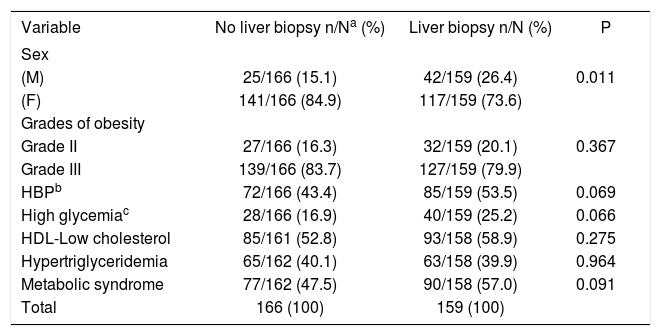
ResultsThree hundred and twenty-five patients were included in this study. The ratio of males to females was 1: 3.8; the average age was 36 ± 10 years; and the BMI was 43.7 ± 5.1 kg/m2. The histological study was carried out on 159 patients who agreed to be submitted to intraoperative liver wedge biopsy. Comparison of the patients who were submitted to liver biopsy and those who were not biopsied showed that the values of the majority of the parameters measured were similar in both groups. Males, however, predominated significantly in the group submitted to biopsy (p = 0.011) (Table I).
Comparative analysis between patients with BMI ≥ 35 kg/m2 submitted or not to liver biopsy.
| Variable | No liver biopsy n/Na (%) | Liver biopsy n/N (%) | P |
|---|---|---|---|
| Sex | |||
| (M) | 25/166 (15.1) | 42/159 (26.4) | 0.011 |
| (F) | 141/166 (84.9) | 117/159 (73.6) | |
| Grades of obesity | |||
| Grade II | 27/166 (16.3) | 32/159 (20.1) | 0.367 |
| Grade III | 139/166 (83.7) | 127/159 (79.9) | |
| HBPb | 72/166 (43.4) | 85/159 (53.5) | 0.069 |
| High glycemiac | 28/166 (16.9) | 40/159 (25.2) | 0.066 |
| HDL-Low cholesterol | 85/161 (52.8) | 93/158 (58.9) | 0.275 |
| Hypertriglyceridemia | 65/162 (40.1) | 63/158 (39.9) | 0.964 |
| Metabolic syndrome | 77/162 (47.5) | 90/158 (57.0) | 0.091 |
| Total | 166 (100) | 159 (100) |
Thirteen patients were excluded: biopsies unsuitable for histological analysis (n = 9), positive serology for HCV (n = 1), use of medication that causes steatohepatitis (n = 2) and other liver disease indicated by histology (n = 1).
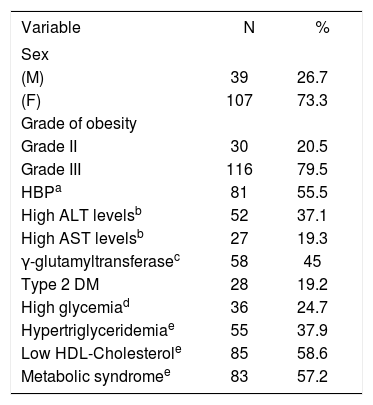
One hundred and forty six patients were available for the clinicohistological study. Eighty-one (55.5%) of the patients presented high blood pressure (HBP) and 28 (19.2%) presented Type 2 DM. Fifty-five (37.9%) presented hypertriglyceridemia and 85 (58.6%) presented HDL-cholesterol levels below the reference levels. Thirty-six (24.7%) presented high glycemic levels, i.e., glycemia > 110 mg/dL, or suffered from diabetes mellitus (Table II).
Descriptive analysis of the clinical characteristics of the 146 obese patients with BMI ≥ 35 kg/m2 in this study.
| Variable | N | % |
|---|---|---|
| Sex | ||
| (M) | 39 | 26.7 |
| (F) | 107 | 73.3 |
| Grade of obesity | ||
| Grade II | 30 | 20.5 |
| Grade III | 116 | 79.5 |
| HBPa | 81 | 55.5 |
| High ALT levelsb | 52 | 37.1 |
| High AST levelsb | 27 | 19.3 |
| γ-glutamyltransferasec | 58 | 45 |
| Type 2 DM | 28 | 19.2 |
| High glycemiad | 36 | 24.7 |
| Hypertriglyceridemiae | 55 | 37.9 |
| Low HDL-Cholesterole | 85 | 58.6 |
| Metabolic syndromee | 83 | 57.2 |
The lipid profile showed an average total cholesterol of 190.11 mg/dL (sd = 37.56 mg/dL). Average HDL-Chol and triglyceride levels were 45.35 mg/dL (sd = 8.6 mg/ dL) and 162.59 mg/dL (sd = 102.67 mg/dL), respectively. Measurement of glycemia showed an average fasting glycemia of 104.87 mg/dL (sd = 46.54 mg/dL).
Metabolic syndrome affected 57.2% of the severely obese patients and was even more prevalent in those with steatohepatitis, irrespective of the diagnostic histological criteria used.
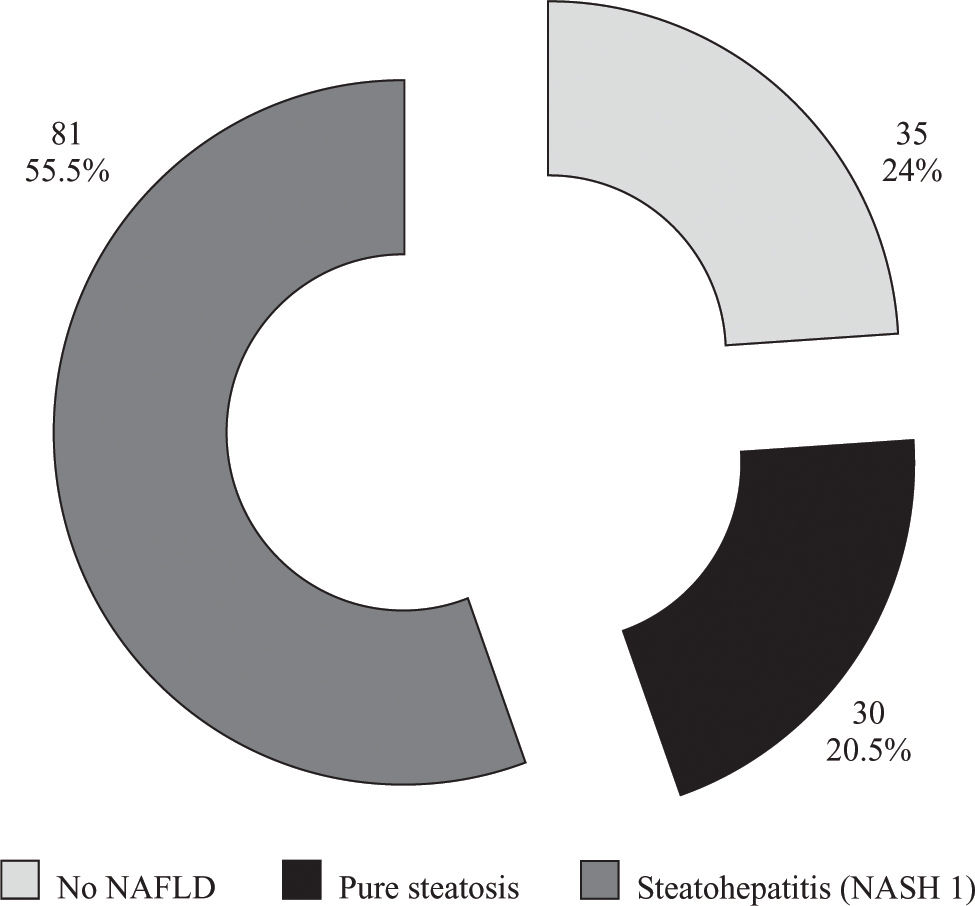
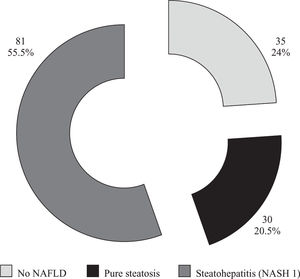
According to our histological analysis, the prevalence of nonalcoholic fatty-liver disease (NAFLD) in the sample of 146 patients was 76% (111 patients). Pure steatosis was only present in 30 patients (20.5%), and thirty five patients (24%) were considered not to have NAFLD (Figure 1).
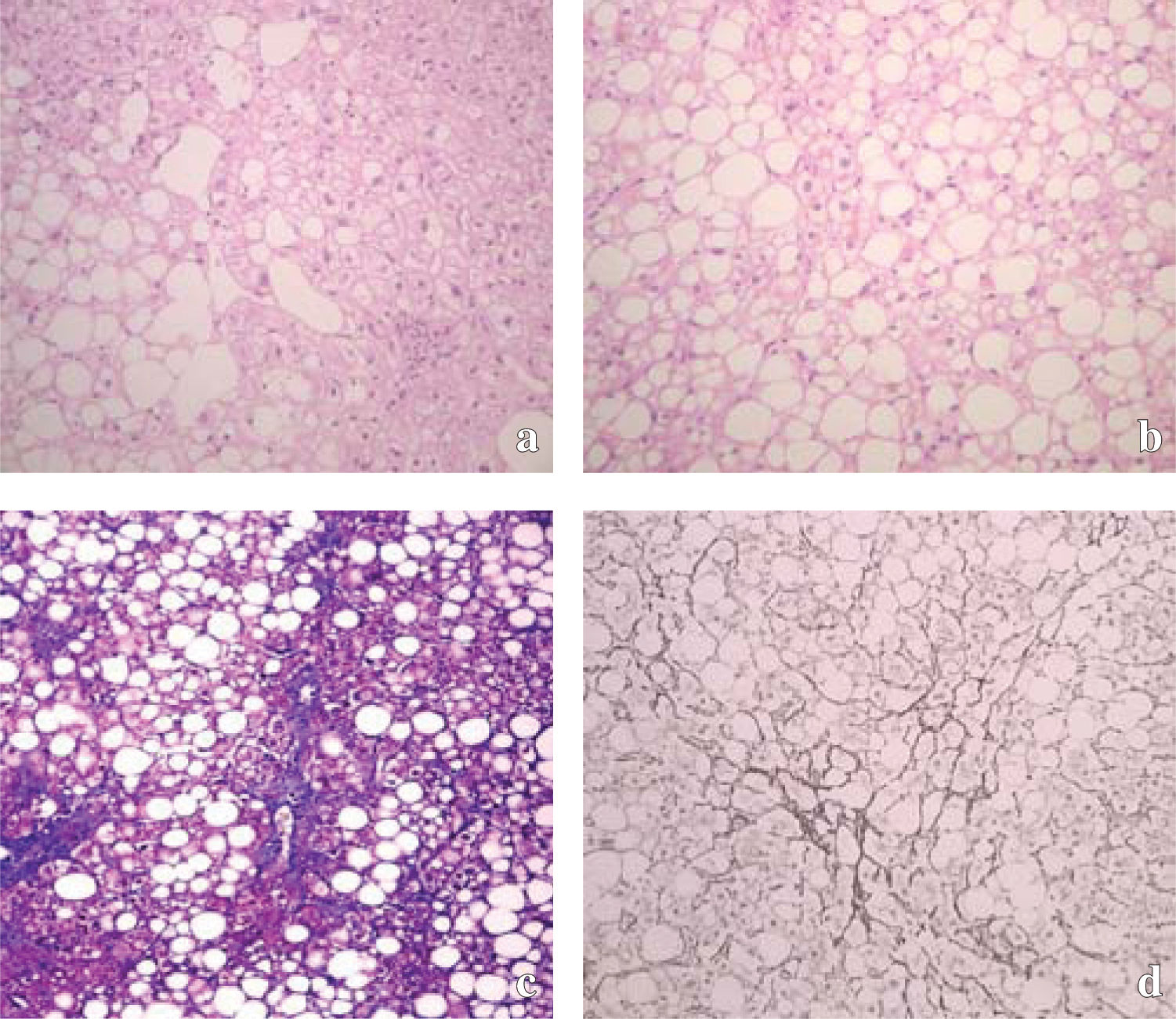
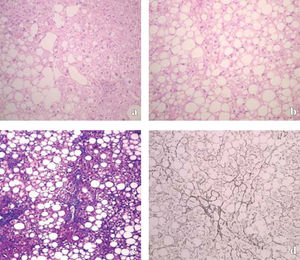
When broader histological criteria were used (including even patients with mild hepatocellular ballooning associated with steatosis and mild inflammatory activity with or without fibrosis), NASH was diagnosed in 81 patients (55.5%) from the sample (NASH 1 - Figure 2a). With more restricted criteria, so that only those patients who presented at least moderate hepatocellular ballooning were included, 60 (41.1%) of the patients were diagnosed with steatohepatitis (NASH 2 - Figure 2b). However, when ultrarestricted criteria were used, so that patients were only considered to suffer from steatohepatitis if, as well as steatosis, they presented perisinusoidal and/or perivenular fibrosis (with or without the presence of other necroinflammatory findings), the prevalence of this diagnosis fell to 25.3% (37 of the severely obese individuals) (NASH 3 - Figures 2cand2d).
Histopatological presentation of NASH. a: Macrovesicular steatosis grade 2, ballooned hepatocytes grade 1 and a moderate mononuclear infiltrate. NASH 1 (Hematoxylin and eosin stain of liver, magnification × 100). b: Necrotic inflammation in the NASH 2 group, with more marked ballooned hepatocytes and a mild mononuclear infiltrate, without fibrosis. (Hematoxylin and eosin stain of liver, magnification × 100). c: Histologic features of fibrosis in nonalcoholic steatohepatitis (NASH 3 group), demonstrating macrovesicular steatosis and fibrosis, most prominent in zone 3 near the central vein of the hepatic lobule. (Trichrome stain of liver, magnification × 100). d: Typically early fibrosis is pericellular and perisinusoidal, giving the appearance of «chickenwire.», also NASH 3 (Reticulin stain of liver, magnification × 100).
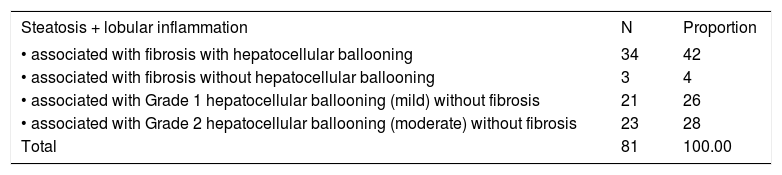
Table III summarizes the association of the different histological components used to diagnose steatohepatitis. Fibrosis was present in 37 (45.7%) of the 81 patients; a perisinusoidal distribution was the most frequent and occurred in 34 (42%) of the 81 patients. Distortion of the parenchymal architecture of the liver occurred in only 1 (1.2%) of the patients, and none of them presented a histological picture compatible with cirrhosis.
Distribution of the different histopathological parameters among 81 patients with nonalcoholic steatohepatitis.
| Steatosis + lobular inflammation | N | Proportion |
|---|---|---|
| • associated with fibrosis with hepatocellular ballooning | 34 | 42 |
| • associated with fibrosis without hepatocellular ballooning | 3 | 4 |
| • associated with Grade 1 hepatocellular ballooning (mild) without fibrosis | 21 | 26 |
| • associated with Grade 2 hepatocellular ballooning (moderate) without fibrosis | 23 | 28 |
| Total | 81 | 100.00 |
Considering the whole population of 325 patients submitted to bariatric surgery only half of them, in whom a liver biopsy was allowed, could be evaluated in terms of the prevalence of NAFLD and NASH. This main limitation raises the question of how representative of the whole population is the studied sample. In order to evaluate this fundamental aspect of our study, a comparative analysis between included and excluded patients was performed. The parameters related to possible risk factors of NAFLD and NASH as degree of obesity, arterial hypertension, glycemia alterations, levels of tryglicerides and HDL cholesterol as well as the metabolic syndrome itself27 were similar between the two groups, assuring that our sample is representative of the whole population studied. A difference was found in sex distribution, namely more men accepted to be submitted to liver biopsy. A clear reason for this difference could not be determined but we could hypothesize that men are more prone to take risks.
Obesity is a well known factor that favors the insulin resistance, which is a common ethiopathogenic element for diseases as diabetes and systemic arterial hypertension.30 Confirming other studies31-34 we also found high prevalences of systemic arterial hypertension, dyslipidemia and hyperglycemia.
The metabolic syndrome itself was also very prevalent (57.2%), corresponding to the double of the estimated prevalence of the Hispano-American in USA in a similar age group.35 For patients with NASH and fibrosis the prevalence of metabolic syndrome raised from 57.2 to 75.7%. This is not very different from the data of another study, with a large series that evaluated prevalences of metabolic syndrome, according to ATP III definition.31These data support the role of insulin resistance in the physiopathology of NASH.36,37 The epidemiological association between metabolic syndrome and NASH is extremely important, due to the epidemy of obesity all around the world.1,38
The aim of this study was to determine the prevalence of NAFLD and NASH in severely obese patients. When a histological assessment was made, 76% of the obese patients with BMI > 35 kg/m2 were found to present NAFLD. The prevalence of steatohepatitis, however, varied according to the histological definition adopted. In the broadest definition, steatohepatitis was found in 55.5%. Using more restricted criteria based on more pronounced liver damage, the prevalence of steatohepatitis dropped to 41.1%. When ultrarestricted criteria were used, i.e., including only patients with fibrosis, the prevalence fall to 25.3%.
There is a great number of other studies into the prevalence of NAFLD and NASH5,14,22,32,33,39 but the range of different criteria used in both the selection of patients and the diagnosis of NAFLD and NASH leads to diverging results.34 A population study carried out recently in the northeast of Italy, in which steatosis was diagnosed using ultrasonography, showed that NAFLD was present in 76% of the obese population.32 However, in another study carried out in Brazil using ultrasonography for diagnosis, the prevalence of steatosis in obese women was 33.5%.40
Other studies into the prevalence of steatosis in different populations have produced results ranging from 1% to 51%,18,34 and the majority of the available data have come from retrospective studies using selected population groups and different methodologies, making it difficult to compare and analyze the results of these studies.
When studies using histological assessment were analyzed, the diagnosis of steatohepatitis was also found to vary from 2.7% and 18.5% in lean and obese patients, respectively,5 to 32% in patients with altered transaminase levels.41
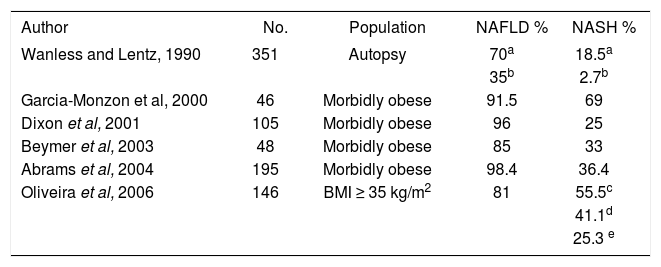
The histological diagnosis of steatohepatitis continues to be controversial, and various experts diverge as to the criteria needed for diagnosis of this disease.42 Thus, the prevalence of steatohepatitis may also be influenced by the different criteria used to characterize the disease, as shown in Table IV. In a study of 46 severely obese patients referred for bariatric surgery, steatohepatitis, defined as the presence of steatosis associated with lobular inflammation, was found in 69% of the patients, and this histological characterization for steatohepatitis, explains this higher prevalence findings.43 When Dixon et al.14 analyzed patients referred for bariatric surgery, they observed a prevalence of 96% for NAFLD and 25% for NASH. Patient’s selection criteria were similar to the ultra strict diagnostic criteria used in this study and required the presence of steatosis associated with perisinusoidal/pericellular fibrosis.
Prevalence of fatty liver disease and nonalcoholic steatohepatitis in obese patients.
| Author | No. | Population | NAFLD % | NASH % |
|---|---|---|---|---|
| Wanless and Lentz, 1990 | 351 | Autopsy | 70a | 18.5a |
| 35b | 2.7b | |||
| Garcia-Monzon et al, 2000 | 46 | Morbidly obese | 91.5 | 69 |
| Dixon et al, 2001 | 105 | Morbidly obese | 96 | 25 |
| Beymer et al, 2003 | 48 | Morbidly obese | 85 | 33 |
| Abrams et al, 2004 | 195 | Morbidly obese | 98.4 | 36.4 |
| Oliveira et al, 2006 | 146 | BMI ≥ 35 kg/m2 | 81 | 55.5c |
| 41.1d | ||||
| 25.3 e |
Other authors who studied severely obese patients more recently and used selection criteria similar to the broad and strict criteria used in this study found NASH prevalence to vary between 33% and 36.4%.44,45 As both histological and epidemiological knowledge increases with time, a more comprehensive diagnosis of NASH will thus become possible.17,18,21,42
The use of a scaled histological assessment was based on the need to treat each criteria used in the diagnosis of NASH individually to enable earlier histological diagnosis of this disorder. Confirming the need for a scaled diagnosis, Kleiner et al. (2005)46 recently published a classification of NAFLD aimed at establishing the following diagnoses of NASH: possible NASH, NASH and non NASH. This was achieved by creating a nonalcoholic-fatty-liver-disease («NAS») activity score.
In our sample, hepatocellular ballooning was the main injury responsible for the difference between pure steatosis and steatohepatitis. It was found in either a mild or moderate form in 97.3% of the patients with NASH. In a study of the prognosis of NAFLD, Matteoni et al. (1999)8 had already demonstrated the importance of hepatocellular ballooning in detecting steatohepatitis and its potential for worsening the evolution of the disorder.
Of the severely obese patients assessed in our study, only one presented distortion of the lobular architecture of the liver compatible with a more advanced disease. This result is different from those of other series, where the prevalence of more advanced fibrosis was around 12%44 and the prevalence of cirrhosis, 4%.14 This divergence can be explained by the fact that the average age of the patients in our study (36 years) was lower than that of patients in other studies (from 42 to 47 years). The presence of fibrosis suggests a more advanced disease and more aggressive liver damage, which require time to become established. Progression of liver damage in NASH may lead to portal fibrosis, the formation of septa and occasionally cirrhosis.21-42-47-48
The absence of universally accepted criteria for the histological diagnosis of steatohepatitis allows a number of studies about steatohepatitis to define it as the association of steatosis with any type of liver inflammation.18-21 Such a definition, however, is insufficiently specific and can result in individuals with nonspecific reactive changes being included in the pool of patients with NASH. In this study, a 40% increase in the diagnosis of steatohepatitis was observed when more flexible criteria were used. The use of very strict criteria requiring the presence of pericellular/perisinusoidal fibrosis,49 however, while increasing the specificity of the diagnosis, fails to detect those patients with less severe histological changes. This would result in over half the diagnoses of steatohepatitis being missed, and as shown by Caldwell et al. (1999),50 these cases could evolve into more severe forms of the disease.
In conclusion, the results presented here for severely obese patients reflect the varying prevalences of NASH among this population depending on the histological parameters used to define the disease. The lack of agreement regarding the histological diagnosis of NASH makes it difficult to determine the true prevalence of this disease. There is therefore a pressing need to define protocols for clinicohistological assessment to allow a prognosis to be made and more aggressive treatment strategies for this disorder to be drawn up.