No definitive indications are provided in the literature for pre-TIPS patient workup, which is often limited to prevent the incidence of refractory hepatic encephalopathy or unacceptable deterioration of liver function. Concerning cardiologic workup, efforts are generally limited at excluding ventricular failure or porto-pulmonary hypertension. The cases presented herein focus the attention of the readers on the possible occurrence of post-TIPS paradoxical embolization in the presence of a patent foramen ovale, frequently recognized in adult population. In conclusion, although this complication has been already reported in literature, in the present manuscript we concentrate on possible additional risk factors which may allow to identify a subset of patients with a higher likelihood to experience paradoxical embolization following TIPS. Another important line of information presented herein is the feasibility of percutaneous closure of a patent foramen ovale before TIPS deployment in the presence of portal vein thrombosis and possibly with additional risk factors.
Trans-jugular intra-hepatic porto-systemic shunt (TIPS) is a well-established procedure for the treatment of portal hypertensive bleeding, refractory ascites and vascular diseases of the liver. In recent years, TIPS gained dignity of an independent therapy due to remarkable prognostic results.1–3 Therefore, TIPS is no longer considered merely as a bridge to liver transplantation, but careful patient’s selection is critical to take full advantage from this derivative procedure. However, selection of patients undergoing TIPS, and pre-procedural workup, are often limited to exclude the possible eventual occurrence of refractory encephalopathy or unacceptable worsening of liver function. Concerning post-TIPS hemodynamic changes, efforts are aimed at excluding ventricular failure and porto-pulmonary hypertension.4,5 For this reason, only a basic cardiologic workup, including physical examination, electrocardiogram (ECG), and echocardiogram is part of the evaluation of the TIPS candidate. In selected cases, direct evaluation of pulmonary pressures is also performed by right heart catheterization.
Here we report two cases of patients undergoing TIPS placement, in whom the clinical history provides evidence for the need of a specific cardiologic evaluation in a subgroup of TIPS candidates.
Case ReportCase 1A 64-year-old Caucasian woman with hepatitis C virus (HCV)-related liver cirrhosis (Child-Pugh A, score 6, MELD 11), hemodynamically non-responder to secondary prophylactic therapy for variceal bleeding was referred to our Unit for TIPS placement due to recent recurrent massive variceal bleeding (Table 1). Clinical history included: insulin-dependent type 2 diabetes mellitus and previous post-traumatic deep vein thrombosis of the left superior limb, complicated by pulmonary embolism. Abdominal ultrasound examination and contrast-enhanced computed tomography (CT) scan demonstrated partial thrombosis of the portal vein trunk (≈ 40% of the lumen). After treatment of esophageal varices by endoscopic band ligation, the patient was anti-coagulated with 5.0 mg fondaparinux to prevent portal vein lumen obliteration. An eight centimeter-long, ten millimeter nominal diameter, Viatorr endoprosthesis (W.L. GORE & Associates Inc., Flagstaff, AZ, USA) was placed between the right hepatic vein and the right branch of the portal vein. The endoprosthesis was than impacted at 6 mm within the intra-parenchymal tract. The porto-systemic gradient dropped from 19 to 9 mmHg. No intra-procedural complications were registered. Three hours after the end of the TIPS procedure, the patient complained of neurological symptoms, such as clumsiness of his right hand. Heart rate was 74 bpm, blood pressure was 130-60 mmHg, respiration rate 21 breaths per minute, temperature 36.4 oC, and peripheral oxygen saturation was 96% in room air. No signs or symptoms of infection were evident. As hepatic encephalopathy, a common disturbance of the central nervous system in patients with TIPS, is usually not associated with focal motor deficit and occurs later in the course of clinical history, imaging of the central nervous system was ordered in this patient to assess other diagnoses. Non-contrast-enhanced CT scan of the head showed three focal areas of hypodensity in the left parietal lobe. A contrast enhanced magnetic resonance (MR) imaging study of the brain showed 4 to 7 foci of restricted diffusion, measuring between 4 and 6 mm in size, consistent with embolic sprinkling in the left middle cerebral artery. A comprehensive investigation for conditions responsible for the ischemic and embolic cerebrovascular event was carried out. However, first level investigations (ultrasound/Doppler study of the carotid arteries, ECG, echocardiogram and Holter monitoring) were unremarkable. A transthoracic contrast-enhanced (Sonovue, Bracco International B.V., Amsterdam, NL) echocardiography finally demonstrated a patent foramen ovale (PFO). Contrast-enhanced abdominal CT scan and ultrasonography showed a patent portal vein at 7 days from derivative procedure. A hypercoagulable state was ruled out, and control upper endoscopy revealed a small isolated esophageal varice with no signs of bleeding risk. Fondaparinux was withdrawn and oral anticoagulation with warfarin was started and continued for six months after discharge. During the subsequent ten month follow-up, the patient did not experience any significant clinical events (Child Pugh B, score 8 and MELD 13), and showed complete neurological recovery.
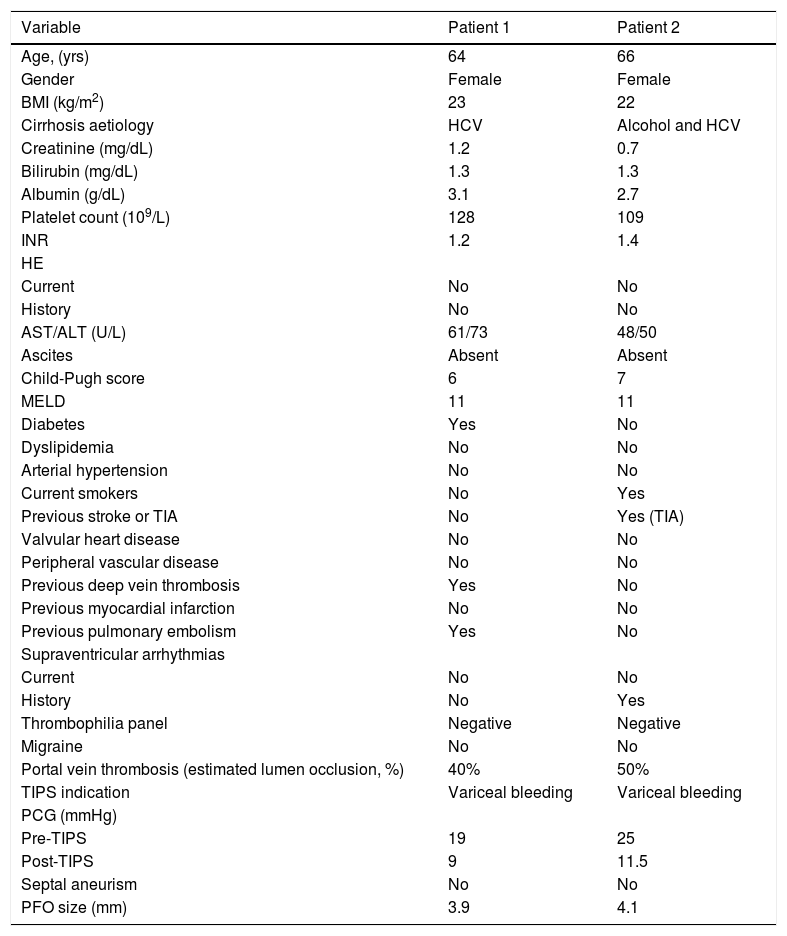
Clinical and hematochemical characteristics of the two patients included in the report.
| Variable | Patient 1 | Patient 2 |
|---|---|---|
| Age, (yrs) | 64 | 66 |
| Gender | Female | Female |
| BMI (kg/m2) | 23 | 22 |
| Cirrhosis aetiology | HCV | Alcohol and HCV |
| Creatinine (mg/dL) | 1.2 | 0.7 |
| Bilirubin (mg/dL) | 1.3 | 1.3 |
| Albumin (g/dL) | 3.1 | 2.7 |
| Platelet count (109/L) | 128 | 109 |
| INR | 1.2 | 1.4 |
| HE | ||
| Current | No | No |
| History | No | No |
| AST/ALT (U/L) | 61/73 | 48/50 |
| Ascites | Absent | Absent |
| Child-Pugh score | 6 | 7 |
| MELD | 11 | 11 |
| Diabetes | Yes | No |
| Dyslipidemia | No | No |
| Arterial hypertension | No | No |
| Current smokers | No | Yes |
| Previous stroke or TIA | No | Yes (TIA) |
| Valvular heart disease | No | No |
| Peripheral vascular disease | No | No |
| Previous deep vein thrombosis | Yes | No |
| Previous myocardial infarction | No | No |
| Previous pulmonary embolism | Yes | No |
| Supraventricular arrhythmias | ||
| Current | No | No |
| History | No | Yes |
| Thrombophilia panel | Negative | Negative |
| Migraine | No | No |
| Portal vein thrombosis (estimated lumen occlusion, %) | 40% | 50% |
| TIPS indication | Variceal bleeding | Variceal bleeding |
| PCG (mmHg) | ||
| Pre-TIPS | 19 | 25 |
| Post-TIPS | 9 | 11.5 |
| Septal aneurism | No | No |
| PFO size (mm) | 3.9 | 4.1 |
BMI: body mass index. INR: international normalized ratio. HE: hepatic encephalopathy. AST: aspartate aminotransferase. ALT: alanine aminotransferase. TIA: transient ischemic attack. MELD: Mayo Clinic end stage liver disease. TIPS: trans-jugular intra-hepatic porto-systemic. PCG: porto-caval gradient. PFO: patent foramen ovale.
A 66-year-old Caucasian woman with alcoholand HCV-related cirrhosis (Child-Pugh B, score 7 and MELD 11) was admitted to our Unit to be evaluated for TIPS placement for a history of recurrent variceal bleeding, not amenable to associated medical and endoscopic treatment (Table 1). Clinical history included: episodic supraventricular tachycardia and a transient ischemic attack of undetermined etiology occurred four years before. Abdominal ultrasound examination and contrast enhanced CT scan demonstrated partial thrombosis of the trunk and right branch of the portal vein (≈ 50% of the lumen). The patient was treated with fondaparinux at prophylactic dose due to the presence of large esophageal varices with red wale marks. A Doppler ultrasound examination of the portal vein conducted five days later showed stabilization of the thrombotic apposition. Evaluation for congenital and/or acquired hypercoagulable states was negative. Meanwhile, cardiologic assessment by transthoracic, contrast-enhanced echocardiography detected the presence of a PFO. Therefore, the patient presented coincident risk factors for paradoxical embolization following TIPS procedure.
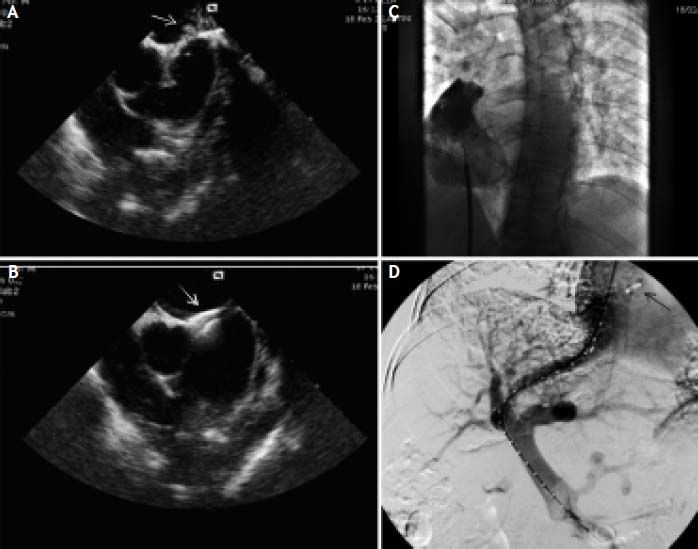
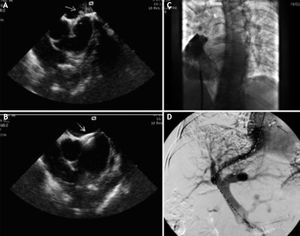
Based on the previous findings, an Amplatzer PFO Occluder (St. Jude Medical, Plymouth, MN, USA) device was released under radioscopic and intracardiac echocardiography guidance (Figure 1A-1C). The procedure was uneventful and PFO could be no longer demonstrated at a further contrastenhanced echocardiography. Three days later, the patient was scheduled for TIPS procedure. A six centimeter long, ten millimeter nominal diameter, Viatorr endoprosthesis was placed between the right hepatic vein and the portal vein branch tributary of the VII hepatic segment. The stent was then impacted at 6 mm in the intra-parenchymal tract. The porto-systemic gradient dropped from 25 to 11.5 mmHg, and the procedure was uneventful (Figure 1D). No clinical signs of paradoxical embolization emerged during hospital stay, and a cerebral MRI was negative for ischemic lesions. After TIPS procedure, the patients was placed on aspirin/clopidogrel for one month, and subsequently on low-dose aspirin. In the succeeding two months follow-up the patient did not experience significant clinical events (Child Pugh B, score 8 and MELD 14).
PFO definition/occlusion and post-TIPS portal vein patency in case 2. A. Intracardiac contrast enhanced (agitated normal saline) echocardiography demonstrating PFO. The white arrow indicate the passage of normal saline in left atrium. B. Intracardiac echocardiography demonstrating correct release of the Amplatzer Occluder (white arrow) across PFO. C. Angiographic confirmation of correct release of the Amplatzer Occluder and adequate PFO occlusion (also confirmed by intracardiac contrast enhanced echocardiography), indeed no contrast medium and normal saline leakage in left cavities was observed. D. Angiography demonstrating post-TIPS patency of the portal vein. The black arrow indicate the previously implanted Amplatzer PFO Occluder.
PFO is a hemodynamically insignificant interatrial communication present in > 25% of the adult population.6,7 However, PFO may serve as a conduit for paradoxical embolization, i.e. the passage of a thrombus from the venous system to the left cardiac cavities. Because PFO is commonly found in the normal population, identification of the subset of patients with higher likelihood to experience paradoxical embolization is critical. Although the size of PFO plays a role in influencing the chance of paradoxical embolization, a 1 mm embolus is sufficient to occlude a large cortical arterial branch, and an embolus of 3 mm occluding the middle cerebral artery can provoke a massive hemispheric infarction.6 Patients submitted to TIPS procedure may present some peculiarities that could increase the risk of paradoxical embolization, if a PFO is present. Blood flow from the inferior vena cava is directed toward the fossa ovalis as it enters the right atrium,6 and thus embolization from the portal vein to the systemic circulation after TIPS deployment has a higher chance of reaching the left cardiac cavities. In addition, elevation in right atrium pressure after opening of the porto-systemic shunt,5 will further increase the chance of a right-to-left cardiac shunt. This latter mechanism could be exacerbated by a coexisting pulmonary embolism or a pre-existing porto-pulmonary hypertension. Portal vein thrombosis, either when is a specific indication to TIPS or an accidental finding in patients with variceal bleeding and/or refractory ascites, is not an infrequent consequence of either vessel wall injury or changes in portal hemodynamic that follow TIPS deployment. Moreover, hypercoagulable states may undermine both patients with non-cirrhotic and cirrhotic portal vein thrombosis.
Acute cerebrovascular accidents due to paradoxical embolization of histoacryl, or crumbling of a portal vein thrombus following TIPS, have been reported in the literature.8,9 On this basis, the Authors suggested to perform echocardiography in TIPS candidate patients with pre-existing portal vein thrombosis, and to adequately inform patients about the risk of paradoxical embolization following the procedure. The cases presented herein provide further support to the possible occurrence of paradoxical embolization following a TIPS procedure. In particular, the occurrence of systemic embolism as a consequence of a TIPS procedure in the presence of a PFO strongly suggests that a scrupulous cardiologic evaluation must be performed at least in patients with pre-existing portal vein thrombosis and/ or in whom conditions such as a hypercoagulable state, increased pulmonary pressures, or history of cerebral ischemic events of undetermined etiology have been documented. As previously mentioned, no definitive indications are provided in the literature for the clinical workup of a patient scheduled for TIPS. In our opinion, cardiologic workup should include a trans-thoracic, contrast-enhanced echocardiography, at least in high-risk patients. Contrastenhanced echocardiography is a validated technique for the detection of PFO,7–10 and has the advantage of being inexpensive (if normal saline is employed), safe and widely available. During contrast echocardiography, PFO is diagnosed if any microbubbles are visible in the left-sided cardiac chambers within 3 cardiac cycles from the maximum right atrial enhancement. Of note, contrast echocardiography could provide additional information, such as the presence of intra-pulmonary functional or anatomical shunts typical of the hepato-pulmonary syndrome. This latter abnormality may represent a further mechanism for paradoxical embolization.
Another important line of information provided by the cases presented herein is the feasibility of percutaneous closure of a PFO before a TIPS placement. Noteworthy, the procedure was uneventful, considering that the general incidence of major and minor complications of percutaneous PFO closure are 1.5 and 7.9%, respectively, although they may be drastically decreased in skilled hands.7,11 Although recent papers12,13 did not showed a clear superiority of PFO closure over medical therapy, interestingly Carroll, et al.13 suggested the possible benefit of PFO closure for patients with a substantial shunt size or atrial septal aneurysm. Moreover, cirrhotic patients submitted to TIPS procedure, as stated above, may present some characteristics that could increase the likelihood of paradoxical embolization in the presence of a PFO. Thus, in the presence of pre-TIPS portal vein thrombosis associated with PFO and possibly with additional risk factors, percutaneous closure of PFO should be strongly considered, preferably assisted by intracardiac echocardiography to enhance PFO definition or occlusion. Moreover, extensive information about the potential risk of systemic embolization following TIPS procedure in the presence of a PFO must be provided even to subjects judged at lower risk.
Abbreviations- •
CT: computed tomography.
- •
ECG: electrocardiogram.
- •
HCV: hepatitis C virus.
- •
MR: magnetic resonance.
- •
PFO: patent foramen ovale.
- •
TIPS: trans-jugular intra-hepatic porto-systemic shunt.
Dr. Vizzutti and Dr. Schepis reports receiving grant support (FS), lecture fees and reimbursement for travel expenses (FV and FS) from Gore. No other potential conflict of interest related to this article was reported.
Financial SupportThis paper was supported by grants from University of Florence (to FV).