Introduction. Model for end-stage liver disease (MELD) is an accurate predictor of mortality in patients with cirrhosis, and has been used on liver allocation in Brazil since 2006. However, its impact on organ allocation, waiting list and post-transplant mortality is still poorly characterized. This study aimed to assess the impact of implementation of the MELD system on liver allocation and mortality after liver transplantation (LT) in Southern Brazil.
Material and methods. Adult patients with chronic liver disease on the waiting list for primary deceased-donor LT were divided into two cohorts (pre- and post-MELD implementation) according to the date of waiting list placement. Disease severity, as assessed by MELD score at placement, was similar in both cohorts. Patients were followed for at least 18 months to assess the outcomes of interest (death/LT).
Results. Higher MELD scores correlated with waiting list mortality, which increased 20% with each additional point (HR 1.2; 95%CI 1.14–2.26; p < 0.001). Waiting list mortality was 30.9% before and 21.7% after MELD implementation (nonsignificant). Transplant rate increased after MELD implementation (52 vs. 40%, p = 0.002). After excluding patients with hepatocellular carcinoma, mean MELD scores at LT were significantly higher in the MELD era (p < 0.01). There was no significant correlation between MELD scores at LT and post-LT survival. During 18-month follow-up, post-LT mortality rate was 25.4% before and 20% after MELD implementation (nonsignificant).
Conclusion. MELD implementation was associated with a reduction in waiting list mortality. Although sicker patients received LT in the MELD era, post-transplant survival was similar in both periods.
In Brazil, until recently, the basis for deceased donor liver allocation was time spent on the waiting list, except for patients with acute liver failure or those requiring urgent retransplantation. With the primary objective of reducing mortality among patients on the waiting list for liver transplantation (LT), in July 2006, the Brazilian National Transplant System (Sistema Nacional de Transplantes, SNT), operated by the Brazilian Ministry of Health,1 changed its criteria for allocation of deceased donor allografts -hitherto based exclusively on time accrued on the transplant list– and instituted severity-based criteria. The SNT adopted the model for end-stage liver disease (MELD) scoring system to organize patients by disease severity.2,3
In the United States, implementation of the MELD system improved the liver allocation process. Not only did waiting list mortality decline by 3.5% in the post-MELD era, but the number of deceased donor LTs increased 10.2% and the number of patients placed on the waiting list decreased 12% as compared to the pre-MELD period,4 with no negative effect on the overall post-LT survival rate.4–9
In Brazil, all activities associated with organ and tissue procurement and distribution are regulated and coordinated by the SNT, which does not, however, monitor the activities of transplant teams. Therefore, there is no information on the potential nationwide impact of the introduction of the MELD score as a criterion for liver allocation; the only data available are from isolated transplant centers.10,11
The present study sought to assess the impact of implementation of the MELD system on deceased donor liver allograft allocation and post-LT mortality at a referral center in Southern Brazil.
Material and MethodsThis was a retrospective cohort study. The database of the Liver Transplantation Group of Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, in Porto Alegre, Brazil, was used to construct two cohorts:
- •
The “pre-MELD” cohort, which comprised patients who were placed on the waiting list or received LT between July 1, 2004 and June 30, 2006 (324 patients, 130 of whom underwent LT during the study period).
- •
The “post-MELD” cohort, which comprised patients who were placed on the waiting list or received LT between July 1, 2006 and July 31, 2008 (221 patients, 115 of whom underwent LT during the study period).
All patients included in the study were adults (with the sole exception of a 16-year-old male) with chronic liver disease who had been placed on the LT waiting list or undergone primary deceased donor LT. Patients who were placed on the waiting list due to primary allograft failure or severe acute liver failure were excluded from analysis, as these patients automatically receive maximum priority.
Before implementation of the MELD scoring system -henceforth, in the pre-MELD era- the only criteria for allocation were ABO compatibility and seniority (time accrued on the waiting list). In both periods (pre- and post-MELD), the minimum criteria for waiting list placement were those defined by the American Association for the Study of Liver Diseases.12
Study variablesWe analyzed demographic data (age and sex), clinical information (presence or absence of concomitant hepatocellular carcinoma [HCC]), laboratory parameters (total bilirubin, creatinine, prothrombin time [international normalized ratio, INR], serum sodium), and survival rates (while on the waiting list and post-transplantation).
All patients were followed for at least 18 months after LT.
MELD scores were calculated using the modified United Network for Organ Sharing (UNOS) formula:13
MELD = 3.8[Ln serum bilirubin (mg/dL)] + 11.2[Ln INR] + 9.6[Ln serum creatinine (mg/dL)] + 6.4.
MELD scores were calculated for two different points in time, using the results of lab work performed on the day of list placement and on the day of LT. No points were added for presence of HCC.
The study was approved by the Institutional Review Board of the Santa Casa de Misericordia de Porto Alegre Hospital, which is accredited by the Office of Human Research Protections.
Statistical analysisData were processed and analyzed in the Statistical Package for the Social Sciences (SPSS) 17.0 software environment (SPSS Inc., Chicago, Illinois, USA).
Quantitative data were expressed as mean, standard deviation, and range. For asymmetrically distributed data, the median and interquartile range (P75-P25) were used instead. Categorical data were expressed as absolute and relative frequencies.
Comparison of means between groups was performed with the Student t-test, or its nonparametric counterpart in case of skewed data. For categorical variables, we used the chi-square test or, in case of low frequencies, Fisher’s exact test.
Survival curves were constructed using the Kaplan-Meier method, and the significance of comparisons determined by the log rank test. The Cox proportional hazards model was used to obtain hazard ratio (HR) estimates (crude or adjusted) and their respective 95% confidence intervals (95% CI).
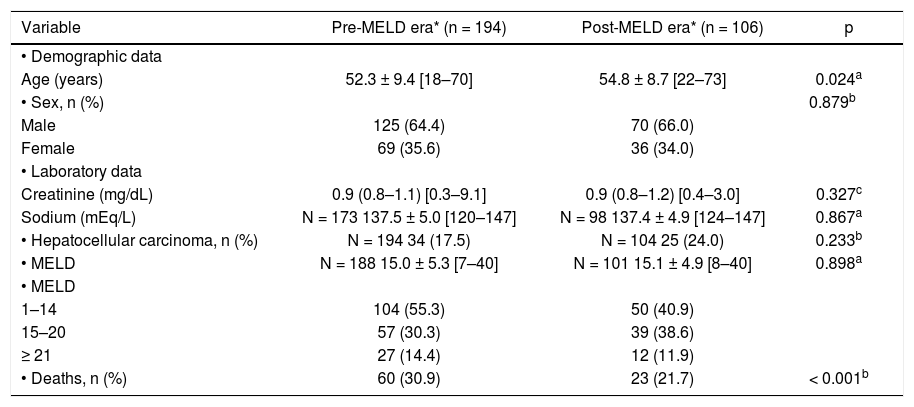
ResultsProfile and status of patients on the LT waiting list in the pre and post-MELD erasA total of 300 patients placed on the LT waiting list –194 in the pre-MELD era and 106 in the MELD era– were analyzed. The mean age of patients placed on the list was significantly higher in the MELD era as compared to the pre-MELD period. In both periods, the majority of patients were male (Table 1). The severity of liver disease, as assessed by MELD scores, was similar in both periods. More patients with HCC were included in the MELD era. There were fewer deaths on the waiting list in the MELD era (21.7 vs. 30.9% in the pre-MELD era; p < 0.001). In both periods, progressively higher MELD scores were associated with higher risk of waiting list mortality; each additional point on the score increased the odds of death by 20% (HR 1.2; 95%CI 1.14–2.26; p < 0.001).
Profiles and outcomes of patients on the waiting list for liver transplantation (LT) before and after implementation of the MELD scoring system.
| Variable | Pre-MELD era* (n = 194) | Post-MELD era* (n = 106) | p |
|---|---|---|---|
| • Demographic data | |||
| Age (years) | 52.3 ± 9.4 [18–70] | 54.8 ± 8.7 [22–73] | 0.024a |
| • Sex, n (%) | 0.879b | ||
| Male | 125 (64.4) | 70 (66.0) | |
| Female | 69 (35.6) | 36 (34.0) | |
| • Laboratory data | |||
| Creatinine (mg/dL) | 0.9 (0.8–1.1) [0.3–9.1] | 0.9 (0.8–1.2) [0.4–3.0] | 0.327c |
| Sodium (mEq/L) | N = 173 137.5 ± 5.0 [120–147] | N = 98 137.4 ± 4.9 [124–147] | 0.867a |
| • Hepatocellular carcinoma, n (%) | N = 194 34 (17.5) | N = 104 25 (24.0) | 0.233b |
| • MELD | N = 188 15.0 ± 5.3 [7–40] | N = 101 15.1 ± 4.9 [8–40] | 0.898a |
| • MELD | |||
| 1–14 | 104 (55.3) | 50 (40.9) | |
| 15–20 | 57 (30.3) | 39 (38.6) | |
| ≥ 21 | 27 (14.4) | 12 (11.9) | |
| • Deaths, n (%) | 60 (30.9) | 23 (21.7) | < 0.001b |
MELD: model for end-stage liver disease. Pre-MELD era: 2004–2006; post-MELD era: 2006–2008. Data expressed as mean ± standard deviation, median (interquartile range), [range], or n (%) as appropriate. p denotes the significance level.
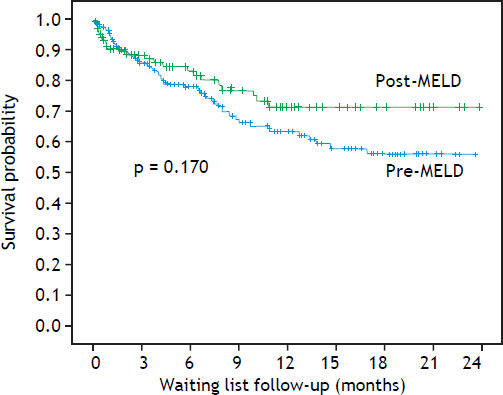
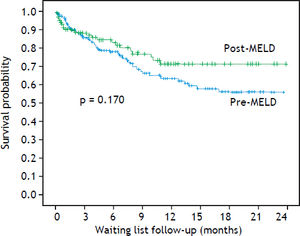
Although fewer patients died on the waiting list during the MELD era as compared to the pre-MELD era, multivariate analysis showed no significant difference in mortality rates between these periods, regardless of age, MELD score, serum sodium, creatinine, and presence or absence of HCC at the time of list placement (HR 0.79; 95%CI 0.47–1.31; p = 0.361). Figure 1 shows a comparison of the survival curves of patients on the waiting list in the pre- and post-MELD eras.
Pooled analysis of patients who died while on the waiting list and those removed from the waiting list due to deterioration of clinical status or progression of HCC yielded rates of 34.0 and 24.5% in the pre-and post-MELD eras, respectively (HR 1.39; 95%CI 0.94–2.04; p = 0.116). In the pre-MELD era, fewer patients were removed from the waiting list due to clinical worsening of the underlying disease as compared to the MELD era (4.9 vs. 7.9%, respectively), but the difference was not significant (p = 0.477).
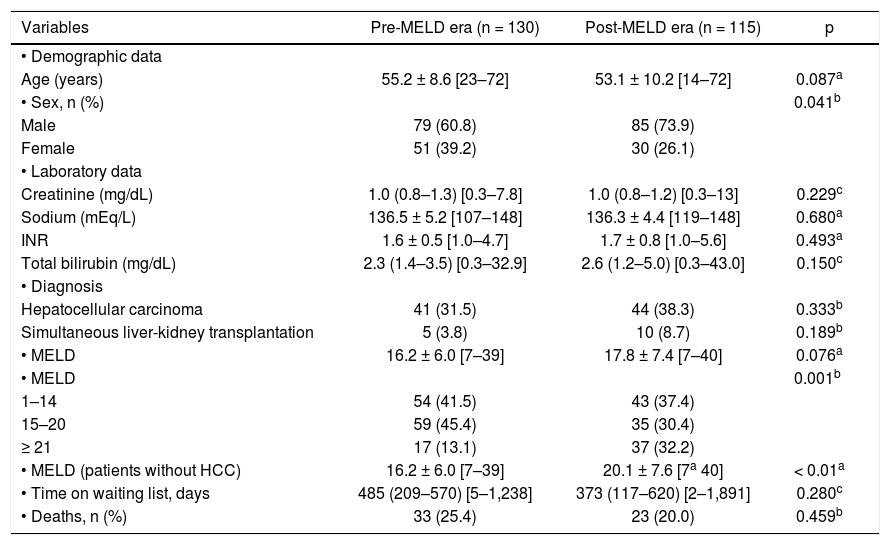
Profile and status of transplanted patients in the pre and post-MELD erasThe study sample included 245 patients who underwent LT: 130 in the pre-MELD era and 115 in the MELD era. The transplantation rate was higher in the latter (52 vs. 40% of all patients placed on the list over the period, p = 0.002). Mean patient age was similar in both cohorts (55.2 vs. 53.1 years). Also in both cohorts, most patients who received transplants were male (60.8% in the pre-MELD era and 73.9% in the MELD era), and in the MELD era, the proportion of men who went on to receive transplants was higher than that of women (p = 0.041) (Table 2). There were no statistically significant between-group differences in the number of transplants performed to treat HCC or in the number of simultaneous liver-kidney transplants. Laboratory parameters on the day of LT, mean MELD scores, and time spent on the waiting list were similar in both cohorts.
Profiles and outcomes (death or survival) of patients who underwent liver transplantation (LT) before and after implementation of the MELD scoring system.
| Variables | Pre-MELD era (n = 130) | Post-MELD era (n = 115) | p |
|---|---|---|---|
| • Demographic data | |||
| Age (years) | 55.2 ± 8.6 [23–72] | 53.1 ± 10.2 [14–72] | 0.087a |
| • Sex, n (%) | 0.041b | ||
| Male | 79 (60.8) | 85 (73.9) | |
| Female | 51 (39.2) | 30 (26.1) | |
| • Laboratory data | |||
| Creatinine (mg/dL) | 1.0 (0.8–1.3) [0.3–7.8] | 1.0 (0.8–1.2) [0.3–13] | 0.229c |
| Sodium (mEq/L) | 136.5 ± 5.2 [107–148] | 136.3 ± 4.4 [119–148] | 0.680a |
| INR | 1.6 ± 0.5 [1.0–4.7] | 1.7 ± 0.8 [1.0–5.6] | 0.493a |
| Total bilirubin (mg/dL) | 2.3 (1.4–3.5) [0.3–32.9] | 2.6 (1.2–5.0) [0.3–43.0] | 0.150c |
| • Diagnosis | |||
| Hepatocellular carcinoma | 41 (31.5) | 44 (38.3) | 0.333b |
| Simultaneous liver-kidney transplantation | 5 (3.8) | 10 (8.7) | 0.189b |
| • MELD | 16.2 ± 6.0 [7–39] | 17.8 ± 7.4 [7–40] | 0.076a |
| • MELD | 0.001b | ||
| 1–14 | 54 (41.5) | 43 (37.4) | |
| 15–20 | 59 (45.4) | 35 (30.4) | |
| ≥ 21 | 17 (13.1) | 37 (32.2) | |
| • MELD (patients without HCC) | 16.2 ± 6.0 [7–39] | 20.1 ± 7.6 [7a 40] | < 0.01a |
| • Time on waiting list, days | 485 (209–570) [5–1,238] | 373 (117–620) [2–1,891] | 0.280c |
| • Deaths, n (%) | 33 (25.4) | 23 (20.0) | 0.459b |
MELD: model for end-stage liver disease. INR: international normalized ratio for prothrombin time. HCC: hepatocellular carcinoma. Data expressed as mean ± standard deviation, median (interquartile range), [range], or n (%) as appropriate. p denotes the significance level.
To assess whether patients who received LT in the MELD era were more severely ill than in the pre-MELD era, we recalculated mean MELD scores after exclusion of patients who underwent LT due to HCC. This procedure yielded a mean score of 20.1-significantly higher than mean scores in the pre-MELD era (16.2) (Table 2).
Stratification of scores into categories (1–14, 15–20, or ≥ 21) showed that patients with higher scores went on to receive LT more often in the MELD era (p = 0.001) (Table 2).
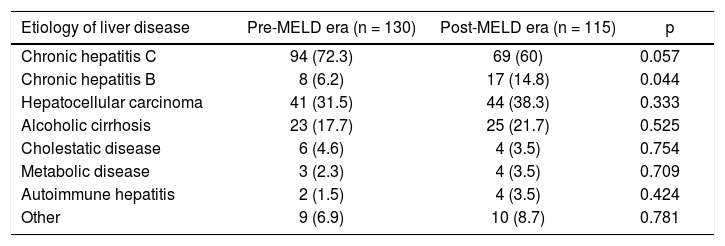
In both periods, HCV-related cirrhosis was the most common indication for LT (72.3 and 60.0% respectively; p = 0.057). More patients with HCC received LT in the MELD era (38.3 vs. 31.5% before implementation of the MELD system; p = 0.333) (Table 3).
Distribution of etiology of liver disease in patients undergoing orthotopic liver transplantation before and after implementation of the MELD scoring system.
| Etiology of liver disease | Pre-MELD era (n = 130) | Post-MELD era (n = 115) | p |
|---|---|---|---|
| Chronic hepatitis C | 94 (72.3) | 69 (60) | 0.057 |
| Chronic hepatitis B | 8 (6.2) | 17 (14.8) | 0.044 |
| Hepatocellular carcinoma | 41 (31.5) | 44 (38.3) | 0.333 |
| Alcoholic cirrhosis | 23 (17.7) | 25 (21.7) | 0.525 |
| Cholestatic disease | 6 (4.6) | 4 (3.5) | 0.754 |
| Metabolic disease | 3 (2.3) | 4 (3.5) | 0.709 |
| Autoimmune hepatitis | 2 (1.5) | 4 (3.5) | 0.424 |
| Other | 9 (6.9) | 10 (8.7) | 0.781 |
MELD: model for end-stage liver disease. Data expressed as n (%). p denotes the significance level as determined by the chi-square or Fisher’s exact test.
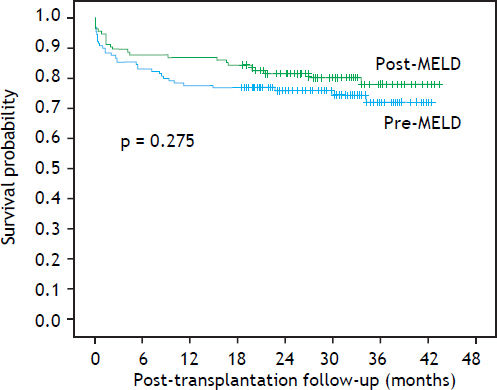
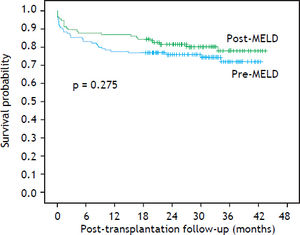
Over ≥ 18 months of follow-up, post-LT mortality rates were 25.4 and 20.0% in the pre-MELD and MELD eras respectively, with no statistically significant difference (Table 2). Mortality was independent of recipient age, serum sodium, creatinine, MELD score, or presence of concomitant HCC (HR 0.79; 95%CI 0.47–1.31; p = 0.361). Post-LT survival curves are shown in figure 2.
DiscussionThis study, conducted at a referral center in Southern Brazil, showed that introduction of the MELD scoring system for deceased donor liver allograft allocation achieved its primary objective-namely, reducing the mortality rate of patients on the LT waiting list without jeopardizing post-transplantation outcomes. The introduction of this new allocation criterion was associated with an approximate 27.9% reduction in waiting list mortality or removal from waiting list due to death or progression of underlying disease. At 24 months after LT, survival rates remained steady at approximately 81.6% (24-month post-LT survival in the pre-MELD era: 75.9%, p = 0.275). The difference in mortality between the two study periods did not reach statistical significance, corroborating the findings of Freeman, et al.4 According to the authors, this finding probably reflects a change in the dynamics of the universe of patients placed on the LT waiting list rather than inadequacy of allocation criteria.14 In fact, as we will describe in greater detail below, implementation of the MELD system at our service was followed by placement of more severely ill patients on the LT waiting list, which would have at least partly justified a higher waiting list mortality rate. Austin, et al.6 studied the impact of MELD implementation in the U.S., in February 2002, by analyzing UNOS data collected between 1999 and 2004. The introduction of the MELD score as an allocation criterion was initially followed by a slight increase in waiting list mortality, which, among other possibilities, may have been associated with the withdrawal of less severely ill patients from the list. Later on, however, a significant reduction in waiting list mortality was found to have occurred after implementation of MELD system.6
The severity of liver disease in patients placed on the waiting list, as estimated by MELD scores, was similar in both periods, which is unsurprising in view of the absence of modifications in the list placement criteria. On the other hand, the greater number of patients with HCC included in the MELD era may have led to a reduction in mean scores, as these patients usually have preserved liver function. Even so, Sachdev, et al.15 found no differences in the mean MELD scores of patients placed on a waiting list before and after implementation of the MELD system, even after exclusion of patients with HCC from analysis. Conversely, studies using the UNOS database4,16 have reported statistically significant differences in the mean MELD scores of patients included before and after MELD implementation. In our series, however, when patients were stratified by MELD score category (6–14, 15–20, or ≥ 21), the proportion of patients with more severe disease was found to be higher in the MELD era, with a consequent reduction in the number of less severely ill patients placed on the list, which probably denotes greater zeal in waiting list placement. This greater care may also explain, at least partly, the 45% reduction in the number of patients placed on the waiting list in the MELD era as compared to the pre-MELD period.
HCC often arises in patients with fairly well-preserved liver function and low MELD scores. Therefore, their risk is more often related to tumor progression than death on the waiting list because of terminal liver failure. In Brazil, with the introduction of MELD score for deceased donor liver allocation, patients with HCC who meet certain characteristics – ≥ 2 cm, within the Milan criteria, and no indication for resection- are placed in the ‘special situations’ category. In these cases, the minimum MELD score is 20. Patients who do not undergo LT within three months have their MELD score increased to 24; and within six months, to 29. Thus, patients with HCC have benefited from the introduction of MELD score, which explains, at least partly, the greater number of LTs observed in patients with HCC in our series.
Furthermore, the greater number of LTs performed in the MELD era contributed to a reduction in the waiting list.2,14 Other authors have described similar increases in the number of transplants performed after implementation of the MELD scoring system.16,17
This study showed that, in the MELD era, female patients went on to receive transplants with a proportionally lower frequency than male patients. This finding has been reported elsewhere in the literature, which suggests that use of the MELD score as an allocation criterion may be systematically disadvantageous to women. This is likely due to inclusion of creatinine levels in the MELD formula, as women exhibit lower creatinine levels than men at similar levels of renal function impairment.18–20 Both in the pre-MELD era and in the MELD era, median serum creatinine levels were higher in men than in women (pre-MELD, 1.0 [0.8–1.3] vs. 0.9 [0.8–1.2], p = 0.465; post-MELD, 1.0 [0.85–1.3] vs. 0.95 [0.8–1.1], p = 0.078).
As expected, the severity of cirrhosis as assessed by MELD scores on the day of LT was greater in the MELD era, but not significantly different from the mean scores of transplanted patients in the pre-MELD era (16.2 vs. 17.8 respectively; p = 0.076). To assess whether use of calculated MELD scores underestimated mean scores in the MELD era due to the greater number of transplants performed on patients with HCC, who accounted for 38.5% of all transplant recipients in the sample as opposed to 31.5% in the pre-MELD era, we recalculated mean MELD scores after exclusion of patients with a diagnosis of HCC. This procedure yielded a significant difference in mean scores (16.2 vs. 20.1 respectively; p < 0.001). This finding is further supported by the observation that the number of transplants performed on patients with a MELD score of ≥ 21 increased in the MELD era. In other words, implementation of MELD as a criterion for allograft allocation truly led to transplants being prioritized for the sickest patients.
Although the proportion of transplanted patients with MELD scores ≥ 21 was higher in the MELD era, post-LT mortality rates at 18 months or beyond declined from 25.4% in the pre-MELD era to 20.0% after MELD implementation. Furthermore, comparison of 18-month post-LT survival with KaplanMeier curves for both periods showed a trend towards improved survival in the transplantation group after implementation of the MELD scoring system. Pooled analysis of the pre-and post-MELD periods showed that patients who died during > 18-month post-LT follow-up had lower mean scores than those who survived. These findings show that the MELD score was able to prioritize liver allocation to patients with more advanced disease without jeopardizing post-LT survival. This is consistent with previous studies.6,8,9,11,16,21–26
It is well known that the risk of post-LT mortality is higher in patients with higher MELD scores.27–30 However, sicker patients -those with higher scoresalso derive the greatest benefit from transplantation.31,32
Nevertheless, MELD score is not without limitations and may not serve quite well all liver transplant candidates. MELD limitations are related to the inter-laboratory variability of the parameters included in the score, or the inability of the formula to accurately predict mortality in specific settings.33,34 Creatinine, for example, as previously discussed,18–20 can be artificially low for women compared with men as it may be associated with overall muscle mass, which can cause women to have a relatively lower MELD score and potentially lower priority on the waiting list.19,35 Several attempts are underway to improve the applicability and reliability of the formula in specific conditions.
In short, the findings of this study show that, at a single center in Brazil, implementation of the MELD scoring system as a criterion for deceased donor liver allograft location met its objectives: it was associated with a decrease in the waiting list mortality rate and enabled transplantation of sicker patients without jeopardizing post-LT survival. Patients suffering from HCC benefited from the new allocation system due to their adjusted match MELD, leading to a more timely transplantation. We did find that, apparently, use of the MELD system for allocation is placing female patients at a disadvantage. Further studies with larger sample sizes should be performed to address this potential issue.
Abbreviations- •
HCC: hepatocellular carcinoma.
- •
HR: hazard ratio.
- •
INR: International normalized ratio.
- •
LT: liver transplantation.
- •
MELD: model for end-stage liver disease.
- •
SNT: Sistema Nacional de Transplantes (Brazilian National Transplant System).
- •
SPSS: Statistical Package for the Social Sciences.
- •
UNOS: United Network for Organ Sharing.
The study did not receive financial support or grants.