Gallbladder disease is a highly prevalent disease in western countries as a consequence of several genetic, biochemical, and environmental factors. Females are a high-risk group, and pregnancy increases this risk considerably. In fact, gallbladder diseases are the second most common indication for nonobstetric surgical intervention in pregnancy. In this review, we discuss the most important aspects of gallbladder disease and pregnancy as part of the Symposium on Liver and Pregnancy, co-sponsored by the Mexican Association of Hepatology and the Mexican Association of Gynecologists and Obstetrics.
Gallbladder disease is a highly prevalent disease in western countries as the consequence of several genetic, biochemical, and environmental factors. The most important factor involved in gallstone formation is an increased biliary secretion of cholesterol from the liver, producing cholesterol-supersaturated bile. Subsequently, biliary cholesterol precipitates as cholesterol monohydrate microcrystals, which grow and agglomerate, with the formation of macroscopic stones in the gallbladder.1
The prevalence of gallbladder disease differs in several populations. For example, in the United States, 10%–15% of the adult population has gallstones. In other populations, such as those of Latin-American countries, the prevalence of gallstones is higher, up to 50% in adult women.2 This sex dominance implies some risk in pregnancy. In fact, gallbladder disease is the second most common indication for nonobstetric surgical intervention in pregnancy,3 with 31% attacks of biliary colic in women with gallstones.4 In this review, we discuss the most important aspects of gallbladder disease and pregnancy as part of the Symposium on Liver and Pregnancy, cosponsored by the Mexican Association of Hepatology and the Mexican Association of Gynecologists and Obstetrics.
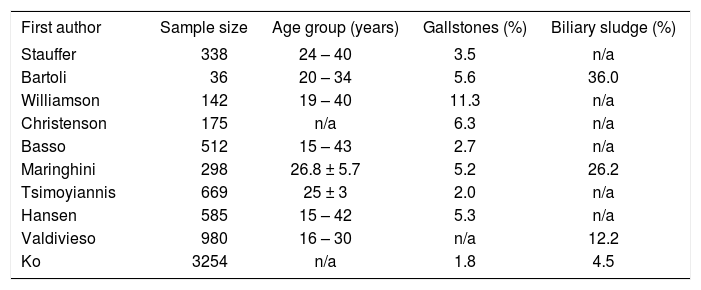
EpidemiologyThe most common causes of gallbladder disease in pregnancy are gallstones and biliary sludge. Pregnancy is associated with an increased frequency of gallstones. Studies in the United States have demonstrated gallstones in 5%-12% of pregnant women.4,5 The risk of gallstones is also thought to increase with the number of pregnancies.6,7 The incidence of gallbladder disease in pregnancy is approximately 0.05%-0.3%,3,8 and asymptomatic gallstones occur in 3.5%-10% of all pregnancies.9 However, the need for cholecystectomy occurs in 1 in 1,600 to 1 in 10,000 pregnancies.10,11
In a study by the University of Southern California, ultrasonography initially revealed biliary sludge in 15% and gallstones in 6% of the pregnant women examined. New sludge or stones were found in 30% and 2% of the women, respectively, at the end of their pregnancies (Table I). Postpartum sonography revealed the disappearance of the sludge in 61% of those women who had previously demonstrated sludge, and the disappearance of stones in 28% of those who had had stones. Therefore, the study concluded that some patients who have symptomatic cholelithiasis during pregnancy may not have it after delivery.12 Unfortunately, about 50% of women presenting with symptoms will have a recurrence of symptoms before delivery.13 However, recent data derived from a German population do not support this hypothesis.14
Review of the prevalence of gallbladder disease during pregnancy detected by ultrasound. Modified from Hansen et al.44
| First author | Sample size | Age group (years) | Gallstones (%) | Biliary sludge (%) |
|---|---|---|---|---|
| Stauffer | 338 | 24 – 40 | 3.5 | n/a |
| Bartoli | 36 | 20 – 34 | 5.6 | 36.0 |
| Williamson | 142 | 19 – 40 | 11.3 | n/a |
| Christenson | 175 | n/a | 6.3 | n/a |
| Basso | 512 | 15 – 43 | 2.7 | n/a |
| Maringhini | 298 | 26.8 ± 5.7 | 5.2 | 26.2 |
| Tsimoyiannis | 669 | 25 ± 3 | 2.0 | n/a |
| Hansen | 585 | 15 – 42 | 5.3 | n/a |
| Valdivieso | 980 | 16 – 30 | n/a | 12.2 |
| Ko | 3254 | n/a | 1.8 | 4.5 |
n/a, not available
Gallstones during pregnancy, especially when complicated by pancreatitis, has traditionally been managed conservatively, with cholecystectomy performed selectively during the postpartum period.6 However, untreated gallstone pancreatitis has an associated maternal mortality rate as high as 37%. The rate of fetal wastage is 38% for fetuses over 20 weeks or 500 g.15
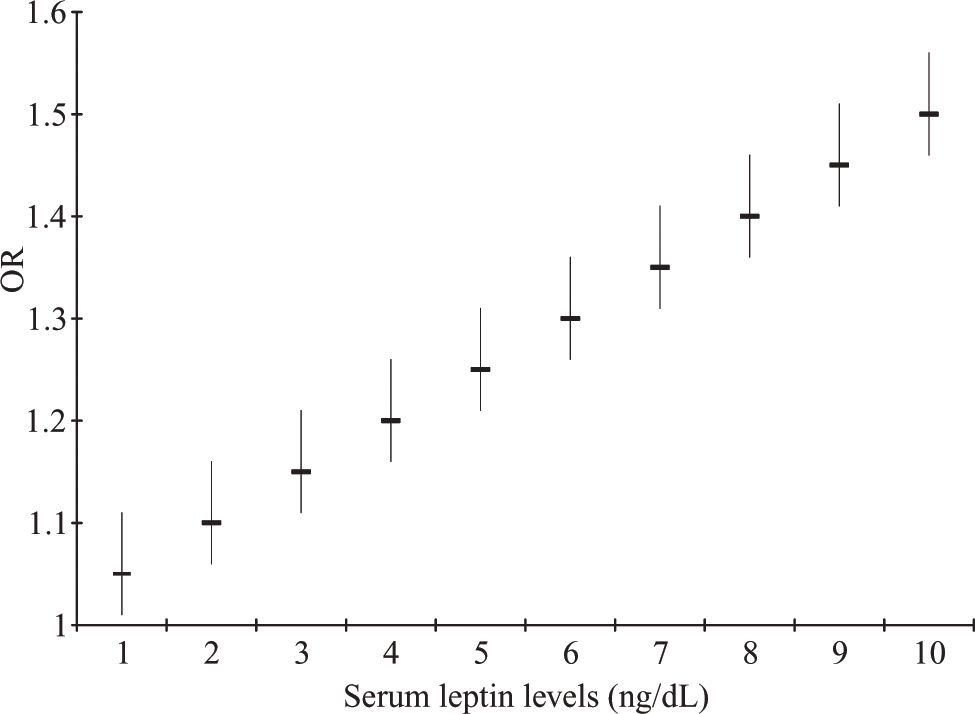
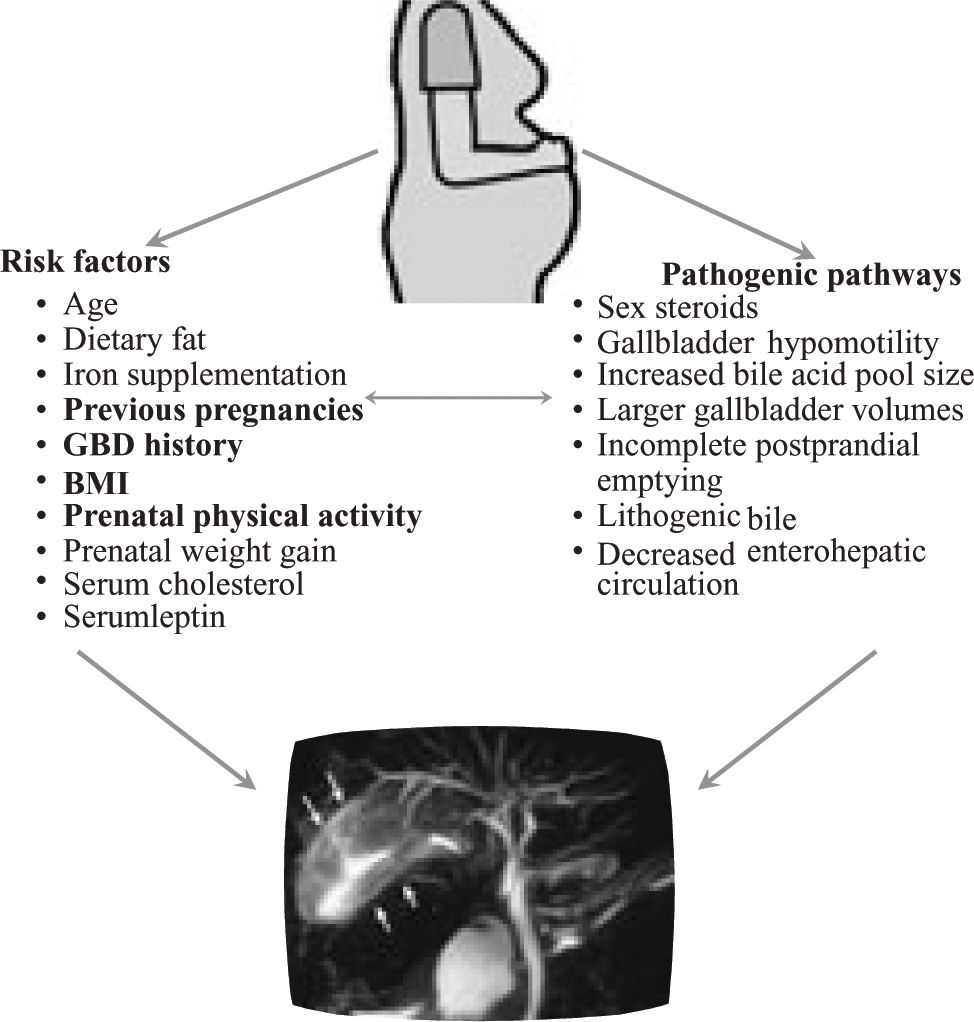
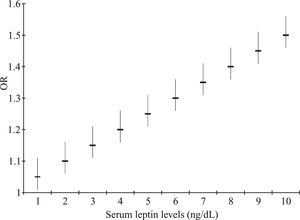
Risk factorsMany risk factors have been associated with gallbladder disease. Probably some of the most important are obesity (and its consequence, the metabolic syndrome),16 diet,17 and some new hormones.18-22 However, in pregnancy, other risk factors have been described, including body mass index, prenatal weight gain, prenatal physical activity, dietary fat, iron supplementation, age, parity, a history of gallbladder disease, and serum cholesterol. In the study by Lindseth et al,23 after multiple regression analyses the most important predictors of cholelithiasis in pregnancy were a history of gallbladder disease, body mass index, and prenatal physical activity. When other variables were evaluated, such as fasting, postprandial gallbladder volume, and the gallbladder ejection fraction, only the gallbladder ejection fraction and the number of previous pregnancies were significant factors related to new gallstones and biliary sludge formation in the pregnant group.24 Recent information from a well-designed prospective study indicates that prepregnancy obesity and serum leptin are strong risk factors for pregnancy-associated gallbladder disease (Figure 1).25
Effects of serum leptin levels as a risk factor (odds ratio) for gallbladder disease (GD) during pregnancy. The risk increases according to each 1 ng/dL leptin. This schematic representation is based on the data of Ko et al.25
Transient changes in the biliary system during pregnancy increase the risk of gallbladder disease. These changes include gallbladder stasis and the secretion of bile with increased amounts of cholesterol and decreased amounts of chenodeoxycholic acid.26 An increase in the lithogenic index of bile is observed in both the hepatic and gallbladder bile, in concert with an increase in cholesterol secretion.
The size of the total bile acid pool also increases by about 50% during pregnancy, although the relative percentages of the various bile acids change. The percentage of cholic acid increases in association with an increase in synthesis, whereas the percentages of chenodeoxycholic acid and deoxycholic acid decrease.27 These changes in the composition of gallbladder bile revert rapidly after delivery, even in patients with gallstones.4 Other changes in bile composition and gallbladder function support gallstone formation during pregnancy, such as the decreased number of enterohepatic cycles.
Sex steroids cause changes in the biliary lipid composition, and gallbladder hypomotility leads to an increase in cholesterol gallstone formation. In vitro models suggest that progesterone inhibits the contractility of the gastrointestinal smooth muscle. In animals pretreated with progesterone, the reduction in the contractile responsiveness to agonists was similar to that seen in pregnant animals.28 Other findings include an enhanced clearance of low-density lipoprotein cholesterol (increased source of the cholesterol secreted in the bile) and the inhibition of acyl coenzyme A: cholesterol acyltransferase.
Fasting and residual gallbladder volumes are larger in pregnant women who are in the second and third trimesters than in the normal population. Incomplete postprandial gallbladder emptying has also been reported in pregnant women (Figure 2).27,29,30
Another mechanism involved in the production of gallstones in the general population is related to apolipoprotein E,31 but apoE4 appears to have little or no association with the development of biliary sludge and/or gallstones in pregnancy.32
DiagnosisThe symptoms of gallbladder disease in pregnancy mimic those in the nonpregnant state. They include the classic colicky or stabbing pain in the right upper quadrant and/or epigastric area, which can radiate to the right flank, scapula, and shoulder. Other symptoms of gallbladder disease include anorexia, nausea, vomiting, dyspepsia, low-grade fever, tachycardia, and often, fatty-food intolerance.33 Differential diagnoses may include viral hepatitis (alcoholic hepatitis is rare in pregnancy), pyelonephritis, duodenal ulcer, acute pancreatitis, pulmonary embolism, acute myocardial infarction, sepsis, and specific pregnancy-related disorders such as preeclampsia, the HELLP (hemolysis, elevated liver function, low platelets) syndrome, and fatty liver disease of pregnancy. Pregnant women who present with acute epigastric pain during pregnancy make diagnosis difficult when they initially present for care, secondary to the displacement of abdominal organs during pregnancy.34
The imaging method of choice in diagnosing gallstones, both in pregnancy and in the nonpregnant state, is ultrasound. Ultrasound is about 95% effective in diagnosing gallbladder disease and avoids radiation exposure altogether.35
ManagementInitial management includes the discontinuation of oral intake, intravenous fluid replacement, analgesia, and the administration of antibiotics when signs of infection are present.36 Patients who fail to respond to medical therapy or who develop recurrent symptoms should undergo cholecystectomy. Early surgery is advocated in these situations to avoid biliary complications and fetal loss, because biliary colic commonly recurs during pregnancy.37 Cholecystectomy should be deferred until the second trimester whenever possible, because of the increased rate of fetal loss when it is performed during the first trimester.38 A study by Lu et al39 demonstrated that women under medical management showed a significantly higher rate of labor induction and preterm delivery (33% vs 0% compared with operative management), caesarean section (9% vs 0%), and relapse before delivery (34% vs 0%). The only adverse effect of surgical treatment was premature contractions (31% vs 28%). Furthermore, nonoperative management of symptomatic cholelithiasis increases the risk of gallstone pancreatitis,12 which causes fetal loss in 10%–20% of cases.7
Laparoscopic cholecystectomy during pregnancy has advantages for the mother in that it speeds her recovery, causes her less pain, and decreases the chance of incisional hernias from large incisions. If a laparotomy incision can be avoided, pain and narcotic administration should be less, and the recovery time is greatly reduced. Thus, postoperative complications due to immobilization, such as deep-vein thrombosis and pulmonary embolism, are less likely. Vaginal delivery without a caesarian section is facilitated, especially in patients who require cholecystectomy later in their pregnancies.40
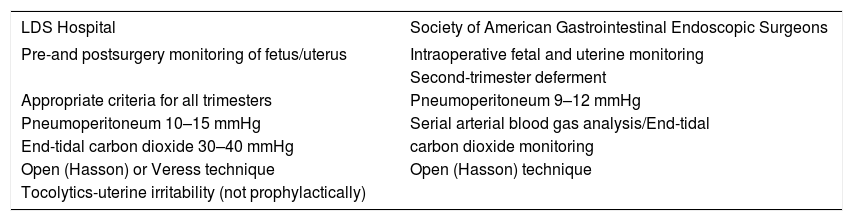
According to a National Institutes for Health statement, patients in the third trimester of pregnancy should generally not undergo laparoscopic cholecystectomy, because there is a risk of damage to the uterus and the large and gravid uterus can obstruct safe access to the abdomen and gallbladder fossa.40 It also suggests that the guidelines for laparoscopy during pregnancy should be revised (Table II).41 In a recent case report, a concurrent caesarean section and laparoscopic cholecystectomy were performed in a woman at 39 weeks’ gestation, but technical expertise necessary and bleeding complications should be considered.42
Comparison of guidelines for laparoscopy during pregnancy. Modified from Rollins et al.41
| LDS Hospital | Society of American Gastrointestinal Endoscopic Surgeons |
|---|---|
| Pre-and postsurgery monitoring of fetus/uterus | Intraoperative fetal and uterine monitoring |
| Second-trimester deferment | |
| Appropriate criteria for all trimesters | Pneumoperitoneum 9–12 mmHg |
| Pneumoperitoneum 10–15 mmHg | Serial arterial blood gas analysis/End-tidal |
| End-tidal carbon dioxide 30–40 mmHg | carbon dioxide monitoring |
| Open (Hasson) or Veress technique | Open (Hasson) technique |
| Tocolytics-uterine irritability (not prophylactically) |
Endoscopic treatment of choledocholithiasis is presently recommended in preference to surgery,40 and several studies have demonstrated that endoscopic retrograde cholangiopancreatography can be successfully and safely performed during pregnancy. Exposure of the fetus to ionizing radiation must be kept to the absolute minimum by the appropriate preprocedure assessments. Consultation with radiologists, who can provide assistance in protecting the fetus and estimating fetal exposure, is also recommended, together with specialized techniques to minimize fluoroscopy time, including the confirmation of biliary cannulation by the aspiration of bile followed by sphincterotomy.43
ConclusionsGallbladder disease is an important issue for the gastroenterologist and hepatologist, particularly its prevention and treatment. These topics require ongoing research. Surgical treatment should be evaluated carefully, and an experienced team consisting of a gastroenterologist, obstetrician, and surgeon should be involved in the management of women with this undesirable effect of pregnancy.