Portal hypertension surgery has evolved widely in the last decades. Since the first surgical shunt was done in 1945 for the treatment of recurrent hemorrhage, many surgical options have been developed including selective shunts, low diameter shunts and extensive devascularization procedures. Many of them have been studied and compared showing their advantages and disadvantages, evolving also their role in the therapeutic armamentarium.
Surgery is nowadays a second line treatment option (after β blockers and endoscopic therapy), and it’s main indication is for patients whose main and only problem is history of bleeding, with good liver function (Child-Pugh A). For emergency situations it has a very limited role and for primary prophylaxis virtually has also no role. Patients with good liver function, electively operated with portal blood flow preserving procedures are the patients that benefit from surgical treatment. Patients with a bad liver function are better candidates for a liver transplant.
The treatment of hemorrhagic portal hypertension has evolved widely in the last decades. Several options have appeared as alternate therapeutic choices, each one with advantages and disadvantages. Their usage depend widely on the individual characteristics of each patient, the cause of portal hypertension, liver function, hospital infrastructure and developed programs as well as the experience of the multidisciplinary team.
Nowadays there are therapeutic options to prevent the first hemorrhage (primary profilaxis), treatment in the acute phase of bleeding and options to preventre bleeding (secondary prophylaxis).
Pharmacological Therapy.1,2,3 This therapeutic choice can be used either for acute bleeding or for primary and secondary prophylaxis. Their mechanism of action is by reducing cardiac output as well as producing vasodilatation of the splachnic vessels and sinusoids in the liver. For the acute bleeding episode, vasopresin can be used with nitroglycerin. Although a good response can be obtained, recurrence of hemorrhage is high when it is interrupted. Glypresin has a long acting effect and somatostatin, that has also a vasoconstrictor effect, has a short availability.
Octreotide has the same effect with longer duration. Betablockers have been used widely, for primary and secondary prophylaxis, although they have a high recurrence rate of rebleeding (between 30 and 50%).
Several prospective, controlled, randomized trials have shown their effectioness when compared with other options for primary prophylaxis. Also combined with other vasodilatation and/o endoscopic therapy, they have shown promissory results for primary prophylaxis and good results for secondary prophylaxis.
Endoscopic treatment.4,5,6,7 Transendoscopic sclerotherapy has been proved for several decades for the treatment of both acute bleeding and primary-secondary prophylaxis. This type of therapy has been used mainly for secondary prophylaxis nevertheless; they have a high rebleeding rate (between 30 and 50%). Transendoscopic banding of varices has emerged in the last two decades as a better option, because the same results can be expected with a lower complication rate.
Transjugular intrahepatic portosystemia shunts (TIPS)8,9,10,11 have been widely used in developed counties. High infrastructure of the hospital is needed as well as technical expertise. They are expensive. The success of placement is high (95%) and several contraindications for their usage has been identified. (Cardiac failure, polycistic disease, deep liver failure). Mortality after placement (0-30 days) range between 10 and 15% and a high frequency of encephalopathy is observed when the shunt is patent. After 6 months a high obstruction rate is observed (up to 50%) that needs another intervention, either to place a new one or dilate the obstructed stent. Recently, a stent has been developed with an internal antithrombotic coverage that could prevent obstruction. Their usage is reserved for patients with bleeding and/or ascitis that are in the waiting list for liver transplantation.
Surgical treatment has envolved widely and a large variety of options (shunt and ablative procedures) have been described.12,13
Shunts can be total (total deviation of portal blood flow to the systemic circulation) partial (partial deviation of portal flow through the placement of a narrow prothesis either in portocaval or mesocaval position) and selective (distal splenorenal, coronariocaval, splenocaval). Selective shunts, described in 1967, have the main advantage that in most patients, maintain portal blood flow because two compartments are created. The esophagogastro splenic area is derived through the anastomosis to the systemic circulation and the mesoportal system is maintained with hypertension. Selective shunts have good results all over the world, when interested teams perform them. In general, a low rebleeding rate is achieved (less than 5%), low encephalopathy rate (less than 10-15%) and a good quality of life in the postoperative period. No other option offers such good short-medium term results.
Encephalopathy has an increased incidence in the late postoperative period (between the 7 and 10 postoperative year). It is the consequence of the transformation of the selective into a total shunt and is the result of an increased resistance at the hepatic sinusoid.
This increased resistance is consequence of progression of liver disease that increased sinusoidal resistance and increases mesoportal pressure. Collaterals to the low pressure area are developed and loss of portal perfusion occurs. Because they leave the hepatic hilus intact, they are a good option for liver transplant candidates and are excellent long term bridge for liver transplantation.
Ablative procedures (devascularizations)14 are been used an alternate choice for patients in which a shunt cannot be done. Some groups, mainly in Japan, used them as a first therapeutic choice, because they have a lower incidence of encephalopathy.
They have a higher rebleeding rate than surgical shunts and this seems to be related to the extension of the devascularization. The extensive the devascularization, the lower is the recurrence rate. Several technique have been described, through the thorax, abdomen or both.
Devascularization is done including afferent and efferent vascular elements as well as esophageal transection. Splenectomy is also done. The Sugiura Futagawa operation (SFO) and its variants (Hassab, Paquet) are the most widely used. The SFO is a two stage operation. In the abdominal stage, the devascularization is done from the incisura angularis up to the cardias and lower esophagus of both minor and large curvature. Splenectomy is also done at this stage. Some authors have included the performance of a transection of the esophagus using an end to end stepler anastomosis device.
In the thoracic stage, the devascularization is done to the level of the aortic arch through a left throacotomy. Complete desvascularization is done and a transection of the esophagus in order to interrupt the esophaged submucosal varices is added.
Complete portoacygos disconnection is an operation designed on the basis of the Sugiura-Futagawa procedure, but with variants that make the procedure easier and safer. In the abdominal stage, the spleen is preserved. Spleen is removed only if a large splenomegaly is found (as in prehepatic portal hypertension), and/or severe hypersplenism (count platelet below 20 x 103/dl).
Truncal vagotomy is done also, because around them newer varicose veins are developed that connect with the azygos system and also the lesser curvature is completely ligated, interrupting the main branches of the left and right gastric veins.
In order to achieve complete portoacygos disconnection the thoracic devascularization is done. Important step is the interruption of the afferent arterial branches that reach the developed varices. The transection is also modified, placing a running suture around the mucosa and submucosa without opening it. This modification has a very low complication rate, without fishilization. In the SFP there frequency of fistulization is 8% with a 50% mortality. With the modified transection virtually no fistulization is observed.
The two procedures, have good results with a low rebleeding rate (10 – 15%) and low encephalopaty rate (2 – 4%) and good long term survival.
Surgery should not be used for primary prophylaxis,15 Although some groups in Japan have shown good results it is generally accepted that it has no place because, although low, has operative mortality and can also induce other complications.
For the acute bleeding episode, it is also generally accepted that better results can be obtained with pharmacotherapy and endoscopic therapy. So, surgical treatment is rarely indicated.
M. Orloff has gained a large experience with portocaval shunts in the acute situation. This results have not been reproduced but also have not been refuted.16
Extreme cases with remarkable good liver function that are refractory to other options (including second line treatment choices an TIPS) could be considered for surgical treatment.
For secondary prophylaxis surgical treatment offers an excellent choice for patients with good liver function. Child-Pugh A and B1 cases can be considered for surgical treatment. In many centers only cases that fail to endoscopic therapy are treated by means of surgery. It is reasonable to consider surgery as first line treatment for low risk, Child-Pugh A patients, because the other options, as has been stated above, have a high rebleeding rate.
It has to be analyzed very carefully that type and prognosis of the underlying, liver disease. So, for example a patient with sclerosis cholangitis that develops portal hypertension is not a good case for surgical treatment. Also patients with bad liver function (B- or C) (Child - Pugh patients) are not good candidates for surgery. In these cases, a liver transplant is a better choice.17
Our group conducted a prospective, controlled, randomized trial comparing farmacotherapy, sclerotherapy and portal blood flow preserving procedures in low risk patients. It was shown a significant lower recurrence rate for the surgical group, but although better, no significant difference in survival was shown. It must be stated that failure from the farmacotherapy and sclerotherapy groups were rescued by means of surgery.18
In the last five year our group has achieved excellent results in low risk patients with portal blood flow preserving procedures.
A low mortality has been reached (less than 2%), with a good as long term survival and very low rebleeding recurrence. We are convinced that. Low risk patients should be surgically treated as their first option.
Liver transplantation (the ultimate shunt) is an important part of the surgical armamentarium. It is mainly indicated for patients with a bad liver function.19,20,21
Many patients receive one or several therapeutic choices in the course of their disease. Some patients start with farmacotherapy and endoscopic therapy, receive a TIPS or surgical treatment and later a liver transplant.
There is no doubt that portal hypertension needs a multidisciplinary approach. Patients should be refereed to interested and well equipped hospitals. Each patient has to the carefully evaluated in order to select his or he best therapeutic option.
Experience with surgical treatment at the Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”.Only four years after the first portocaval shunt was done by Whipple in 1945 for the treatment of hemorrhagic portal hypertension, a proximal splenorenal shunt was done at our hospital by Robles and Muñoz Kapellmann.
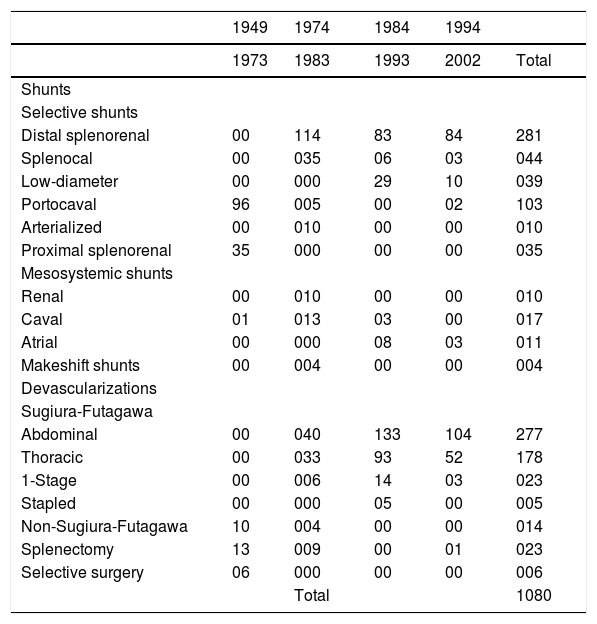
In the first decade (Table I) several total shunts were done, mainly portocaval shunts, which confirmed the findings of others groups in the world that were effective procedures to treat the recurrence of bleeding but that total deprivation of portal blood flow was deleterious to the liver function. Nevertheless, they were an important tool at that time for the treatment of bleeding because no other therapies were available. In 1973, a clinic founded by Hector Orozco MD, devoted to the study and treatment of patients with portal hypertension, started the protocolization of treatment. Many surgical procedures were maintained in the surgical armamentarium. Nowadays, only extensive devascularizations and selective shunts, as well as low diameter shunts were done.
| 1949 | 1974 | 1984 | 1994 | ||
|---|---|---|---|---|---|
| 1973 | 1983 | 1993 | 2002 | Total | |
| Shunts | |||||
| Selective shunts | |||||
| Distal splenorenal | 00 | 114 | 83 | 84 | 281 |
| Splenocal | 00 | 035 | 06 | 03 | 044 |
| Low-diameter | 00 | 000 | 29 | 10 | 039 |
| Portocaval | 96 | 005 | 00 | 02 | 103 |
| Arterialized | 00 | 010 | 00 | 00 | 010 |
| Proximal splenorenal | 35 | 000 | 00 | 00 | 035 |
| Mesosystemic shunts | |||||
| Renal | 00 | 010 | 00 | 00 | 010 |
| Caval | 01 | 013 | 03 | 00 | 017 |
| Atrial | 00 | 000 | 08 | 03 | 011 |
| Makeshift shunts | 00 | 004 | 00 | 00 | 004 |
| Devascularizations | |||||
| Sugiura-Futagawa | |||||
| Abdominal | 00 | 040 | 133 | 104 | 277 |
| Thoracic | 00 | 033 | 93 | 52 | 178 |
| 1-Stage | 00 | 006 | 14 | 03 | 023 |
| Stapled | 00 | 000 | 05 | 00 | 005 |
| Non-Sugiura-Futagawa | 10 | 004 | 00 | 00 | 014 |
| Splenectomy | 13 | 009 | 00 | 01 | 023 |
| Selective surgery | 06 | 000 | 00 | 00 | 006 |
| Total | 1080 |
It should be stated that in our group, better results have been obtained with portal blood flow preserving procedures, with better long term results.
Also, it has to be remarked that in the last years a very low operative mortality (less than 2%) has been achieved, offering excellent results in low risk patients.