Background and aim. Hepatocellular carcinoma (HCC) is a frequent cancer. Its prognosis is highly dependent on early diagnosis. Patients at risk for developing HCC should be enrolled in a surveillance programme. Nevertheless, many patients at risk are not regularly screened. We aimed at exploring the characteristics that affect enrolment in a surveillance programme.
Material and methods. The characteristics of the patients included in the prospective Bern HCC cohort between August 2010 and August 2011 were analysed according to their participation in a surveillance programme.
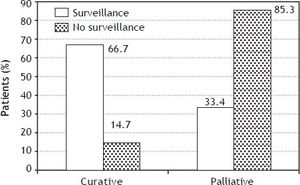
Results. Among the 82 patients included in the cohort during this period of time, 48 were in a surveillance program before the diagnosis of HCC. Thirty five percent of cirrhotic patients were not screened. Age, sex, level of education, Child-Pugh status and MELD score were similar between the patients who were screened and those who were not screened. Patients with a private insurance and patients treated by a liver specialist were more frequently enrolled in a surveillance program. Sixty seven percent of the screened patients were eligible for curative treatment whereas only 15% of the non-screened patients were.
Conclusions. In conclusion the surveillance of patients at risk for developing HCC increases their chances to be diagnosed at an early stage to allow curative treatment. More than one third of cirrhotic patients were not regularly screened. Patients with chronic liver disease should be referred to identify those at risk and enrol them in a surveillance program.
Hepatocellular carcinoma (HCC) ranks fifth worldwide in terms of cancer incidence and third in terms of cancer-related mortality.1 The management of patients with HCC is based on the assessment of 3 parameters: tumor burden, liver function and patient performance status. This assessment forms the basis of the Barcelona Clinic Liver Cancer (BCLC) algorithm, which is the most widely used.2 Patients with tumor less than 2 cm are eligible for radiofrequency ablation or surgical resection. Patients with 1 tumor less than 5 cm or up to 3 tumors each less than 3 cm are eligible for transplantation. Patients with larger tumors are not candidates for curative approaches; they are treated with trans-arterial chemoembolization, selective internal radiotherapy and/or systemic targeted therapy. Patients with a Child-Pugh C stage who are not eligible for transplantation receive best supportive care. If the median survival in case of curative approach is more than 5 years, it is less than 2 in case of palliative approach.3
Numerous guidelines recommend screening for hepatocellular carcinoma.3–6 The population at risk is well-defined, the screening test which is sonography, is well accepted and widely available and its interval of application has been set to 6 month.7 There is only one randomized controlled trial showing a benefit for HCC screening.8 However, it was criticized for not controlling for cirrhosis, for suboptimal adherence and for incorrect statistical analysis. Nevertheless numerous cost-analysis studies have shown that enrolment in a surveillance program reduces HCC mortality.9–14 It is assumed that this benefit is due to diagnosing patients at an earlier stage.
Despite these considerations, it is still unknown what proportion of patients diagnosed with HCC is included in a surveillance program and what are the barriers to screening. The aim of this work was to investigate the parameters that could influence inclusion in a surveillance program for HCC using data from the Bern HCC cohort, which prospectively collects standardized information on patients affected by HCC.
Material and MethodsDesign of the studyThe HCC cohort started in the 1st of August 2010 at the University Hospital of Berne, one of the largest referral hospitals in Switzerland. It is a multidisciplinary prospective study including hepatologists, radiologists, oncologists and visceral surgeons. All the adult patients with diagnosed HCC in the last 18 months were invited to participate. The diagnosis of HCC was based on the American Association for the Study of Liver Diseases (AASLD) practice guidelines criteria.15 The protocol was approved by the Bern ethics committee and each participant has to sign an informed consent. This manuscript evaluates the characteristics of the patients included during a period of 12 months.
Data collection and processingAt inclusion patients were evaluated for the following variables: demographic information (age, sex, race), date of initial diagnosis of HCC, methods of diagnosis (CT, MRI, histology), context leading to the diagnosis of HCC (finding in a surveillance program, new symptoms, laboratory results, incidental radiological finding), risk factors for HCC and comorbidities (cirrhosis, smoking, alcohol consumption, diabetes, elevated BMI), tumor burden, Child-Pugh stage and its variables (albumin, bilirubin, prothrombin time, ascites, encephalopathy), Barcelona Clinic Liver Cancer (BCLC) classification, Model of End-Stage Liver Disease (MELD) score, α-fetoprotein (AFP) level, socio-economic parameters (achieved education, professional occupation, type of health insurance). The diagnosis of cirrhosis was based on histology and/or indirect clinical signs such as the presence of varices or ascites. With regard to the cause of liver disease multiple etiologies were possible. Anti-HBc denoted exposure to hepatitis B virus. Positive viremia was required for classification as hepatitis C virus. Alcohol was retained in individuals who drank more than 60 g of alcohol a day. Non-alcoholic steatohepatitis was considered in individuals with metabolic syndrome and/or a liver histology with the features of steatohepatitis in a patients drinking less than 30 g of alcohol/day. Patients were considered in a sur-veillance program if they had 2 liver sonographies at 6 month interval in the 12 months preceding the diagnosis of HCC.
Statistical methodsContinuous data are expressed as the mean ± SD. Fisher’s exact test for comparison of categorical outcomes and Wilcoxon’s test for comparison of continuous outcomes were used to compare screening and the non-screening groups. Characteristics associated with HCC screening at p ≤ 0.20 in univariable analysis were included in a multivariable exact logistic regression model. Analyses were performed with Stata IC 11.0 (StataCorp, College Station, TX).
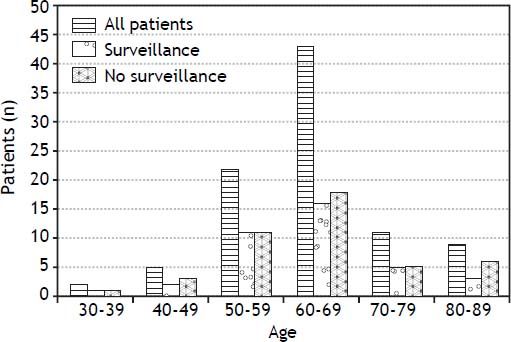
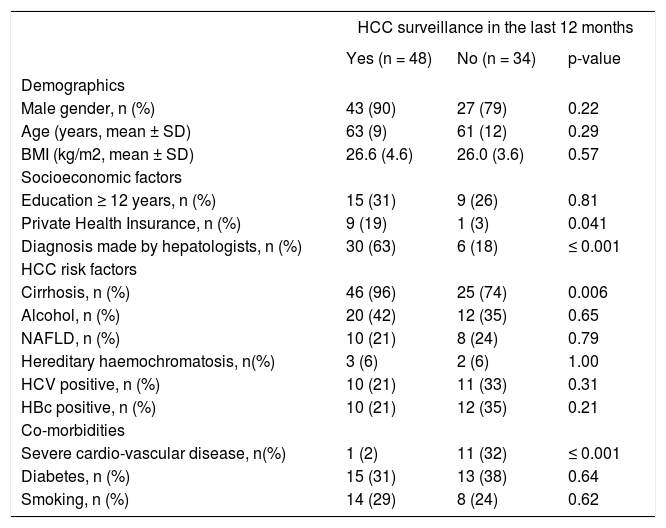
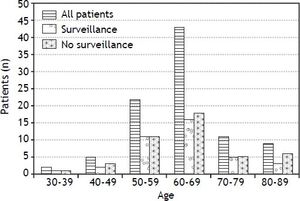
ResultsFrom the 1st of August 2010 to the 1st of August 2011, 82 patients were enrolled, no patient declined to participate. Table 1 shows the characteristics of these 82 patients. The majority were men (70/82, 85%). The majority of male patients were included in a surveillance program (43/70, 61%), whereas the majority of the female patients were not (7/12, 58%). The mean age was 62 years. Figure 1 shows the age distribution in both, the screened and non-screened group. The age group 60-69 years was the most frequent. Patients older than 80 years old continued to be screened. The mean value of the BMI was 26.4. Thirty-seven percent of all patients had a normal weight (BMI 18.5-25) whereas 49% were slightly overweight (BMI 25-30). There was no difference in BMI between the patients who were screened and those who were not screened.
Characteristics of patients by HCC surveillance.
| HCC surveillance in the last 12 months | |||
|---|---|---|---|
| Yes (n = 48) | No (n = 34) | p-value | |
| Demographics | |||
| Male gender, n (%) | 43 (90) | 27 (79) | 0.22 |
| Age (years, mean ± SD) | 63 (9) | 61 (12) | 0.29 |
| BMI (kg/m2, mean ± SD) | 26.6 (4.6) | 26.0 (3.6) | 0.57 |
| Socioeconomic factors | |||
| Education ≥ 12 years, n (%) | 15 (31) | 9 (26) | 0.81 |
| Private Health Insurance, n (%) | 9 (19) | 1 (3) | 0.041 |
| Diagnosis made by hepatologists, n (%) | 30 (63) | 6 (18) | ≤ 0.001 |
| HCC risk factors | |||
| Cirrhosis, n (%) | 46 (96) | 25 (74) | 0.006 |
| Alcohol, n (%) | 20 (42) | 12 (35) | 0.65 |
| NAFLD, n (%) | 10 (21) | 8 (24) | 0.79 |
| Hereditary haemochromatosis, n(%) | 3 (6) | 2 (6) | 1.00 |
| HCV positive, n (%) | 10 (21) | 11 (33) | 0.31 |
| HBc positive, n (%) | 10 (21) | 12 (35) | 0.21 |
| Co-morbidities | |||
| Severe cardio-vascular disease, n(%) | 1 (2) | 11 (32) | ≤ 0.001 |
| Diabetes, n (%) | 15 (31) | 13 (38) | 0.64 |
| Smoking, n (%) | 14 (29) | 8 (24) | 0.62 |
Wilcoxon test for comparison of continuous outcomes. Fisher’s exact test for comparison of categorical outcomes.
Fifty-one percent of patients were retired, 24% were employees, 14% were independents and 11% were on social support. When examining whether the level of education affected the enrollment in a surveillance program, we found similar proportions of patients with at least 12 years of education in those with and without HCC surveillance. There was a significant relationship between the type of health insurance and the likelihood of being in a surveillance program, however. Seventy-two patients had a general health insurance (88%) and only 10 had a private health insurance (12%). Nine out of the 10 patients (90%) with private insurance were screened, but only 39 of those with a general health insurance (54%, p = 0.04). Inclusion in a surveillance program was significantly more frequent for patients who were followed by a liver specialist. Thirty out of the 36 patients treated by a liver specialist and diagnosed with HCC were screened (83%), but only 18 patients out of the 46 patients not followed by a liver specialist (39%, p < 0.001).
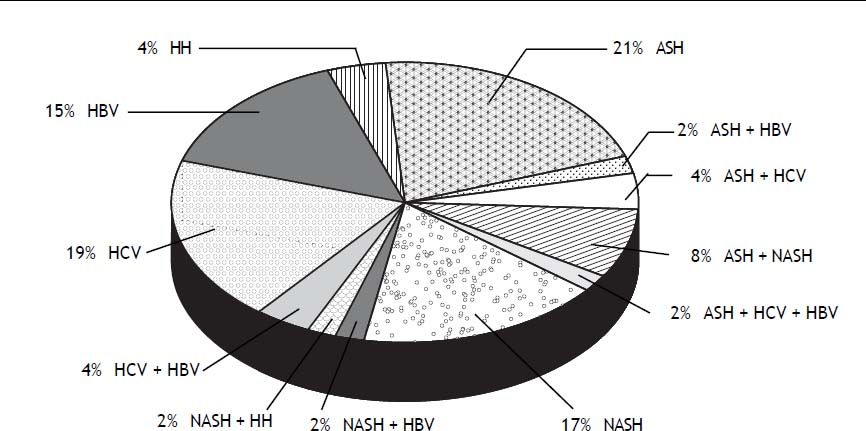
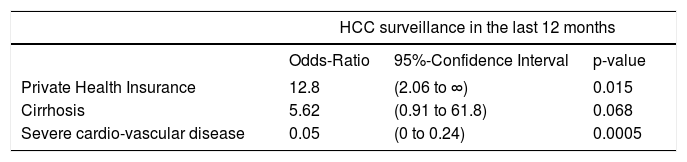
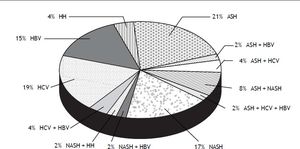
Eighty seven percent of the patients had cirrhosis (71/82). Two patients without cirrhosis but with advanced fibrosis were subjected to screening. Alcohol was the most frequent cause of liver disease (32 patients) followed by hepatitis B (22 patients) and hepatitis C (21 patients). Eighteen patients had a non-alcoholic fatty liver disease (NAFLD). Thirty four percent of the patients had a diabetes mellitus and 27% were smokers. As shown in figure 2 nearly a quarter of the patients (24%) cumulated more than one cause for their underlying liver disease. All combinations were present; 4% had a co-infection with hepatitis C and B, 4% had a combination of alcohol and HCV infection and 2% a combination of alcohol and HBV infection. Two percent had even three different causes for their underlying liver disease including alcohol, HCV and HBV. Regarding participation in a surveillance program, the presence of cirrhosis was significantly associated with regular screening (p = 0.006): 65% of the screened patients had cirrhosis, whereas 35% of the non-screened patients had liver cirrhosis. Neither the etiology of the liver disease, nor the presence of diabetes and smoking was associated with surveillance. Patients with advanced cardiovascular disease were significantly less likely to undergo surveillance (p = 0.002). Table 2 presents results from a multivariable model including the three patient characteristics that were associated with HCC surveillance in univariable analysis at p ≤ 0.20. Patients with private health insurance remained more likely to have had HCC surveillance (odds ratio 12.8, p = 0.015), whereas patients with severe cardiovascular disease were significantly less likely (odds ratio 0.05, p = 0.0005). For patients with cirrhosis there was a statistical trend towards more frequent HCC surveilance (odds ratio 5.62, p = 0.068).
Association of patient characteristics with HCC surveillance in multivariable model.
| HCC surveillance in the last 12 months | |||
|---|---|---|---|
| Odds-Ratio | 95%-Confidence Interval | p-value | |
| Private Health Insurance | 12.8 | (2.06 to ∞) | 0.015 |
| Cirrhosis | 5.62 | (0.91 to 61.8) | 0.068 |
| Severe cardio-vascular disease | 0.05 | (0 to 0.24) | 0.0005 |
Odds-ratio from multivariable exact logistic regression. A variable was included in the multivariable model if its p-value was < 0.2 in univariable analysis. Type of physician who made the diagnosis (hepatologist or other) not included in multivariable model, since this was not a patient characteristic.
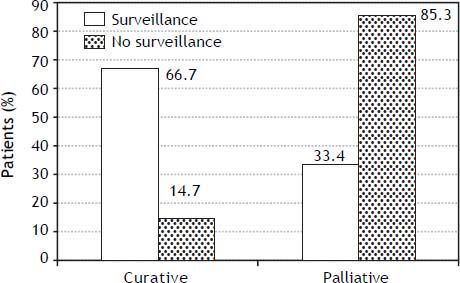
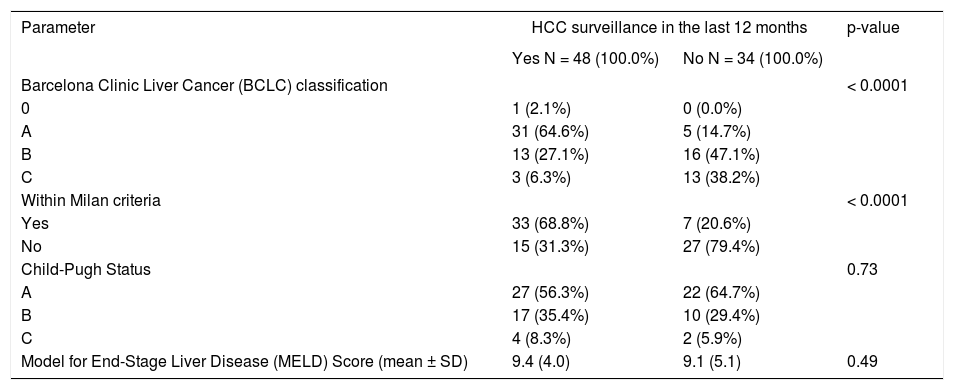
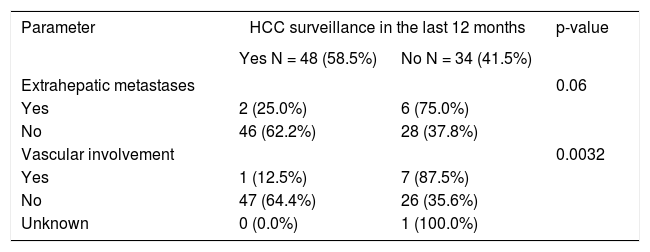
Tumor staging at the time of diagnosis is described in table 3. Patients who were not in a surveillance program had significantly more advanced tumors as assessed by the BCLC classification (p < 0.0001). The majority of the patients who were screened were in a BCLC class A and therefore were eligible for curative treatments (65%), whereas the majority of the non-screened patients were in a BCLC group B and therefore were confined to palliative therapies (47%). Patients, who were in a surveillance program were more likely to have a tumor within the Milan criteria than those who were not in a surveillance program (69 vs. 21%, p < 0.0001). These 2 groups of patients were neither dif-ferent based on their Child-Pugh score (p = 0.73) nor on their MELD score (p = 0.49). Table 4 shows that inclusion in a surveillance program was associated with less macro-vascular invasion (2 vs. 21%, p = 0.032), and tended to be associated with less extra-hepatic localization (4 vs. 18%, p = 0.061). Three patients had extra-hepatic metastasis or vascular involvement at diagnosis even though they were in a screening program prior to the diagnosis of HCC. These 3 patients were male, cirrhotic and older than 50 years of age. As baseline liver disease, one patient had an alcohol-induced liver disease, one patient had a NASH and the third one a chronic hepatitis B. As comorbidity, 2 of these 3 patients had an insulin-dependent diabetes mellitus.
Tumor classification and staging.
| Parameter | HCC surveillance in the last 12 months | p-value | |
|---|---|---|---|
| Yes N = 48 (100.0%) | No N = 34 (100.0%) | ||
| Barcelona Clinic Liver Cancer (BCLC) classification | < 0.0001 | ||
| 0 | 1 (2.1%) | 0 (0.0%) | |
| A | 31 (64.6%) | 5 (14.7%) | |
| B | 13 (27.1%) | 16 (47.1%) | |
| C | 3 (6.3%) | 13 (38.2%) | |
| Within Milan criteria | < 0.0001 | ||
| Yes | 33 (68.8%) | 7 (20.6%) | |
| No | 15 (31.3%) | 27 (79.4%) | |
| Child-Pugh Status | 0.73 | ||
| A | 27 (56.3%) | 22 (64.7%) | |
| B | 17 (35.4%) | 10 (29.4%) | |
| C | 4 (8.3%) | 2 (5.9%) | |
| Model for End-Stage Liver Disease (MELD) Score (mean ± SD) | 9.4 (4.0) | 9.1 (5.1) | 0.49 |
Wilcoxon test for comparison of continuous outcomes. Fisher’s exact test for comparison of categorical outcomes.
HCC characteristics.
| Parameter | HCC surveillance in the last 12 months | p-value | |
|---|---|---|---|
| Yes N = 48 (58.5%) | No N = 34 (41.5%) | ||
| Extrahepatic metastases | 0.06 | ||
| Yes | 2 (25.0%) | 6 (75.0%) | |
| No | 46 (62.2%) | 28 (37.8%) | |
| Vascular involvement | 0.0032 | ||
| Yes | 1 (12.5%) | 7 (87.5%) | |
| No | 47 (64.4%) | 26 (35.6%) | |
| Unknown | 0 (0.0%) | 1 (100.0%) | |
Fisher’s exact test for comparison of categorical outcomes.
Figure 3 shows the eligibility of patients for curative and palliative treatments according to their enrollment in a surveillance program. Only 15% of the patients not included in a surveillance program were eligible for a curative therapy.
DiscussionThese results identify statistically significant and clinically relevant differences in patients diagnosed with HCC depending on their participation in a surveillance program or not. Patients who benefited from a regular screening were diagnosed at an earlier stage and were eligible more frequently for curative treatments. These patients did not have a higher education than the patients not enrolled in surveillance, but they did more often have a private health insurance. Care-givers have a strong impact on screen-ing; patients treated by a liver specialist were much more often enrolled in a surveillance program.
The demographic characteristics of our patients showed a strong male predominance with a ratio of 6:1. It is well known that HCC affects men more frequently than women and a similar ratio has been reported in Spain.16 In the Swiss Hepatitis C Cohort we found a ratio 3:1.17 This suggests that other etiologies such as alcohol, NASH and hepatitis B are more predominant in males than in females. The majority of the patients were diagnosed in their early sixties, which explains why half of our patients were retired. In line with the Spanish experience, advanced age was not a discriminatory factor against screening.16 Actually, age should not be a factor since radio-frequency ablation and TACE are particularly successful in small tumors and can be administered in older patients. Severe cardiovascular co-morbidity did influence screening. Patients with this co-morbidity are likely not to benefit from screening and were not included in a surveillance program. Obesity has been linked to HCC. Males with a BMI above 35 increase their risk for HCC by a factor of 4.5, much more than for any other kind of cancer.18 The BMI in our cohort can be considered normal with a median of 25.9. However, we can not exclude that overweight patients lost weight before inclusion in the cohort.
Our results identify factors that affect screening some of which are patient-related and some of which are physician-related. For patients, neither the level of education nor the type of occupation influenced inclusion in a surveillance program. In contrast, the type of insurance did. Patients who contracted a private insurance were also those who participated more frequently in a surveillance program. This parameter likely identifies patients with interest in their health who are seeking adequate management. The type of physician (whether patients were followed by a liver specialist or not) was also strongly associated with surveillance. Despite guidelines recommending surveillance of patients at risk,3–6 and data supporting the cost-effectiveness of regular screening,9–14 these measures are insufficiently implemented by non-liver specialists. The importance of screening patients at risk should be better recognized. Progresses in this area will improve the outcome of patients diagnosed with HCC.
Inclusion in a surveillance program was associated with diagnosis at an earlier stage. Our data confirm other publications that show that screened patients are more likely to be eligible for curative treatment.19–21 Patients in a surveillance program were more frequently BCLC 0 or BCLC A, were more frequently diagnosed within the Milan criteria and had less macro-vascular involvement. This was independent from the clinical stage of cirrhosis assessed by either Child-Pugh score or MELD score. Several studies have shown that diagnosis of HCC at an early stage translates into longer survival.20,22 Only randomized controlled trials could assure this is not due to lead time bias. The only study that has been performed supports periodic screening, but it presents some weaknesses.8 However, it is unlikely that another trial will be conducted and the available evidence is considered sufficient to recommend surveillance of the patients at risk.23
Our study has several limitations. We do not know whether patients who were not included in a surveillance program were offered screening and refused to participate. Similarly, we do not have data about the adherence to screening and cannot evaluate the acceptance of patients for screening. We are not considering patients who have screening to detect early a recurrence of HCC, these patients form a special collective which can benefit from specific predictive tools.24 These data have been acquired prospectively with a one-center cohort, it is unclear to what extent they are relevant for other centers and other countries.
In conclusion, we found that 35% of patients with cirrhosis and at risk of developing HCC are not regularly screened. Not surprisingly, patients who were regularly screened were diagnosed at an earlier stage of the disease. Although the level of education of the patients did not influence inclusion in a surveillance program, the type of health insurance did. Patients managed by a liver specialist were more frequently included in a surveillance program and had therefore more opportunities to be diagnosed at an earlier stage. This stresses the importance of referring patients who are at risk to centers with expertise in liver diseases.
AcknowledgmentsWe are thankful to the philanthropic committee of the Firmenich Family, which supported this HCC cohort from its start. This project was also supported by the Swiss Foundation against Liver Cancer and the Bern League against Cancer. JFD has received founding from Oncosuisse. We thank Ms N. Sollberger for assistance in managing the data and to Dr. B. Saar for contributing to the initiation of this project.
Financial SupportSwiss Foundation against Liver Cancer, Philanthropic Committee of the Firmenich Family, Bern League against Cancer.