Introduction: Incidence of fatty liver is rising all over the world. Non alcoholic Steatohepatitis which is a subset of fatty liver disease has become a major concern since it is known to progress to liver cirrhosis. Obesity and diabetes mellitus are considered to be the important risk factors for nonalcoholic steatohepatitis. However fatty liver is also seen in non obese and non diabetic individuals. The epidemiology of fatty liver disease slightly differs in different countries, specially where various infections are more prevalent.
Aim: To determine various risk factors responsible for steatosis and to assess severity of steatosis with fibrosis amongst various groups.
Material and methods: Total 1,230 adult autopsies were screened over the period of 4 years. Amongst them 195 cases showing fatty liver were included in the study. Different risk factors responsible for fatty liver were analyzed from the clinical data and laboratory findings obtained from hospital records. Liver histological sections were studied for the presence of steatosis, inflammation and fibrosis. These 3 histological parameters were compared amongst the risk factors.
Results: Alcoholism was found to be the commonest risk factor for staetosis followed by tuberculosis. Other risk factors were cardiac disorders, diabetes, hypertension, Hepatitis B & C infection, HIV and miscellaneous conditions. Overall prevalence of steatosis was found to be 15.8%. Steatosis, inflammation and fibrosis were more common in alcoholics. Tuberculosis was the second commonest risk factor, showed grade 2 to 3 steatosis however inflammation and fibrosis were significantly less in cases of tuberculosis. Findings in other risk factors were variable.
Conclusion: Overall prevalence of fatty liver in this autopsy study was found to be 15.8%. Alcoholism was the commonest risk factor followed by tuberculosis. Fibrosis was mainly observed in association with alcoholism as compared to other risk factors.
Steatosis of liver is the frequent histological finding either in association with other histological features or as the only structural abnormality. The histological spectrum of fatty liver ranges from simple steatosis which may progress to steatosis with inflammation (steatohepatitis) and fibrosis, ending with development of cirrhosis.1-4 Non alcoholic fatty liver disease (NAFLD) which is a subset of fatty liver has become the major public health problem in western countries.3 It is also expanding in Asia pacific regions. The prevalence of fatty liver is found to be between 20 to 50% in general population.6,7 Various conditions are associated with fatty change in the liver. Alcoholism, obesity, diabetes and hepatitis C infection are the most common causes for NAFLD in developed countries.8-10 Due to increased incidence of obesity and their by metabolic syndrome, steatosis of liver having tendency to progressive liver disease, has gained significant importance. However fatty liver has been also found in non obese, non diabetic patients.4 The risk factors for steatosis may be slightly different in developing countries where various infections are more prevalent, mainly in lower socioeconomic group. Hence this autopsy study was carried out to determine various underlying risk factors responsible for steatosis and to assess severity of steatosis with fibrosis amongst various risk factors.
Material and methodsThis was a retrospective autopsy study carried out in tertiary referral hospital. Total 1,230 complete adult medical autopsies were screened over a period of 5 years from 2000 to 2005. Amongst these, 195 random cases, representing entire cohort were included for analysis in which steatosis was seen in more than 10% of hepatocytes. Clinical data was obtained from autopsy records. Majority of the patients were from lower socioeconomic group. Detail autopsy findings were noted in each case. Special emphasis was given to the probable cause of steatosis from available history and laboratory investigations and accordingly patients were grouped together.
At least 2 histopathological sections of the liver were studied for severity of steatosis, inflammation and fibrosis. Steatosis was judged by semiquantitative grading system as per Mofrad PS et al.1 It was labeled as grade 1 when 10 to 30% of hepatocytes showed fatty change, grade 2 - 30 to 60% hepatocytes with fatty change and grade 3 in which more than 60% of the hepatocytes showed fatty change. Inflammation was noted as mild, moderate or sever. Fibrosis was graded as stage 0-no fibrosis, stage 1-pericellular or perisinusoidal fibrosis, stage 2-stage 1 plus portal fibrosis, stage 3-bridging fibrosis and stage 4 - cirrhosis. These histological features were compared amongst various etiological factors responsible for steatosis.
ResultsThe demographic profile of 195 patients showed age ranging from 18 to 80 years with mean age of 21 to 60 years. Male to female ratio was 9:4. Obesity was noticed only in 10 of 195 patients showing steatosis. The commonest risk factor for steatosis was found to be chronic alcoholism 75 (38.4%) followed tuberculosis 50 (25.6%). Other factors were cardiac disorders 10 (5.1%), diabetes 10 (5.1%), hypertension 10 (5.1%), hepatitis B infection 3 (1.5%), hepatitis C infection 3 (1.5%), HIV infection 2 (1.02%) and miscellaneous conditions 32(16.4%). Miscellaneous conditions included cases of malaria, shock, adult respiratory distress syndrome, meningitis, pulmonary thromboembolism, respiratory failure and disseminated malignancy.
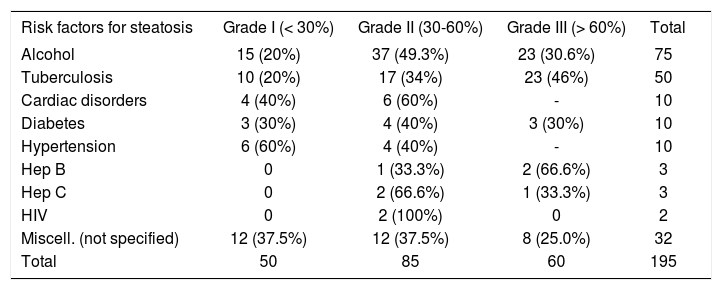
The steatosis in alcoholism and tuberculosis was grade I in 15 (20%) and 10 (20%), grade 2 in 37 (49%) and 17 (34%) and grade 3 in 23 (30.6%) and 23 (46%) respectively, which were found to be important etiologies for steatosis in this study. In cardiac disorders steatosis was grade 1 in 4 (40%) and grade 2 in 6 (60%). None of the case showed sever fatty change. In diabetic patients steatosis was grade 1 in 3 (30%), grade 2 - 4 (40%) and grade 3 in 3 (30%) cases, while in patients with hypertension it was grade I, 6 (60%) and grade II 4 (40%). Amongst hepatitis B, C and HIV infection, none of the case showed grade 1 steatosis while grade 2 steatosis was seen in 1 (33%), 2 (66%), 2 (100%) and grade 3 in 2 (66%), 1 (33%), 0 (0.0%) respectively. In miscellaneous group which consisted of varied etiology, grade 1 steatosis was found in 12 (37%), grade 2 in 12 (37%) and grade 3 in 8 (25%) cases (Table I).
Comparison of grade of steatosis amongst various risk factors.
| Risk factors for steatosis | Grade I (< 30%) | Grade II (30-60%) | Grade III (> 60%) | Total |
|---|---|---|---|---|
| Alcohol | 15 (20%) | 37 (49.3%) | 23 (30.6%) | 75 |
| Tuberculosis | 10 (20%) | 17 (34%) | 23 (46%) | 50 |
| Cardiac disorders | 4 (40%) | 6 (60%) | - | 10 |
| Diabetes | 3 (30%) | 4 (40%) | 3 (30%) | 10 |
| Hypertension | 6 (60%) | 4 (40%) | - | 10 |
| Hep B | 0 | 1 (33.3%) | 2 (66.6%) | 3 |
| Hep C | 0 | 2 (66.6%) | 1 (33.3%) | 3 |
| HIV | 0 | 2 (100%) | 0 | 2 |
| Miscell. (not specified) | 12 (37.5%) | 12 (37.5%) | 8 (25.0%) | 32 |
| Total | 50 | 85 | 60 | 195 |
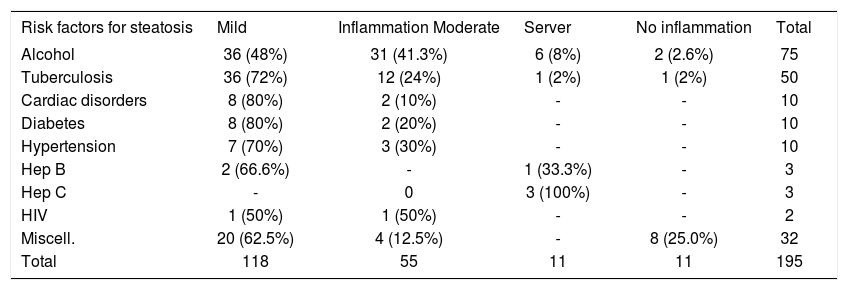
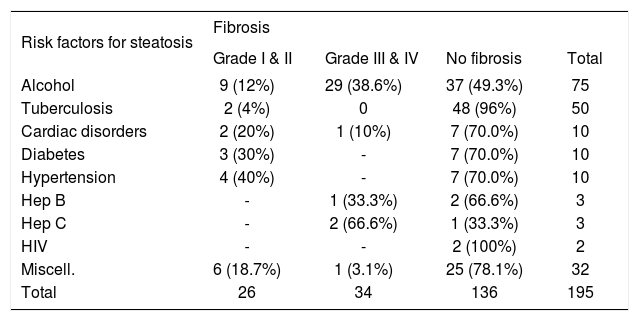
Inflammation was mixed consisting of lymphocytes and polymorphs. It was mainly present in the parenchyma except in hepatitis B and C infection. Inflammation was mild 36 (48%), moderate 31 (41.3%) and sever 6 (8%) in alcoholic patients. In cases of tuberculosis it was mainly mild 36 (72%). Cardiac disorders, diabetes and hypertension showed mainly mild inflammation. In hepatitis B infection, inflammation was mild in 2 (66%), sever in 1 (33%) and in hepatitis C, all the 3 cases showed sever inflammation. In 2 cases of HIV positive patients, inflammation was mild to moderate. Miscellaneous conditions mainly showed mild inflammation 20 (62.5%) (Table II). On analyzing fibrosis, amongst various etiologies of steatosis, alcohol was found to be an important factor responsible for fibrosis. It was also observed that with increasing stage of fibrosis, there was reduction in grade of steatosis. Stage 1 and 2 fibrosis was found in 9 (12%) and 3 and 4 in 29 (38.6%) cases of alcoholics. None of the case of tuberculosis showed stage 3 to 4 fibrosis. In cardiac disorders, fibrosis was mild in 2 (20%) and sever in a single case leading to cardiac cirrhosis. None of the case of diabetes, hypertension and HIV infection showed stage 3 to 4 fibrosis. From 3 cases of hepatitis B infection only 1 (33%) developed cirrhosis, remaining 2 did not show fibrosis. Two (66.6%) out of 3 cases of hepatitis C showed stage 4 fibrosis and in remaining one, there was no fibrosis. In miscellaneous group, fibrosis was absent in 25 (80%), stage 1 & 2 fibrosis was seen in 6 (18.7%) and stage 3 and 4 fibrosis in only 1 (3.1%) case (Table III).
Comparison of grade of inflammation amongst various risk factors.
| Risk factors for steatosis | Mild | Inflammation Moderate | Server | No inflammation | Total |
|---|---|---|---|---|---|
| Alcohol | 36 (48%) | 31 (41.3%) | 6 (8%) | 2 (2.6%) | 75 |
| Tuberculosis | 36 (72%) | 12 (24%) | 1 (2%) | 1 (2%) | 50 |
| Cardiac disorders | 8 (80%) | 2 (10%) | - | - | 10 |
| Diabetes | 8 (80%) | 2 (20%) | - | - | 10 |
| Hypertension | 7 (70%) | 3 (30%) | - | - | 10 |
| Hep B | 2 (66.6%) | - | 1 (33.3%) | - | 3 |
| Hep C | - | 0 | 3 (100%) | - | 3 |
| HIV | 1 (50%) | 1 (50%) | - | - | 2 |
| Miscell. | 20 (62.5%) | 4 (12.5%) | - | 8 (25.0%) | 32 |
| Total | 118 | 55 | 11 | 11 | 195 |
Comparison of stage of fibrosis.
| Risk factors for steatosis | Fibrosis | |||
|---|---|---|---|---|
| Grade I & II | Grade III & IV | No fibrosis | Total | |
| Alcohol | 9 (12%) | 29 (38.6%) | 37 (49.3%) | 75 |
| Tuberculosis | 2 (4%) | 0 | 48 (96%) | 50 |
| Cardiac disorders | 2 (20%) | 1 (10%) | 7 (70.0%) | 10 |
| Diabetes | 3 (30%) | - | 7 (70.0%) | 10 |
| Hypertension | 4 (40%) | - | 7 (70.0%) | 10 |
| Hep B | - | 1 (33.3%) | 2 (66.6%) | 3 |
| Hep C | - | 2 (66.6%) | 1 (33.3%) | 3 |
| HIV | - | - | 2 (100%) | 2 |
| Miscell. | 6 (18.7%) | 1 (3.1%) | 25 (78.1%) | 32 |
| Total | 26 | 34 | 136 | 195 |
The prevalence of liver steatosis ranges from 20 to 50 % in western countries which is rising every year.6,7 The overall prevalence of steatosis in this autopsy study was found to be 15.8%. This prevalence is similar to western population.11 Alcohol, diabetes and obesity are considered to be leading factors for steatosis in developed countries8,9 Leavy CM12 analyzed 270 patients of fatty liver on histology and found that the alcoholism was the commonest cause for steatosis 43.3%, followed by diabetes 6.3%, heart disease 4.07%, obesity 2.6%, gall bladder disease 2.2%, infections 1.8%, neoplasms 1.8%, gastrointestinal ulceration 1.8 %, pancreatic disease 1.4% and CNS disease 1.4%. Similarly we have also found that the commonest factor for steatosis was chronic alcoholism. Second common factor was tuberculosis. While analyzing data on the risk factors for steatosis, it was found that there was a lot of overlap amongst the risk factors. There was no clear history about chronic alcoholism in some of the patients since the presentation of the patients varied. The error due to overlap was minimized by correlating history, investigations with the autopsy findings. Of 75 cases of alcoholics, steatosis was between grade 2 to 3, inflammation ranged between mild to moderate and 38.6 % developed stage 3 to 4 fibrosis. Hence alcoholism was found to be a major factor responsible for development of liver cirrhosis.
Tuberculosis was the second most common risk factor for steatosis after alcoholism in this study. The steatosis in tuberculosis was mainly grade 2 to 3, inflammation was mild to moderate and fibrosis was seen in only 2 (4%) cases which was limited to stage 1 & 2. It was interesting to note that there was not a single case with grade 3 to 4 fibrosis. This may be due to poor socioeconomic status leading to malnutrition and cachexia that are responsible for steatosis in these cases. 13 Steatosis has been a common finding in patients with tuberculosis. The prevalence ranges from 8 to 40% which is in accordance with our results.14,15 Association of liver cirrhosis with tuberculosis is not unusual.15 Cirrhotics are more prone for various types of bacterial infections, one of which is tuberculosis specially in endemic areas like India.16 In this study, though tuberculosis was the second most common cause of steatosis, liver fibrosis was not seen. This may be attributed to absence of underlying liver disease in these patients.
In cardiac disorders, diabetes mellitus and hypertension, steatosis and inflammation was mainly grade 1 to 2. Majority (70%) of them did not show evidence of fibrosis. Fibrosis was seen in only 3 cases (30%) of cardiac disease of which only 1 patient developed cardiac cirrhosis which was the case of congestive cardiac failure. None of the cases of diabetes mellitus and hypertension showed grade 3 to 4 fibrosis. Cirrhosis is found to be 2 to 3 times more frequent in diabetes mellitus than non-diabetic patients17,18 The overall mortality rate in fatty liver disease is determined by the risk factors posed by co morbid conditions with fatty liver disease such as diabetes and obesity.5 In this study majority of our patients were non-obese and from lower socioeconomic group. Fatty liver disease has been also reported in non-obese and non-diabetic individuals. Wanless IR and Lentz JS19 in their autopsy study have reported 18.5% incidence of NAFLD in obese patients and 2.7% in lean patients. This incidence of steatosis in non obese individuals is slightly lower as compared to our patients. Hypertension is also a part of metabolic syndrome which can give rise to a type of fatty liver disease (NAFLD). Incidence of steatosis in hypertensive has been reported to be around 30% which may be related to increased insulin resistance and body weight20,21 Regarding hepatitis B,C and HIV infection, steatosis was between grade 2 to 3. Inflammation was variable in them. One patient of hepatitis B infection and 2 hepatitis C infection showed grade 4 fibrosis, remaining did not show evidence of fibrosis. Steatosis is not a common feature of hepatitis B infection; however 10 to 20% patients of hepatitis B infection can have steatosis possibly due to overlap with metabolic syndrome.22 In hepatitis C infection, steatosis is one of the histological diagnostic features of hepatitis C infection. Both these infection are chronic and can lead to liver fibrosis. In this study we could not come out with definite conclusion with respect to steatosis and fibrosis in hepatitis B, C and HIV infection. This is because autopsies were not indicated in majority of the patients with HBV, HCV or HIV infection. Hence number of patents were very few. Amongst 18 HIV positive patients, steatosis was seen in 2 cases which was grade 2, showing mild to moderate inflammation and no fibrosis. Simple steatosis in HIV patients can be because of malnutrition, Cachexia or therapy related.23 It can be associated with HBV or HCV co-infection. Changes of developing fibrosis with coinfection is high, however we did not get any information about co-infection in HIV patients. In miscellaneous group, 32 (7.4%) of these showed varying degree of steatosis with mild to moderate inflammation. Fibrosis was stage 1 & 2 in 6 (18.7%) and stage 3 & 4 in 1 (3.1%) cases. Definite cause of steatosis and fibrosis could not be judged from available autopsy data in this group.
In conclusion, prevalence of steatosis at autopsy was found in 15.8%. Majority of these patients were non obese, non alcoholic and from lower socioeconomic group. Alcoholism and tuberculosis were the most important risk factors for steatosis. Fibrosis was mainly observed in association with alcoholism as compared to other risk factors.