Primary biliary cholangitis (PBC) is a chronic cholestatic autoimmune disease that disrupts the cholesterol metabolism. Our aim was to investigate the frequency of dyslipidemias and to evaluate the risk of cardiovascular events in a historic cohort of patients with PBC.
PatientsAll patients attended from 2000 to 2009 with histological diagnosis of PBC were included and were compared with healthy controls. The 10-year cardiovascular risk was estimated by the Framingham risk score.
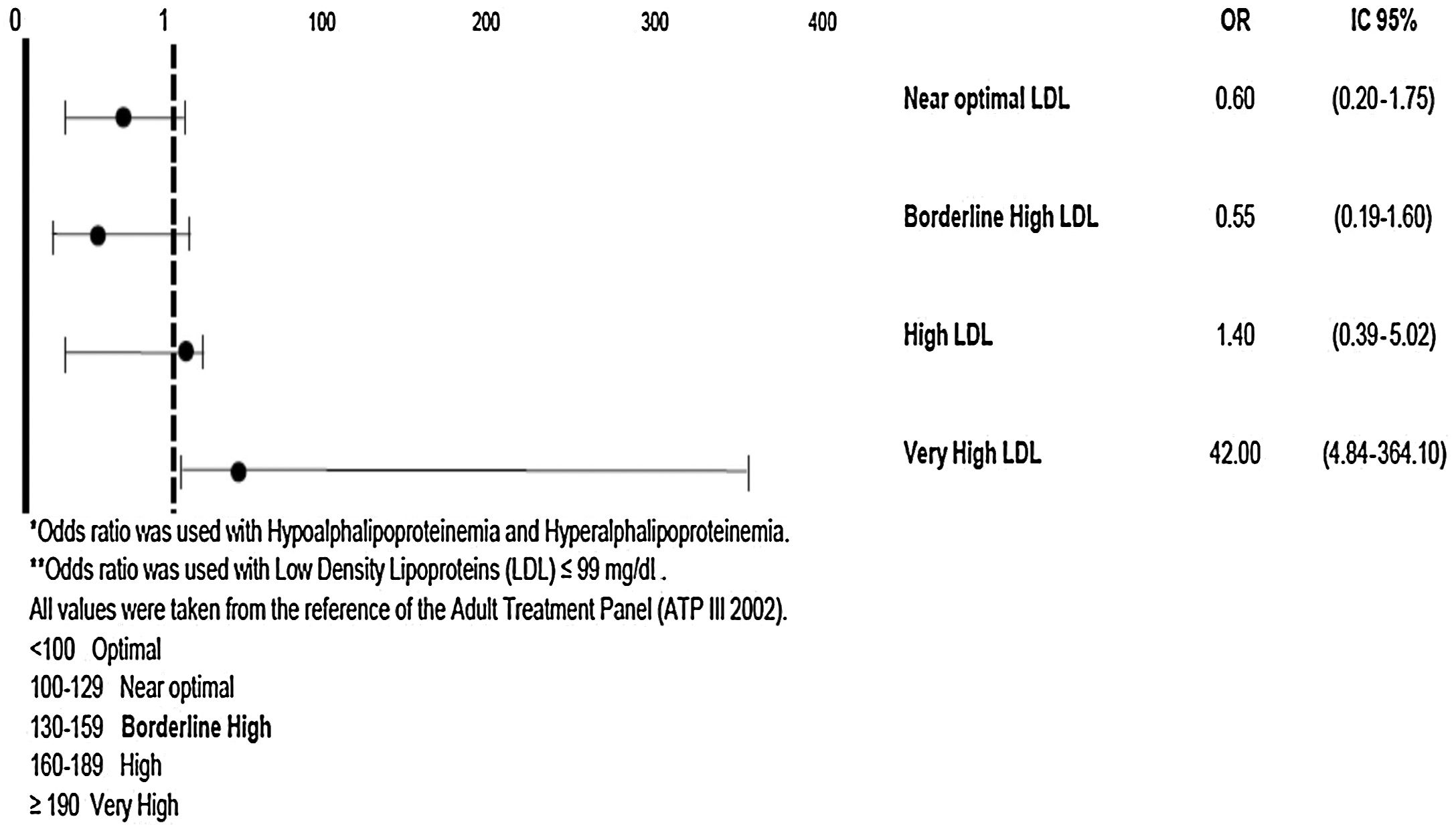
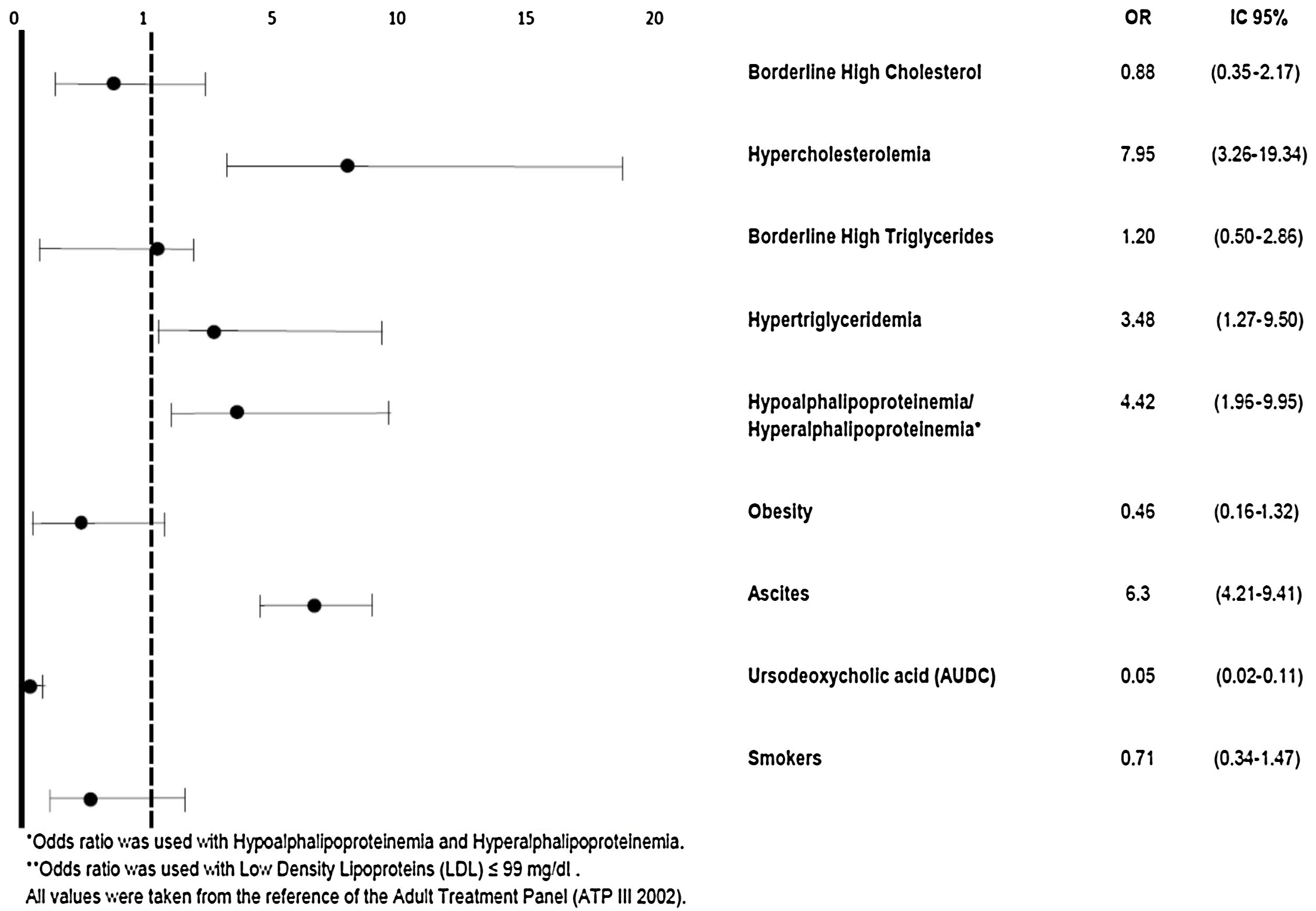
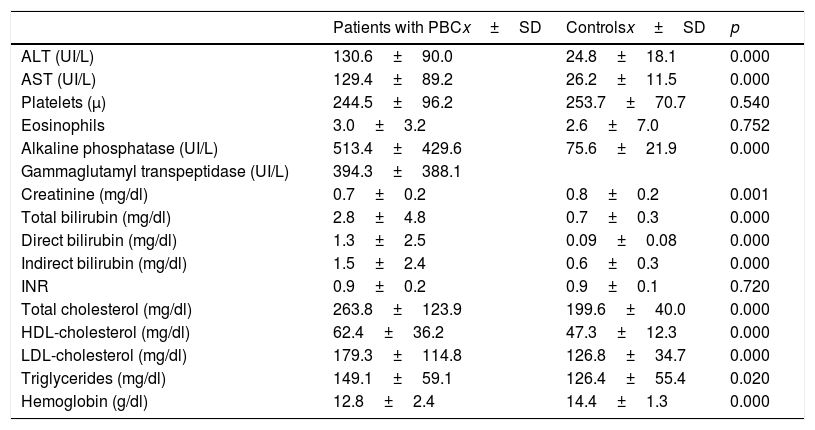
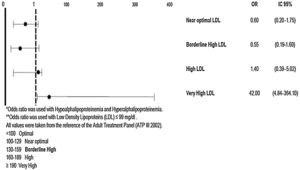
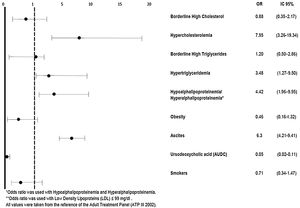
ResultsFifty four patients with PBC were included and compared to 106 controls. Differences in total cholesterol (263.8±123.9mg/dl vs. 199.6±40, p=0.0001), LDL-cholesterol (179.3±114.8 vs. 126.8±34.7, p=0.0001), HDL-cholesterol (62.4±36.2mg/dl vs. 47.3±12.3, p=0.0001) and triglycerides (149.1±59.1mg/dl vs. 126.4±55.4, p=0.001) were found. Hypercholesterolemia (>240mg/dl) was found in 52.4% of the patients with PBC vs. 11% in the control group, high LDL-cholesterol (160–189mg/dl) in 45.2% of the patients with PBC vs. 10% in controls and hyperalphalipoproteinemia (HDL-cholesterol >60mg/dl) in 45.2% of the patients with PBC vs. 16% in controls. The 10-year cardiovascular risk was 5.3%±5.9 in the patients with PBC and 4.1%±5.7 in the control group (p=0.723, IC 95%=0.637–1.104). Only one cardiovascular event (stroke) in a patient with PBC was registered in a mean follow up time of 57.9±36.5 months.
ConclusionsMarked derangements in serum lipids and a high frequency of dyslipidemias are found in patients with PBC, however, these do not increase the risk of cardiovascular events.
Primary biliary cholangitis (PBC) is a chronic cholestatic disease caused by progressive autoimmune-mediated injury to small bile ducts. PBC affects mainly middle-aged women with a female to male ratio of 8:1. In clinical practice derangements in the serum lipids pattern are frequently observed [1,2]. Hyperlipidemia affects 75–95% of the patients with PBC [3]. PBC alters cholesterol metabolism in several ways. Cholestasis reduces bile acid secretion, leading to diminished bile acid synthesis and down-regulation of hepatic cholesterol synthesis. Most of the cholesterol elevation is due to lipoprotein X (LpX), a lipoprotein within the density range of the low density cholesterol (LDL) [4] but with a physical size within the range of the very low density lipoprotein (VLDL) [5]. Also as a result of the gradual loss of LDL receptors in the liver that parallels the severity of the disease, a failure in the clearance by the hepatocytes is observed and an increase in LDL is consequently observed. On the other hand, the high density lipoprotein (HDL) tends to be higher in the earlier stages of PBC and lower in the more advanced stages of the disease [6].
According to the ATP III Guidelines resulting from the Framingham Study, a total cholesterol of 200–239mg/dl is considered as a borderline high value, a concentration above 240mg/dl is considered as a high value and an LDL cholesterol concentration between 160 and 189mg/dl is considered as a high value. No value for hyperalphalipoproteinemia is defined by these ATP III Guidelines [7]. Hypercholesterolemia has been identified as a major risk factor for morbidity and mortality from atherosclerotic disease; however the reason by which there is no increase in the risk of cardiovascular events in patients with PBC despite hypercholesterolemia remains unknown. The aim of our study was to investigate the frequency of dyslipidemias, to evaluate the risk of cardiovascular events and to investigate the frequency of cardiovascular events (acute myocardial infarction, transient ischemic attack or stroke) in patients with PBC.
2Patients and methodsPBC is a relatively uncommon disease, however, our institution is a reference center for this disease. All patients attended at our hospital from 2000 to 2009 with histological diagnosis of PBC were included on this retrolective study. Sample size and power calculations considering cholesterol as the strongest predictor, a type I error <0.05 and a type II error 0.20 resulted in a sample size of 36 patients (expected difference among independent groups, 20% minimum, that is 48–50mg/cholesterol). Patients with PBC were compared to healthy controls. The control group consisted on two healthy organ donors (for each patient) attended during those years, paired by gender and age to every patient with PBC. The total cholesterol, HDL-cholesterol, LDL-cholesterol and triglycerides serum concentrations were extracted from the clinical records of both groups; additionally, the frequency of dyslipidemias, low HDL-cholesterol (<40mg/dl in men, <50mg/dl in women), high LDL-cholesterol (>130mg/dl) and hypertriglyceridemia (>200mg/dl) were recorded. Patients with PBC and controls were compared for metabolic variables, such as cholesterol, HLD-cholesterol, LDL-cholesterol, triglycerides, and for the 10-years risk for cardiovascular disease.
Patients were followed up for the development of cardiovascular events (myocardial infarction of cerebrovascular event). The individual's risk of cardiovascular disease was calculated by means of the Framingham risk score [7] considering age, total cholesterol, smoking status, HDL-cholesterol and blood pressure in order to assess the 10-year risk for developing a heart attack or dying from coronary heart disease.
Statistical analysis was performed using the Student's t test and x2 test (significant values when p<0.05) and the association between variables was evaluated by means of odds ratios.
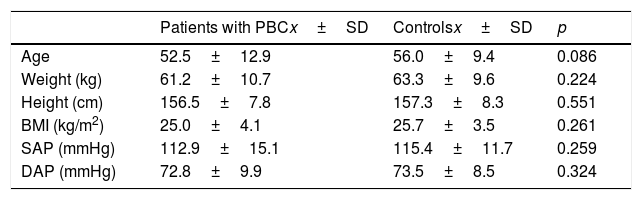
3ResultsFifty four PBC patients were included in the study and were compared with 106 healthy controls. The general characteristics of the patients and controls are depicted in Table 1. Subjects in the control group were similar to patients with PBC regarding age (56 years±9.4 vs. 52.5 years±12.9, respectively p=0.086), systolic arterial pressure (115.4mmHg±11.7 vs. 112.9mmHg±15.1, respectively p=0.259) and diastolic pressure (73.5mmHg±8.5 vs. 72.8mmHg±9.9, respectively p=0.324). Serum concentrations of total cholesterol, LDL-cholesterol, HDL-cholesterol and triglycerides were significantly higher in patients with PBC compared to controls (Table 2, Figs. 1 and 2). Forty-one patients (79%) in the PBC group were receiving pharmacologic treatment consisting of ursodeoxycholic acid.
Demographic characteristics of patients with primary biliary cholangitis (PBC) and controls.
| Patients with PBCx±SD | Controlsx±SD | p | |
|---|---|---|---|
| Age | 52.5±12.9 | 56.0±9.4 | 0.086 |
| Weight (kg) | 61.2±10.7 | 63.3±9.6 | 0.224 |
| Height (cm) | 156.5±7.8 | 157.3±8.3 | 0.551 |
| BMI (kg/m2) | 25.0±4.1 | 25.7±3.5 | 0.261 |
| SAP (mmHg) | 112.9±15.1 | 115.4±11.7 | 0.259 |
| DAP (mmHg) | 72.8±9.9 | 73.5±8.5 | 0.324 |
BMI: body mass index; SAP: systolic arterial pressure; DAP: diastolic arterial pressure.
Student's T test for independent samples.
Significant p value, p<0.05.
Biochemical variables of patients with primary biliary cholangitis (PBC) and controls (without hypolipemiant medication).
| Patients with PBCx±SD | Controlsx±SD | p | |
|---|---|---|---|
| ALT (UI/L) | 130.6±90.0 | 24.8±18.1 | 0.000 |
| AST (UI/L) | 129.4±89.2 | 26.2±11.5 | 0.000 |
| Platelets (μ) | 244.5±96.2 | 253.7±70.7 | 0.540 |
| Eosinophils | 3.0±3.2 | 2.6±7.0 | 0.752 |
| Alkaline phosphatase (UI/L) | 513.4±429.6 | 75.6±21.9 | 0.000 |
| Gammaglutamyl transpeptidase (UI/L) | 394.3±388.1 | ||
| Creatinine (mg/dl) | 0.7±0.2 | 0.8±0.2 | 0.001 |
| Total bilirubin (mg/dl) | 2.8±4.8 | 0.7±0.3 | 0.000 |
| Direct bilirubin (mg/dl) | 1.3±2.5 | 0.09±0.08 | 0.000 |
| Indirect bilirubin (mg/dl) | 1.5±2.4 | 0.6±0.3 | 0.000 |
| INR | 0.9±0.2 | 0.9±0.1 | 0.720 |
| Total cholesterol (mg/dl) | 263.8±123.9 | 199.6±40.0 | 0.000 |
| HDL-cholesterol (mg/dl) | 62.4±36.2 | 47.3±12.3 | 0.000 |
| LDL-cholesterol (mg/dl) | 179.3±114.8 | 126.8±34.7 | 0.000 |
| Triglycerides (mg/dl) | 149.1±59.1 | 126.4±55.4 | 0.020 |
| Hemoglobin (g/dl) | 12.8±2.4 | 14.4±1.3 | 0.000 |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; INR: International Normalization Index; HDL: high density lipoproteins; LDL: low density lipoproteins.
Student's t test for independent samples.
Significant p value, p<0.05.
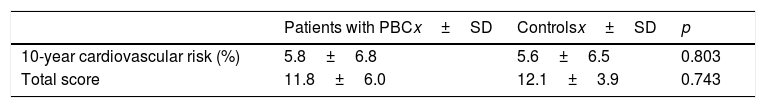
The 10-year cardiovascular risk was 5.8±6.8% in the patients with PBC and 5.6±6.5% in the control group (p=0.803, IC 95%=0.637–1.104, Table 3).
Comparison of cardiovascular risk among patients with primary biliary cholangitis (PBC) and controls without hypolipemiant medication.
| Patients with PBCx±SD | Controlsx±SD | p | |
|---|---|---|---|
| 10-year cardiovascular risk (%) | 5.8±6.8 | 5.6±6.5 | 0.803 |
| Total score | 11.8±6.0 | 12.1±3.9 | 0.743 |
The cardiovascular risk is estimated by a series of parameters including age groups, gender, systolic arterial pressure, total cholesterol, HDL-cholesterol, smoking habit and diagnosis of diabetes mellitus. Validation of the Framingham Coronary Heart Disease Prediction Scores: results of multiple ethnic groups investigation. J Am Med Assoc 2001;286:180–7.
Student's t test for independent samples.
Significant p value, p<0.05.
There were no differences in the cardiovascular risk when only patients or controls with LDL-cholesterol >130mg/dl were analyzed. The 10-year risk for such patients with PBC (n=28) was 7.036±7.06%, and 7.042±7.12% for such controls (n=48) (p=0.92, IC 95% −3.36–3.37). In a mean follow-up time of 57.9 months±36.5 only one cardiovascular event (stroke) was registered in one patient with PBC group, vs. none in the control group (72.17 months+51).
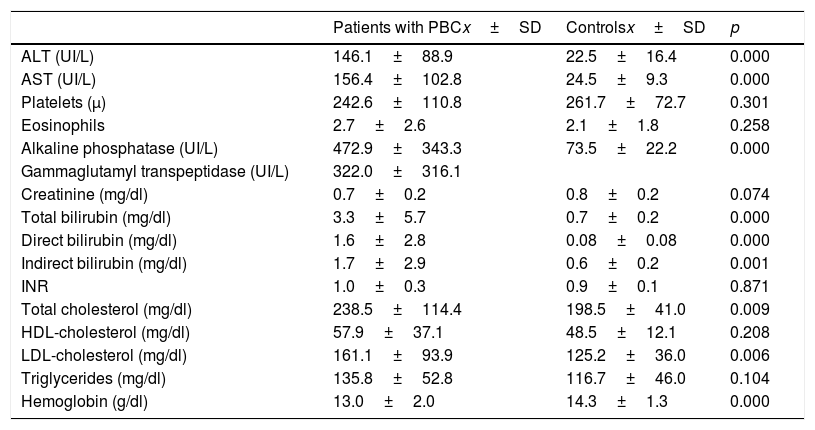
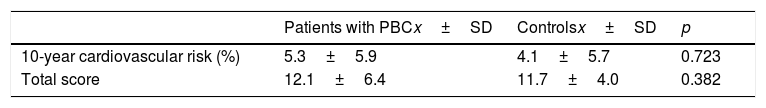
Table 4 describes the biochemical variables of patients and controls who were under hypolipemiant medication. When compared to controls, patients with PBC did not seem to respond to the pharmacological treatment as did the controls (total cholesterol 238.5mg/dl±114.4 in the PBC group vs. 198.5mg/dl±41 in the controls, p=0.009; LDL-cholesterol 161.1±93.9mg/dl in the PBC group vs. 125.2±36.0mg/dl in the control group, p=0.006). No difference in the 10-year cardiovascular risk among both groups was found (5.3±5.9% in patients with PBC vs. 4.1±5.7% in the control group, p=0.723, IC 95%=0.637–1.104; Table 5).
Biochemical variables of patients with primary biliary cholangitis (PBC) and controls (with hypolipemiant medication).
| Patients with PBCx±SD | Controlsx±SD | p | |
|---|---|---|---|
| ALT (UI/L) | 146.1±88.9 | 22.5±16.4 | 0.000 |
| AST (UI/L) | 156.4±102.8 | 24.5±9.3 | 0.000 |
| Platelets (μ) | 242.6±110.8 | 261.7±72.7 | 0.301 |
| Eosinophils | 2.7±2.6 | 2.1±1.8 | 0.258 |
| Alkaline phosphatase (UI/L) | 472.9±343.3 | 73.5±22.2 | 0.000 |
| Gammaglutamyl transpeptidase (UI/L) | 322.0±316.1 | ||
| Creatinine (mg/dl) | 0.7±0.2 | 0.8±0.2 | 0.074 |
| Total bilirubin (mg/dl) | 3.3±5.7 | 0.7±0.2 | 0.000 |
| Direct bilirubin (mg/dl) | 1.6±2.8 | 0.08±0.08 | 0.000 |
| Indirect bilirubin (mg/dl) | 1.7±2.9 | 0.6±0.2 | 0.001 |
| INR | 1.0±0.3 | 0.9±0.1 | 0.871 |
| Total cholesterol (mg/dl) | 238.5±114.4 | 198.5±41.0 | 0.009 |
| HDL-cholesterol (mg/dl) | 57.9±37.1 | 48.5±12.1 | 0.208 |
| LDL-cholesterol (mg/dl) | 161.1±93.9 | 125.2±36.0 | 0.006 |
| Triglycerides (mg/dl) | 135.8±52.8 | 116.7±46.0 | 0.104 |
| Hemoglobin (g/dl) | 13.0±2.0 | 14.3±1.3 | 0.000 |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; INR: International Normalization Index; HDL: high density lipoproteins; LDL: low density lipoproteins.
Student's t test for independent samples.
Significant p value, p<0.05.
Comparison of cardiovascular risk among patients with primary biliary cholangitis (PBC) and controls with hypolipemiant medication.
| Patients with PBCx±SD | Controlsx±SD | p | |
|---|---|---|---|
| 10-year cardiovascular risk (%) | 5.3±5.9 | 4.1±5.7 | 0.723 |
| Total score | 12.1±6.4 | 11.7±4.0 | 0.382 |
The cardiovascular risk is estimated by a series of parameters including age groups, gender, systolic arterial pressure, total cholesterol, HDL-cholesterol, smoking habit and diagnosis of diabetes mellitus. Validation of the Framingham Coronary Heart Disease Prediction Scores: results of multiple ethnic groups investigation. J Am Med Assoc 2001;286:180–7.
Student's t test for independent samples.
Significant p value, p<0.05. IC 95%=0.637–1.104.
In our study we found a marked alteration in the serum lipid profile in PBC patients, mainly due to high LDL-cholesterol, but also a significant elevation in triglycerides and HDL-cholesterol when compared with healthy controls; but the cardiovascular risk and the frequency of cardiovascular events were not different from the healthy population. One explanation is that patients with PBC and extreme hypercholesterolemia have a substantial proportion of circulating LpX. This lipoprotein has a unique high content of unesterified cholesterol and phospholipids and carries apoC. apoE, apoA-I and albumin but is devoid of the structural protein apoB. LpX is not thought to be very atherogenic and may in fact decrease atherosclerotic risk [5]. LpX reduces the atherogenicity of low-density lipoprotein (LDL) cholesterol by preventing LDL oxidation, which suggests that lipoprotein X may protect the integrity of endothelial cells in the presence of hypercholesterolemia [6], such as in PBC patients the time of LDL oxidation induced by copper sulfate is markedly prolonged (>300min) compared with controls and reduces significantly after liver transplantation (100–150min).
Patients with PBC have a significantly lower pulse wave velocity compared to healthy controls, which corresponds to a reduced risk for cardiovascular events [8]. Nonetheless, these patients have serological evidence of endothelial dysfunction, as sICAM, sVCAM and hsCRP are all significantly higher when compared to those of healthy subjects. Therefore, it could be expected that patients with PBC may have an increased cardiovascular risk, and the endothelial dysfunction could be explained by the impairment of micellar formation that prevents absorption of fat soluble antioxidants vitamins, in particular of tocopherol. It has been demonstrated that these patients may have lower serological concentrations of other antioxidant vitamins such as vitamin C and retinol [6]. Therefore, a counterbalance of protective factors and cardiovascular risk factors may be involved in these phenomena, in which protective factors may overcome the risk factors [8]. Nevertheless, due to the nature of our study where mechanisms were not analyzed, the 10-year cardiovascular risk may be enough to confirm the findings of other authors, However, the, potential mechanisms by which PBC patients may be protected against cardiovascular disease should be considered and explored in future research.
Some studies have demonstrated a beneficial effect of statins in reducing total cholesterol, LDL-cholesterol and triglycerides in PBC patients [9]; however, we could not confirm this finding because the serum lipid profile of our patients with PBC did not improve with the hypolipemiant treatment, moreover when compared to that of the controls.
In our study most of the patients were on ursodeoxycholic acid (UDCA) treatment. Some studies suggested that UDCA has lowering lipids properties and this could have a protective effect on cardiovascular events in PBC patients. The efficacy of UDCA in primary type IIa or IIb hypercholesterolemia was studied in a multicenter, randomized, double-blind clinical trial for 24 months; however, UDCA failed to show any significant lowering effect on the total cholesterol or triglycerides when compared to placebo. Therefore, results suggest that UDCA has no intrinsic cholesterol-lowering properties and is not a useful therapy for patients suffering from primary hypercholesterolemia [10].
In conclusion, patients with PBC do not seem to have an increased risk of cardiovascular events. PBC patients do not have an increased cardiovascular risk.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or no-for-profit sectors.
Conflict of interestThe authors have no conflicts of interest to declare.
This article has been written and revised by the authors, no other special collaborations have to be declared.