Introduction and aim. Many transplant programs have expanded eligibility to include patients previously ineligible because of advanced age. Outcomes of simultaneous liver-kidney transplantation (SLK) in recipients with advanced age are not known.
Material and methods. Data from patients undergoing transplantation between 2002 and 2015 were obtained from the UNOS Standard Analysis and Research file.
Results. SLK recipients aged ≥ 65 years (N = 677), SLK recipients aged < 65 years (N = 4517), and recipients of liver transplant alone(LTA) aged ≥ 65 years(N = 8495) were compared. Recipient characteristics were similar between the SLK groups. Similar patient and graft survival were observed in SLK recipients aged ≥ 65 years compared to SLK recipients aged < 65 years and LTA recipients aged ≥ 65 years. Importantly, in a subgroup analysis, superior survival was seen in the SLK group aged ≥ 65 years compared to LTA recipients aged ≥ 65 years who underwent dialysis in the week prior to transplantation (p < 0.001). A prediction model of patient survival was developed for the SLK group aged ≥ 65 years with predictors including: age ≥ 70 years (3 points), calculated MELD score (-1 to 2 points), and recipient ventilator status at the time of SLK (4 points). The risk score predicted patient survival, with a significantly inferior survival seen in patients with a score ≥ 4 (p < 0.001).
Conclusions. Age should not be used as a contraindication for SLK transplantation. The validated scoring system provides a guide for patient selection and can be used when evaluating elderly patients for SLK transplantation listing.
Advances in surgical technique and peri-operative care have led to increasing patient and graft survival following liver transplantation (LT). As a result of these improvements, many transplant programs have extended the eligibility criteria for transplant candidates to include patients previously ineligible due to advanced age. While some reports have suggested decreased long-term survival, many single-center reports have demonstrated acceptable outcomes for these patients; and advanced age alone is no longer an absolute contraindication for LT at many centers.1–4 Due to increased acceptance of LT for older patients, the proportion of patients ≥ 65 years of age waitlisted for LT has significantly increased in the past decade from 9.9% (1,637) in 2001 to 16% (2,460) in 2011.5 Similar acceptance of patients with advanced age has been seen with kidney transplantation (KT), where the survival benefit of KT compared to wait-listed patients remaining on dialysis has been shown to extend to elderly patients.6 As LT for patients with advanced age gains broader acceptance, the envelope is pushed even further when deciding how to approach the elderly patient with both end-stage liver disease (ESLD) and significant renal function impairment. Notwithstanding the increasing surgical demands of simultaneous liver-kidney transplantation (SLK), these patients often have multiple medical co-morbidities and varying degrees of frailty.7 This question becomes ever more difficult in the context of the critical organ shortage and maximizing survival benefits for all patients who have both ESLD and end-stage kidney disease.8
To address this question, we sought to investigate the outcomes of SLK in elderly recipients (≥ 65 years of age) using a large national database in the United States. We also aimed to develop and to validate a prediction model using a risk score that could be used when evaluating elderly patients for SLK transplantation. Our secondary goals were to examine the changes in trends of SLK transplantation in elderly patients over time.
Material and MethodsAfter approval from the Mayo Clinic Institutional Review Board, data were obtained and extracted from the United Network of Organ Sharing (UNOS) Standard Analysis and Research file. The study population included all deceased donor LT performed in the United States from February 27, 2002 to March 30, 2015. Elderly patients were defined as those ≥ 65 years of age at the time of transplantation. Comparisons were performed between 3 groups: SLK recipients aged ≥ 65 years, SLK recipients aged < 65 years, and those aged ≥ 65 years receiving liver transplant alone (LTA).
Graft survival was calculated from the time of transplant until death, graft loss, or date of last follow-up. The occurrence and the date of death were obtained from data reported to the Scientific Registry of Transplant Recipients (SRTR) by transplant centers and were completed by data from the US Social Security Administration and from the Organ Procurement Transplant Network (OPTN). Potentially confounding donor and recipient factors were examined, including the liver donor risk index (DRI),9 kidney donor profile index (KDPI),10–11 recipient age, Model for End-Stage Liver Disease (MELD) score at transplant, body mass index (BMI), recipient and donor gender, liver retransplant status, etiology of ESLD, presence of hepatocellular cancer (HCC) as a secondary diagnosis and requirement for dialysis in the week prior to transplantation. DRI is a risk score generated based on liver donor factors correlated with graft survival, while KDPI is a is a remapping of the KDRI (kidney donor risk index) onto a cumulative percentage scale, such that a donor with a KDPI of 80% has higher expected risk of graft failure than 80% of all kidney donors recovered last year. A sub-analysis was performed comparing the SLK group aged ≥ 65 years to patients in the LTA group aged ≥ 65 years who had undergone dialysis in the week prior to transplant.
All statistical analyses were performed using STATA 12 (Stata Corp., College Station, TX). Differences between groups were analyzed using the unpaired t test for continuous variables and by the χ2 test or continuity correction method for categorical variables. Wilcoxon rank-sum was used for variables that did not display a normal distribution. Survival curves for patient or graft survival were generated using the Kaplan-Meier method and compared by the log-rank test. Cox proportional hazard univariate regression for patient survival was performed. All statistical tests were two-sided and differences were considered significant when p < 0.05.
Prognostic scoring Model in SLK group aged ≥ 65 yearsFor patients in the SLK age ≥ 65 group, we developed a prediction model of patient survival. Age categories (65-69 and ≥ 70) were determined a priori based on previous studies.4,6,15 Calculated MELD score was examined per 5 unit increase. Since this scoring system is meant to be used in the evaluation process we omitted donor factors as these would not be available until the time of organ offer. The data were randomly split (50:50) into a derivation and validation data set. In the derivation cohort, univariate and multivariate analysis with backwards stepwise regression were conducted using Cox’s proportional hazard model. A liberal retention criterion of P < 0.15 level of significance during the backward stepwise search was used.12 Regression coefficients (β values) predicting patient survival were determined from the Cox multivariate regression. Points associated with each of the risk factor categories were assigned based on how far each category was from the base category (MELD 5 unit increase) in regression units (βi(Wij- WiREF).13 Patients were then assigned to three risk categories (≤ 0 points; 1-3 points; or ≥ 4 points). The survival outcomes were analyzed using the 3 risk categories in the validation cohort.14
ResultsBetween February 27, 2002 and March 30, 2015, we identified 677 patients undergoing SLK aged ≥ 65 years, 4517 patients undergoing SLK aged < 65 years, and 8,495 patients undergoing LTA aged ≥ 65 years. A trend of both an increasing number of patients aged ≥ 65 years listed for SLK by year and those undergoing SLK transplant by year can be seen in figure 1. Recipient and donor characteristics for the three groups can be seen in tables 1 and 2, respectively.
Recipient characteristics in SLK group aged ≥ 65 years, SLK group aged < 65 years and LTA group aged ≥ 65 years.
| Recipient characteristics | SLK age ≥ 65 N = 677 | SLK age < 65 N = 4,517 | LTA age ≥ 65 N = 8,495 | P1 | P2 |
|---|---|---|---|---|---|
| Age at transplant (years) | 67.3 ± 2.2 | 50.4 ± 12.9 | 67.7 ± 2.6 | < 0.001 | < 0.001 |
| Body mass index | 27.6 ± 5.3 | 26.8 ± 6.0 | 27.8 ± 5.2 | 0.002 | 0.34 |
| Gender (male) | 421 (62.2%) | 2,984 (66.1%) | 5,300 (62.4%) | 0.048 | 0.92 |
| Diagnosis | |||||
| Hepatitis C virus serology | 166 (24.5%) | 1,712 (37.9%) | 2,379 (28%) | < 0.001 | 0.05 |
| EtOH | 101 (14.9%) | 668 (14.8%) | 846 (10.0%) | 0.93 | < 0.001 |
| NASH | 136 (20.1%) | 302 (6.7%) | 884 (10.4%) | < 0.001 | < 0.001 |
| Cholestatic | 42 (6.2%) | 251 (5.6%) | 712 (8.4%) | 0.5 | 0.047 |
| HCC exception | 41 (6.1%) | 187 (4.1%) | 2,858 (33.6%) | 0.02 | < 0.001 |
| Calculated MELD score | 29.2 ± 8.1 | 28.8 ± .6 | 18.9 ± 9.7 | 0.24 | < 0.001 |
| Match MELD score | 30.3 ± 6.7 | 30.3 ± 7.2 | 25 ± 14.1 | 0.99 | < 0.001 |
| Re-transplant | 43 (6.3%) | 639 (14.1%) | 314 (3.7%) | < 0.001 | < 0.001 |
| Days on waitlist | 72 (1-5379) | 65 (1-6734) | 96 (1-5719) | 0.39 | 0.009 |
| (at transplanting center)* | |||||
| Race/ethnicity | |||||
| White | 508 (75.0%) | 2,792 (61.8%) | 6,316 (74.4%) | < 0.001 | 0.69 |
| Black | 57 (8.4%) | 732 (16.2%) | 510 (6.0%) | < 0.001 | 0.01 |
| Other | 102 (15%) | 993 (22%) | 1,669 (19.6%) | < 0.001 | 0.004 |
| Dialysis prior to transplant | 407 (60.1%) | 3,013 (66.7%) | 533 (6.3%) | < 0.001 | <0.001 |
| Days on dialysis*,‡ | 65 (1-4120) | 124 (1-19031) | NA | < 0.001 | NA |
| All diabetes | 310 (45.8%) | 1,616 (35.8%) | 2,756 (32.4%) | < 0.001 | < 0.001 |
| Type I diabetes | 28 (4.1%) | 189 (4.2%) | 206 (2.4%) | 0.95 | 0.007 |
| Peripheral vascular disease | 11 (1.6%) | 92 (2.0%) | NA | 0.47 | NA |
| Mechanical, ventilated or organ | 42 (6.2%) | 309 (6.8%) | 342 (4.0%) | 0.54 | 0.007 |
| perfusion support at transplant | |||||
| Medical condition | |||||
| At home | 372 (54.9%) | 2,588 (57.3%) | 6,388 (75.2%) | 0.41 | < 0.001 |
| In hospital (not ICU) | 177 (26.1%) | 1,098 (24.3%) | 1,266 (14.9%) | 0.3 | < 0.001 |
| In ICU | 127 (18.8%) | 831 (18.4%) | 841 (9.9%) | 0.82 | < 0.001 |
EtOH: alcoholic cirrhosis. NASH: non-alcoholic steatohepatitis. HCC: hepatocellular carcinoma. P1: SLK group aged ≥ 65 years vs. SLK group aged < 65 years comparison. P2: SLK group aged ≥ 65 years vs. LTA group aged ≥ 65 years comparison.
The SLK group aged ≥ 65 had a statistically higher BMI (27.6 ± 5.3 vs. 26.8 ± 6.0, p = 0.002) and were less likely to be men (62% vs. 66% p = 0.048) than patients in the SLK group aged < 65 years. The proportion of patients with a BMI ≤ 20 was 5% in the SLK group aged ≥ 65 years and 11% in the SLK group aged < 65 years (p < 0.001). The proportion of recipients with cholestatic liver disease (6.2 vs. 5.6%; p = 0.5) and alcohol-related liver disease (14.9 vs. 14.8%; p = 0.93) were similar between the groups. Hepatitis C-positive serology (24.5 vs. 37.9%; p < 0.001) was lower in the SLK group aged ≥ 65 years. There was a higher proportion of patients with cirrhosis due to non-alcoholic steatohepatitis (NASH) (20.1 vs. 6.7%; p < 0.001) and HCC (6.1 vs. 4.1%; p = 0.02) in the SLK group aged ≥ 65 years. Both biologic MELD score (29.2 ± 8.1 vs. 28.8 ± 6.0; p = 0.24) and match MELD score (30.3 ± 6.7 vs. 30.3 ± 7.2; p = 0.99) were similar between the two groups. There was a smaller proportion of patients undergoing liver re-transplantation (6.3 vs. 14.1%; p < 0.001) in the SLK group aged ≥ 65 years. A higher proportion of white patients (75 vs. 61.8%; p < 0.001) were seen in the SLK group aged ≥ 65 years compared to the SLK group aged < 65 years. A lower proportion of patients in the SLK group aged ≥ 65 years had dialysis prior to SLK (60.1 vs. 66.7%; p < 0.001), while a higher proportion of patients had diabetes mellitus (DM) (45.8 vs. 35.8%; p < 0.001). Time on dialysis prior to transplant was available for 305 recipients in the SLK group aged ≥ 65 years and for 2,436 recipients in the SLK group aged < 65 years: this was significantly shorter for the SLK group ≥ 65 years (median 65 days vs. 124 days; p < 0.001). No differences in mechanical ventilation status or the location of the patient at the time of transplant (home, hospital, or intensive care unit [ICU]) was seen between the two groups.
Donor characteristics for the study groups can be seen in table 2. Mean donor age was 37.7 ± 15.4 years in the SLK group aged ≥ 65 years and 34.4 ± 15.0 years in the SLK group aged < 65 years group (p < 0.001), while DRI was higher in the SLK group aged ≥ 65 years (1.31 ± 0.31 vs. 1.28 ± 0.29; p = 0.01). Cold ischemic time (CIT), the proportion of donation after cardiac death (DCD) donors, and the share type (local, regional, or national) were similar between the groups. Donor KDPI was significantly higher in the SLK group aged ≥ 65 years (0.42 ± 0.28 vs. 0.38 ± 0.27; p = 0.001).
Donor characteristics in SLK group aged ≥ 65 years, SLK group aged < 65 years and LTA age ≥ 65 groups.
| Donor characteristics | SLK age ≥ 65 N = 677 | SLK age < 65 N = 4517 | LTA age ≥ 65 N = 8495 | P1 | P2 |
|---|---|---|---|---|---|
| Age (years) | 37.7 ± 15.4 | 34.4 ± 15.0 | 44.5 ± 18.0 | < 0.001 | < 0.001 |
| DRI | 1.31 ± 0.31 | 1.28 ± 0.29 | 1.49 ± 0.39 | 0.01 | < 0.001 |
| Cold ischemia time (h) | 6.9 ± 4.1 | 7.0 ± 3.6 | 6.7 ± 3.3 | 0.51 | 0.14 |
| DCD | 24 (3.6%) | 153 (3.4%) | 440 (5.4%) | 0.83 | 0.06 |
| Share Type | |||||
| Local | 557 (82.3%) | 3,706 (82.1%) | 6,108 (71.9%) | 0.88 | < 0.001 |
| Regional | 110 (16.3%) | 706 (15.6%) | 1,855 (21.8%) | 0.68 | < 0.001 |
| National | 10 (1.5%) | 105 (2.3%) | 532 (6.3%) | 0.16 | < 0.001 |
| KDPI | 42% ± 28% | 38% ± 27% | NA0.001 | NA |
DRI: donor risk index. DCD: donation after cardiac death. KDPI: kidney donor profile index. P1: SLK group aged ≥ 65 years vs. SLK group aged < 65 years comparison. P2 SLK group aged ≥ 65 years vs. LTA group aged ≥ 65 years comparison.
Age at transplant was lower in the SLK group aged ≥ 65 years (67.3 ± 2.2 vs. 67.7 ± 2.6; p < 0.001). No difference in BMI or gender was seen between the two groups. The proportion of recipients with an etiology of hepatitis C-positive serology (24.5 vs. 28%; p = 0.05), cholestatic liver disease (6.2 vs. 8.4%; p < 0.001), and HCC as secondary diagnosis (6.1 vs. 33.6%; p < 0.001) were lower, while alcohol-related liver disease (14.9 vs. 10%; p < 0.001) and cirrhosis due to NASH (20.1 vs. 10.4%; p < 0.001) were higher in the SLK group aged ≥ 65 years. Both biologic MELD score (29.2 ± 8.1 vs. 18.9 ± 9.7; p < 0.001) and match MELD score (30.3 ± 6.7 vs. 25 ± 14.1; p < 0.001) were higher in the SLK group aged ≥ 65 years. There was a higher proportion of patients undergoing liver re-transplantation (6.3 vs. 3.7%; p < 0.001) in the SLK group aged ≥ 65 years and a shorter median time on the waitlist (72 days vs. 96 days; p = 0.009). There was no difference in the proportion of white patients (75 vs. 74.4%; p = 0.69); however there was a higher proportion of African-Americans (8.4 vs. 6.0%; p =0.01), and a lower proportion of recipients of other races (15 vs. 19.6%; p = 0.004) seen in the SLK group aged ≥ 65 years compared to the LTA group aged ≥ 65 years. A higher proportion of patients had DM (45.8 vs. 32.4%; p < 0.001), required mechanical ventilation (6.2 vs. 4.0%; p = 0.007), or were in hospital (26.1 vs. 14.9%; p < 0.001) or in the ICU (18.8 vs. 9.9%; p < 0.001) prior to transplant in the SLK group aged ≥ 65 years.
Donor characteristics for the two groups can be seen in table 2. Mean donor age was 37.7 ± 15.4 years for the SLK group aged ≥ 65 years and 44.5 ± 18.0 years in the LTA group aged ≥ 65 years (p < 0.001), while DRI was significantly lower in the SLK group aged ≥ 65 years (1.31 ± 0.31 vs. 1.49 ± 0.39; p < 0.001). Mean KDPI in SLK group aged ≥ 65 years was 42% ± 28% compared to 38% ± 27% in the SLK group aged < 65 years (p = 0.001). Cold ischemic time (CIT) and the proportion of DCD donors were similar between the groups. A higher proportion of donors were of the local share type in the SLK group aged ≥ 65 years (82.3 vs. 71.9%; p < 0.001), while a lower proportion were regional share (16.3 vs. 21.8%; p < 0.001) and national share (1.5 vs. 6.3%; p < 0.001).
SurvivalOverall patient survival can be seen in figure 2. No difference in patient survival was seen between the SLK group aged ≥ 65 years and the SLK group aged < 65 years (p = 0.10) or between the SLK group aged ≥ 65 years and the LTA group aged ≥ 65 years (p = 0.89). Survival was significantly lower for the SLK group aged ≥ 65 years compared to the LTA group aged < 65 years (reference group only) (p < 0.001). Patient survival at 1-, 3- and 5-years was 84%, 74%, and 67% in the SLK group aged ≥ 65 years; 86%, 77% and 70% in the SLK group aged < 65 years, and 84%, 74% and 66% in the LTA group aged ≥ 65 years. Liver graft survival for the groups can be seen in figure 3. No difference in liver graft survival was seen between the SLK group aged ≥ 65 years and SLK group aged < 65 years (p = 0.43) or between the SLK group aged ≥ 65 years and the LTA group aged ≥ 65 years (p = 0.44). Liver graft survival was significantly lower for the SLK group aged ≥ 65 years compared to patients undergoing LTA aged < 65 years (p = 0.03). Liver graft survival at 1-, 3- and 5-years was 83%, 73% and 67% in the SLK group aged ≥ 65 years; 84%, 75% and 69% in the SLK group aged < 65 years, and 82%, 72% and 64% in the LTA group aged ≥ 65 years.
Patient survival in SLK group aged ≥ 65 years, SLK group aged < 65 years and LTA group aged ≥ 65 years. SLK group aged ≥ 65 years vs. SLK group aged < 65 years (p = 0.10); SLK group aged ≥ 65 years vs. LTA group aged ≥ 65 years (p = 0.89); SLK group aged ≥ 65 years vs. LTA group aged < 65years (p < 0.001).
Liver graft survival in SLK group aged ≥ 65 years, SLK group aged < 65 years and LTA group aged ≥ 65 years. SLK group aged ≥ 65 years vs. SLK group aged < 65 years (p = 0.43); SLK group aged ≥ 65 years vs. LTA group aged ≥ 65 years (p = 0.44); SLK group aged ≥ 65 years vs. LTA group aged < 65 years (p = 0.03).
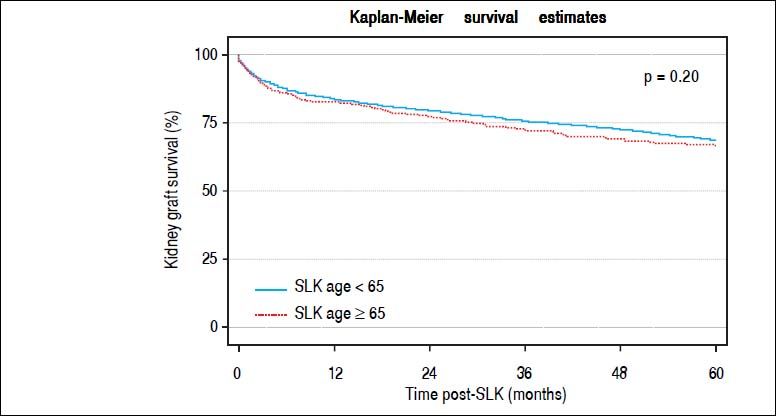
Kidney graft survival can be seen in figure 4. No difference in kidney graft survival was seen between the SLK group aged ≥ 65 years and SLK group aged < 65 years (p = 0.20). Kidney graft survival at 1-, 3- and 5-years was 82%, 72%, and 66% in the SLK group aged ≥ 65 years and 83%, 75%, and 68% in the SLK group aged < 65 years.
A subgroup analysis was performed comparing overall survival in the SLK group aged ≥ 65 years and in LTA recipients aged ≥ 65 years who underwent dialysis in the week prior to transplantation (Figure 5). Superior survival was seen in the SLK group aged ≥ 65 years (p < 0.001).
Prognostic scoring Model in SLK group aged ≥ 65 yearsA Cox univariate analysis predicting survival was performed in the derivation cohort of recipients of SLK who were aged ≥ 65 years (Table 3). All variables were included in a Cox multivariate regression model with backwards stepwise selection, and liberal retention criteria of p < 0.15 was used. Variables retained in the model included: age ≥ 70 years (reference age: 65-69 years; HR 1.4; p = 0.095), calculated MELD score (HR 1.02; p = 0.02), and recipient ventilator status at the time of SLK (HR 1.98; p = 0.006). None of the other variables were significant in the multivariate model. There were 573 patients in the age group 65 -69 and 104 patients in the age group ≥ 70 years. On the basis of the results of the multivariate analysis, points were assigned to the various risk categories (Table 4). Patients were then assigned to three risk category groups (group 1: ≤ 0 points, group 2: 1-3 points, or group 3: ≥ 4 points). Survival curves for the three risk groups in the validation cohort can be seen in figure 6. The risk score predicted patient survival (p = 0.003). A trend of higher patient survival was seen between risk score groups 1 and 2 (p = 0.18). A statistically significant higher survival was seen between risk score group 1 and 3 (p < 0.001) as well as between risk score groups 2 and 3 (p < 0.001). Patient survival at 1-, 3- and 5-years was 90%, 79%, and 73% in group 1; 82%, 70% and 68% in group 2, and 68%, 58% and 45% in group 3.
Cox univariate and multivaraite backwards stepwise analysis predicting patient survival in derivation cohort (N = 338) SLK group aged ≥ 65 years.
| Univariate | Multivariate* | |||
|---|---|---|---|---|
| HR | p value | HR | p value | |
| Age ≥ 70 (reference age 65-69) | 1.58 | 0.08 | 1.60 | 0.07 |
| Body mass index (per 5 unit increase) | 1.05 | 0.54 | ||
| Gender (reference female) | 1.15 | 0.54 | ||
| Diagnosis (reference other) | ||||
| Hepatitis C virus serology | 1.11 | 0.67 | ||
| EtOH | 1.10 | 0.75 | ||
| NASH | 0.94 | 0.82 | ||
| Cholestatic | 0.96 | 0.94 | ||
| HCC Exception | 0.67 | 0.43 | ||
| Calculated MELD score (per 5 unit increase) | 1.20 | 0.04 | 1.15 | 0.1 |
| Dialysis prior to transplant | 1.11 | 0.63 | ||
| Diabetes | 1.06 | 0.78 | ||
| On ventilator at SLK | 2.04 | 0.03 | 1.80 | 0.07 |
| Medical condition (reference at home) | ||||
| In hospital (not ICU) | 0.83 | 0.47 | ||
| In ICU | 1.56 | 0.07 | ||
EtOH: alcoholic cirrhosis. NASH: non-alcoholic steatohepatitis. HCC: hepatocellular carcinoma.
Patient Survival in Recipients of SLK group aged ≥ 65 years based on Risk Score (Test cohort; N = 339). Comparison across all 3 groups (p = 0.003). Risk score group (≤ 0) vs. Risk score group (1-3) (p = 0.18); Risk score group (≤ 0) vs. Risk score group (≥ 4) (p < 0.001); Risk score group (1-3) vs. Risk score group (≥ 4) (p < 0.001).
The data and analyses presented herein demonstrate that in properly selected cases similar patient and graft survival can be achieved in patients aged ≥ 65 years undergoing SLK transplant compared to patients aged < 65 years undergoing SLK and patients aged ≥ 65 years undergoing LTA. In addition, we provide a validated scoring system predicting patient survival that can be used as a guide to help physicians select patients aged ≥ 65 years for SLK.
As a result of improving outcomes in patients undergoing LT, many transplant programs continue to extend the pool of eligible transplant candidates to include patients previously ineligible because of advanced age. In concordance with the overall aging United States population, there has been an increase in the number of patients aged ≥ 65 years listed for LTA from 9.9% (n = 1,637) in 2001 to 16% (n = 2,460) in 2011 (OPTN).5 Moreover, the number of SLK has increased by 200% to 300% in the United States since the implementation of MELD score for liver graft allocation.15,16 It is therefore not surprising that the present study demonstrates a steady increase in the number of patients aged ≥ 65 years listed for and ultimately undergoing SLK between 2002 and 2015. These trends highlight the importance of the goals of this study; namely evaluating outcomes in elderly patients undergoing SLK transplantation and determining prognostic factors in this population to help with patient selection. The data and analyses herein will prove useful as the numbers of elderly patients being evaluated for SLK transplant will likely continue to rise.
While minimal data on SLK in recipients 65 years or older exist in the literature, a number of studies examining LTA in elderly patients have been published.2–4,17 A large study using UNOS data from 2002-2011 demonstrated higher 5-year mortality but lower 5-year death-censored graft failure rates with increasing age after age 55 years.1 Another study comparing recipients older than 70 years with those younger than 60 years demonstrated that older patients were not at an increased risk of death (relative risk, 1.00; 95% confidence interval, 0.43-2.31) or graft loss (relative risk, 1.17; 95% confidence interval, 0.54-2.52).18 It has also been demonstrated that younger, sicker patients a had a higher survival rate than older patients who had poor hepatic synthetic function, high bilirubin levels, or were admitted to the hospital;17 older patients who were less ill also had a higher survival rate compared to this older sicker group. In patients 70 years or older undergoing living donor liver transplant, good results have been observed when patients did not have major medical comorbidities.19 Despite some variability in the results of these studies, all concluded that chronological age alone should not be a deterrent for an otherwise acceptable LT candidate.
There has been very little data published investigating the outcomes of SLK in elderly recipients. A study by Dellon, et al. (2006) demonstrated poor 1-year survival in recipients 65 years or older who underwent SLK in the pre-MELD era (25%) but showed significant improvements in the several years following the introduction of MELD (67%).20 In the present study, we demonstrate 1-, 3- and 5-year patient survival of 84%, 74%, and 67% in the SLK ≥ group 65 years or older. We did not find any differences in patient, liver graft, or kidney graft survival between the SLK group 65 years or older, SLK group younger than 65 years or the LTA group aged 65 years or younger. Therefore these data suggest that age alone should not be considered a contraindication for considering SLK in elderly patients. However, the good outcome data presented in the current study should be critiqued carefully because not all patients aged 65 years or older in need of SLK should be considered appropriate candidates for the procedure. This population may have multiple comorbidities and varying levels of debility, and all of which must be taken into account during evaluation. It is important to note that in the present study, there was no difference in biologic MELD score, rate of peripheral vascular disease, rate of DM, medical condition prior to SLK (home, in hospital, or in ICU), or proportion of patients on mechanical ventilation prior to transplant between patients < 65 and patients ≥ 65 years undergoing SLK. The two study groups, therefore, at least based on these variables, are comparable.
Another aim of the current study was to develop a scoring system that could add objective data to clinical judgment. As a large volume liver and kidney transplant program, we have observed increased number of patients evaluated and presented for SLK in recent years. This fact, in turn, causes a clinical question (which patients are best candidates for SLK?) as well as a societal question (best use of available organs). We feel that these are relevant questions in the era of organ shortage. In addition, a more objective candidate selection system could be very valuable for fulfilling our duty to individual patients and society in general. A scoring system could be used at the time of patient evaluation for transplant and at different time points during the waiting period to determine the suitability of a candidate for SLK. We developed a scoring system using retrospective outcome data in patients aged ≥ 65 years who underwent SLK during the study time period (Table 4). Since this scoring system is meant to be used in the evaluation process of SLK candidate we omitted donor factors, as these would obviously not be available until the time of organ offer. Using this scoring system, patients with a score ≥ 4 had a significantly inferior survival. Based on these findings, SLK should be avoided in the following situations:
- •
Patients ≥ 65 years of age on a mechanical ventilation prior to SLK.
- •
Patients ≥ 70 years of age with a MELD score ≥ 30.
In addition, the best survival was observed in patients with a risk score ≤ 0; encompassing a group of patients 65-69 years of age, with a MELD score ≤ 29 who were not on a ventilator immediately prior to SLK transplant.
When evaluating elderly patients for SLK there is no question there are a multitude of factors not captured in the SRTR data (and hence not in our score) that must be considered. These include but are not limited to cardiac disease, functional status, nutritional status and social support system. The scoring system provided herein is only meant to provide a rough guide to be used in conjunction with all of the above factors as part of a multi-disciplinary evaluation. It is almost certain that recipients ≥ 65 years who underwent SLK transplantation in the present data set are a selected cohort who had favorable evaluation in all of the above based factors that are not captured in the SRTR data. Nonetheless, the results presented in the current study document for the first time that the methods of selection for elderly patients undergoing SLK that are being employed are achieving comparable results to those that are observed with patient < 65 undergoing SLK transplantation.
SLK allocation has recently been debated as concerns about varying practices of listing patients for SLK transplant versus liver transplant alone have been raised.21 Increasing the number of elderly patients undergoing SLK will undoubtedly use a small number of kidney grafts that would otherwise be used for patients undergoing kidney transplant alone. Mechanisms to avoid performing SLK in patients who may ultimately recover renal function have been proposed: a salvage kidney transplant option (in the form of prioritization of kidney allocation) for patients who do not have renal function recovery after LTA. It is likely that a policy with a “safety net” of some type will be adopted in the future to avoid utilization of kidney grafts in patients who ultimately do not need them. There are also allocation issues to be considered when performing an SLK in a patient aged 65 years or older: the updated kidney allocation system has been designed to preferentially allocate lower kidney donor profile index (KDPI) kidney grafts to younger kidney transplant candidates. Recent data has demonstrated that 48.3% of the kidney grafts allocated to SLK recipients had a KDPI less than 35% (21). In the present study, we demonstrate that the mean KDPI was relatively low (42%) in SLK recipients ≥ 65 years of age. While there are still a relatively low number of SLK recipients aged ≥ 65 years, as the population ages in the United States, the number of such patients will continue to rise.
Recently, a study looking into outcomes of patients undergoing LTA after listing for SLK demonstrated inferior survival and a graft loss rate twofold higher in the LTA group when compared to patients undergoing SLK.22 This result is consistent with other analyses comparing LTA and SLK transplant outcomes among dialysis-dependent patients.23,24 In the present study we also demonstrated inferior survival in LTA patients aged ≥ 65 years who underwent dialysis in the week prior to transplantation when compared to recipients in the in the SLK group aged ≥ 65 years by using a subgroup analysis. In light of these findings and the similar survival rates in patients aged ≥ 65 and < 65 years undergoing SLK, it does not seem justified to discriminate against elderly SLK patients despite the small drain it may have on the availability of kidney grafts for the cohort undergoing kidney transplant alone.
Limitations of the present study include its reliance on registry data and lack of granularity. Limited data on pretransplant cardiac disease, frailty, nutritional status and social support are available in the UNOS dataset. Pre-transplant time on dialysis was not available for all patients. In addition the screening protocol of older liver transplant candidates varies among transplant centers, therefore selection bias favoring healthier older adults could have accounted for better outcomes.
In conclusion the present study demonstrates that similar patient and graft survival can be achieved in patients aged ≥ 65 years undergoing SLK compared to patients aged < 65 years undergoing SLK transplant and patients aged ≥ 65 years undergoing LTA. Chronological age alone should not be used as an absolute contraindication for SLK but should be considered in conjunction with other patient attributes. The scoring system created and validated for SLK patients aged ≥ 65 years provides an objective and practical tool to aid decision making when evaluating elderly patients for SLK.
Abbreviations- •
CI: confidence interval.
- •
CIT: cold ischemia time.
- •
CT: computed tomography.
- •
DCD: donation after cardiac death.
- •
DBD: donation after brain death.
- •
DM: diabetes mellitus.
- •
DRI: donor risk index.
- •
HCC: hepatocellular carcinoma.
- •
KDPI: kidney donor profile index.
- •
LDLT: living donor liver transplant.
- •
LT: liver transplant.
- •
LTA: liver transplant alone.
- •
MELD: Model for End Stage Liver Disease.
- •
NASH: non-alcoholic steatohepatitis.
- •
OPTN: Organ Procurement Transplant Network.
- •
SD: standard deviation.
- •
SLK: simultaneous liver/kidney transplantation.
- •
UNOS: United Network for Organ Sharing.
Participated in research design: Kris P. Croome, Justin M. Burns, David D. Lee, Dana K. Perry, Andrew P. Keaveny, C. Burcin Taner.
Participated in the writing of the paper: Kris P. Croome, David D. Lee, Andrew P. Keaveny, Hani M. Wadei, C. Burcin Taner.
Participated in the performance of the research: Kris P. Croome, David D. Lee.
Participated in data analysis: Kris P. Croome, David D. Lee, C. Burcin Taner.
Final Approval: Kris P. Croome, C. Burcin Taner.
DisclosureNone of the authors have any conflict of interest to disclose.
AcknowledgementFunding provided internally by Mayo Clinic Collaborative in Transplant Research and Outcomes.