Telangiectatic hepatocellular adenoma is a rare, recently recognized subtype of benign liver tumor that may very rarely undergo transformation into hepatocellular carcinoma. We report an unusual case of a 75-year-old woman with no history of oral contraceptive use that underwent malignant transformation of a telangiectactic hepatocellular adenoma. No risk factors for adenoma development were identified in this otherwise healthy woman. Radiological characteristics, gross features and histopathology are herein described. In conclusion, telangiectatic hepatocellular adenoma can undergo malignant transformation. Further studies are needed to better clarify the factors associated with malignant progression.
Hepatocellular adenomas comprise a heterogeneous group of rare, primary, benign tumors, in young to middle-aged women with a long history of oral contraceptive use.1 Four subgroups are identified based ondistinctive molecular and histological criteria: HNF1α-mutated adenomas, β-cate-nin-mutated adenomas, inflammatory and/or telangiectatic adenomas, and hepatocellular adenomas without markers.1,2 The characterization of these tumors is relevant, since their clinical course and prognosis markedly differ. Telangiectatic hepatocellular adenomas (THCA) have been mostly associated with hemorrhage rather than with malignant transformation, whereas β-catenin-mutated tumors are more frequently associated with the development of hepatocellular carcinoma.2 We herein describe the case of a woman with hepato-cellular carcinoma arising in a telangiectatic adenoma.
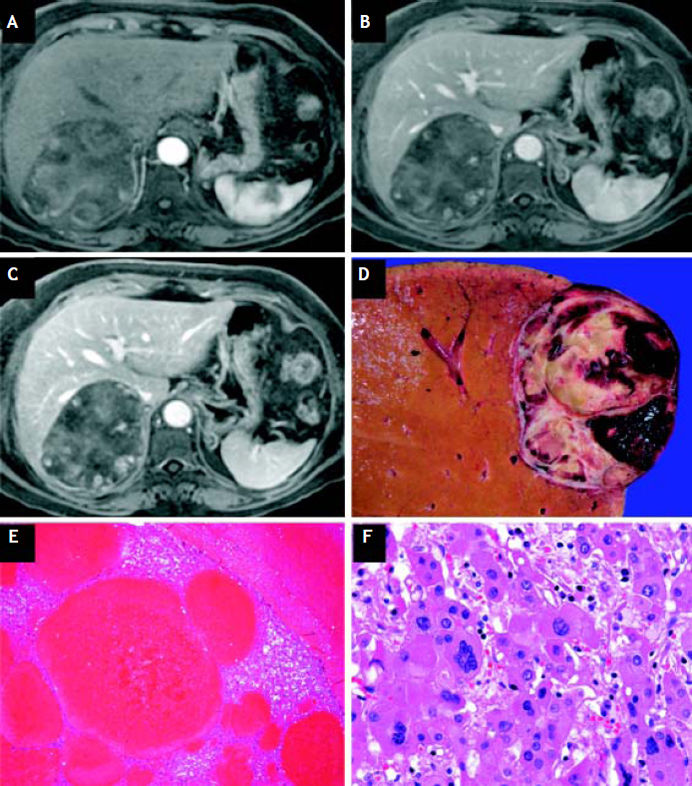
Case ReportA 75-year-old woman was admitted with a 3-month history of early satiety, abdominal distention, heartburn and upper right abdominal pain, irradiated to the scapula. She had no significant weight loss, history of liver disease, alcohol abuse or oral contraceptive use. A right hepatic lobe tumor was identified on a screening abdominal ultrasound performed in another institution. On admission, the physical examination was irrelevant except for tenderness in the right upper abdominal quadrant. Laboratory evaluation revealed normal liver enzymes, bilirubin, and coagulation profile. There was no leukocytosis or anemia. A screening serology profile for viral hepatitis was negative/un-reactive, and her serum alpha-fetoprotein concentration was normal (2.78 ng/mL; range 0-40 ng/mL). Magnetic resonance imaging (MRI) showed an intrahepatic tumor involving segment VII and measuring 10 cm in its largest diameter (Figures 1A-1C). Right lobe hepatectomy was performed. Grossly, an encapsulated, well-delimitated tumor of 9 cm in its greatest dimension, with central fibrosis and hemorrhage was observed (Figure 1D). Microscopically, the tumor was composed of well-differentiated neoplastic hepatocytes with loss of the normal trabecular array adjacent to the cystic spaces (Figure 1E). Nucleomegaly, irregular nuclear membranes, hyperchromasia, loss of the nucleus/cytoplasm ratio and occasional multinucleation were also observed (Figure 1F). The diagnosis of hepatocellular carcinoma originating in a telangiectatic adenoma was reached. After six months of follow-up, the patient is symptom-free and no recurrent disease has been documented.
Arterial phase (A), portal phase (B), and venous phase (C) magnetic resonance imaging. Macroscopic examination of the liver resection (D) showing a well-defined, encapsulated lesion with a heterogeneous surface with hemorrhage, necrosis and degenerative changes. The remaining liver parenchyma is brown, with normal vascularity. Low power (E) view of hepatic parenchyma with ectatic, thin-walled vessels surrounded by hepatocytes with regenerative changes (H&E, × 20). High magnification microscopy (F) showing wide trabecular growth with binucleation, nucleus/ cytoplasm ratio alteration, nuclear atypia and giant cell changes in neoplastic hepatocytes (H&E, x 100).
Hepatocellular adenomas occur in 1-3 per 100,000 young women who use oral contraceptives. THCAs comprise approximately 15% of hepatocellular adenomas (HCA). A high body mass index has also been associated with an increased incidence. Diagnostic criteria include trabecular hepatocellular proliferation displaying short fibrous structures, which contain small amounts of extracellular matrix associated with thickened arterial walls. Additional histological findings include ductular reaction, inflammatory infiltrate, the presence of sinusoidal dilatation, and marked ectasia.2
Malignant transformation of HCA approaches 4.2%.3 However, only 12 previously reported cases of THCA have harbored hepatocellular carcinoma, which suggests that it is an unrecognized disease.2 A recent case series of HCAs reported a mean size of 11.3 cm in cases associated to malignant transformation.3 Aside from the size, other risk factors for malignancy include a history of androgen or anabolic steroid use, male gender, glycogen storage disease, HCAs with dysplasia or β-catenin activation.2,3
Hemorrhage and malignant transformation into hepatocellular carcinomas are the two main reasons for surgical treatment.4–6
In conclusion, THCAs are rare, benign tumors that can progress to hepatocellular carcinoma. Therefore, additional research is warranted in order to define a better selection of surgical candidates.
Abbreviations- •
THCA: telangiectatic hepatocellular adenomas.
- •
MRI: magnetic resonance imaging.
- •
HCA: hepatocellular adenomas.
There are no sources of funding or potential conflicts of interest to disclose.