The prevalence of obesity is increasing globally, with nearly half of a billion of the world’s population now considered to be overweight or obese. Obesity and overweight patients are one of the major health issues in Canada, resulting in approximately 57,000 deaths related to obesity over the last 15 years. The effect of obesity on outcomes following liver transplantation remains largely unclear. To determine the effect of obesity on outcome we reviewed 167 liver transplants, performed at the Vancouver General Hospital, between February 1999 and October 2003. Severe obesity was defined as body mass index (BMI) > 35 kg/m2 and moderate obesity as BMI of 30 – 34 kg/m2. One hundred forty three transplants were performed in patients with a body mass index (BMI) < 30 kg/m2, 14 in patients with a BMI of 30 – 34 kg/m2, and 10 in patients with a BMI > 35 kg/m2. Non-weight related patient demographics were similar between the groups. A very high proportion of Hepatitic C patients (7/10) were observed in the severely obese group. In the early postoperative course severely obese patients had a higher rate of wound infection (20% vs. 4%, p = 0.0001) and wound dehiscence (40% vs. 1.2%, p = 0.0001). Within the first twelve postoperative months severely obese liver transplant recipients had a higher rate of ventral wound herniation (30% vs. 2.8%, p = 0.0001) when compared to obese or non-obese recipients. The one-year graft and patient survival were similar to non-obese patients. An increased BMI in liver transplant recipients in our centre did not increase the risk of early postoperative mortality, but did increase surgical complications, such as wound infection and wound dehis-cence. The 1-year patient and graft survival however was indistinguishable from those of non-obese patients.
Obesity and overweight patients are one of the major health issues in Canada, resulting in approximately 57,000 death related to obesity over the last 15 years.1 Obese patients are not only at an increased risk for several medical problems, they are also at an increased risk for postoperative morbidity and mortality for a range of surgical procedures.2,3 Due to the increasing prevalence of nonalcoholic fatty liver disease (NAFLD), a common complication of obesity, within the westernized world,4,5 NAFLD has become the only indication for liver transplantation that has increased in the United States between 2006 and 2006.6 Two recent US-based studies have shed some light on the impact of obesity on the long-term outcomes in liver transplant recipi-ents.7,8 The most recent study by Leonard et al.8 examined 1,313 patients over a time span of 4 years and concluded that obesity, as observed within their study, does not pose a contraindication to liver transplantation in the absence of other relative contraindications. To the best of our knowledge no comparative study has been published on the experience of obesity on liver transplant outcomes in Canada. Despite the evidence from a large cohort, the weight of the potential transplant recipient is more than often the subject of discussion in the selection committee meeting, due to perceived worse outcomes in this patient group. Thus it becomes a ‘quality assurance’ issue to determine the outcome in specific subgroups of liver transplant recipients and we evaluated the morbidity and mortality in obese patients undergoing liver transplantation using our centre’s database.
Patients and methodsThe study population consisted of 167 consecutive adult liver transplantations performed at the Vancouver General Hospital, between February 1999 and October 2003. BMI at the time of transplant was calculated using the formula: weight in kg/(height in m)2.9 A BMI of 30-34 kg/m2 was considered obese, and a BMI of • • 35 kg/m2 was considered severely obese. Patients were subdivided according to BMI in Groups I, II and III, respectively. Demographic, operative and outcome variables were recorded. Outcomes measured were events requir-ing significant intervention, such as major infections, reoperation, biliary complications, renal failure, hepatic artery thrombosis (HAT), and death. Minimum follow-up was 12 months.
All donor organs were obtained from heart beating donors, perfused in situ, and preserved in University of Wisconsin solution. The mean cold ischemia times ranged from 212 minutes to 1,183 minutes (mean: 543 min).
Our institutional standard induction immunosuppres-sion protocol included 500 mg of methylprednisolone at the time of declamping the hepatic artery, followed by the purine analogue Azathioprine in combination with calcineurin inhibitor or an alternative regiment of myco-phenolate mofetil or an interlukin-2 receptor antagonist in selected individual cases. Maintenance immunosup-pression was achieved with a combination of low dose corticosteroids, azathioprine and calcineurin inhibitor in the majority of cases.
Statistical analysis. The statistical analysis was conducted using the computer program SPSS 11.0 (Chicago, IL). The chi-square test was used to compare group dependent variables with a statistical significance at a p value less than 0.05.
ResultsOne hundred forty three transplants were performed in patients with a body mass index (BMI) < 30 kg/m2 (Group I), 14 in patients with a BMI of 30 – 34 kg/m2 (Group II), and 10 in patients with a BMI > 35 kg/m2 (Group III).
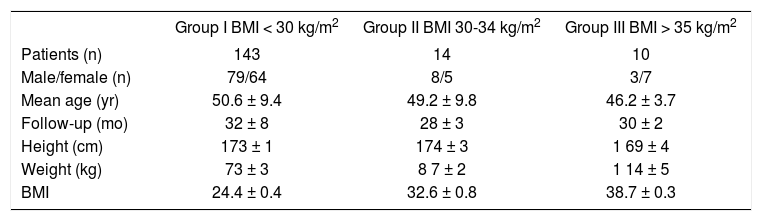
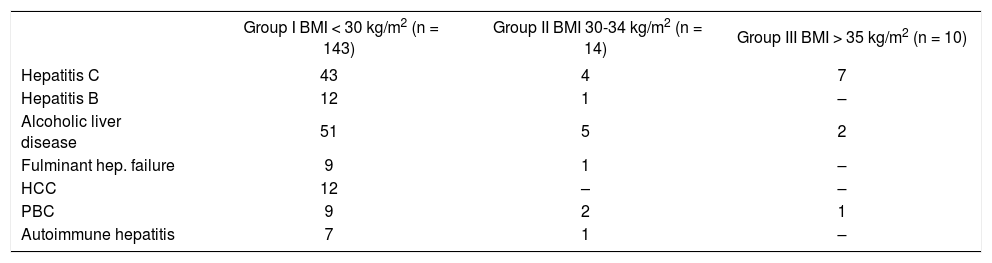
As seen in Table I the mean age was between 42.6 to 60.0 years. The proportion of females was higher in the overweight group (55%) compared with the group III (70%). Primary causes of end-stage liver disease are shown in Table II The most common indications for transplant were alcohol-related disease (primary and secondary, eg. mixed alcohol and hepatitis C). Chronic hepatitis C and hepatocellular carcinoma. A very high proportion of Hepatitic C patients (70%) were observed in the severely obese group.
Patient Demographics stratified by BMI.
| Group I BMI < 30 kg/m2 | Group II BMI 30-34 kg/m2 | Group III BMI > 35 kg/m2 | |
|---|---|---|---|
| Patients (n) | 143 | 14 | 10 |
| Male/female (n) | 79/64 | 8/5 | 3/7 |
| Mean age (yr) | 50.6 ± 9.4 | 49.2 ± 9.8 | 46.2 ± 3.7 |
| Follow-up (mo) | 32 ± 8 | 28 ± 3 | 30 ± 2 |
| Height (cm) | 173 ± 1 | 174 ± 3 | 1 69 ± 4 |
| Weight (kg) | 73 ± 3 | 8 7 ± 2 | 1 14 ± 5 |
| BMI | 24.4 ± 0.4 | 32.6 ± 0.8 | 38.7 ± 0.3 |
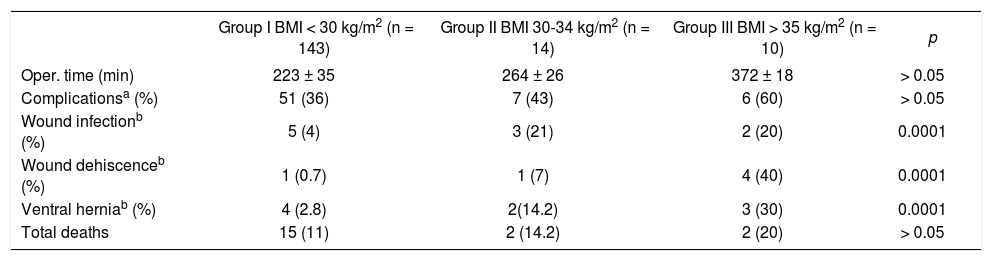
Table III gives data for operative time and post-operative variables. Outcome analysis displayed a significantly higher wound infection rate (20% vs. 4%, p = 0.0001) and wound dehiscence (40% vs. 1.2%, p = 0.0001) among severely obese patients, leading to a marginal higher overall complication rate. Within the first twelve postoperative months severely obese liver transplant recipients had a higher rate of ventral wound herniation (30% vs. 2.8%, p = 0.0001) when compared to obese or non-obese recipients. Graft survival and patient survival in the total cohort and those with a 1-yr follow-up were similar between groups. Early death from multisystem organ failure was more common in the severely obese group, though neither death prior to hospital discharge following transplantation nor death from other causes was different when compared to obese and non-obese patients.
Patient outcome stratified by BMI.
| Group I BMI < 30 kg/m2 (n = 143) | Group II BMI 30-34 kg/m2 (n = 14) | Group III BMI > 35 kg/m2 (n = 10) | p | |
|---|---|---|---|---|
| Oper. time (min) | 223 ± 35 | 264 ± 26 | 372 ± 18 | > 0.05 |
| Complicationsa (%) | 51 (36) | 7 (43) | 6 (60) | > 0.05 |
| Wound infectionb (%) | 5 (4) | 3 (21) | 2 (20) | 0.0001 |
| Wound dehiscenceb (%) | 1 (0.7) | 1 (7) | 4 (40) | 0.0001 |
| Ventral herniab (%) | 4 (2.8) | 2(14.2) | 3 (30) | 0.0001 |
| Total deaths | 15 (11) | 2 (14.2) | 2 (20) | > 0.05 |
Selection of liver transplant recipients is a very difficult task given the great number of patients with end-stage liver disease seeking a liver transplant and the relatively few organs available. Decisions must be made on the basis of “the best available medical evidence”, unfortunately the selection committee of any liver transplant program may not be able to find adequate data from the literature to predict outcomes of liver transplant recipient, based on age, underlying disease, concomitant associated illnesses, in every specific clinical situation. It is therefore an on-going and important process for every program to assess and review clinical variables within their own centre especially if the published experience is sparse. This is a dynamic situation as with changing patient demographics, new variables emerge that might influence the selection process. The international epidemic of obesity will clearly impact on liver transplant programs and may force them to consider the weight and BMI of liver transplant recipients with regards to outcomes. Our experience suggests that the rate of surgical wound complications is significantly higher in those with a BMI greater than 30 kg/m2 compared to those with a BMI less 30 kg/m2. The overall mortality, however, was not significantly different. Based on our experience, a greater morbidity with obese patients can be expected but whether severe obesity might pose a relative contraindication for undergoing a major surgical procedure awaits further study. Regardless, it is clear that physicians who follow patients with cirrhosis must make a determined effort to encourage them to avoid obesity well before a liver transplant situation arises. Although we did not explore this aspect of liver transplantation and obesity, the perception and belief of the physicians and sur-geons associated with our transplant program is that it is extremely difficult to have obese patients with end-stage decompensated cirrhosis successfully lose weight during the pre-transplant period.
With respect to obesity and post-transplant outcomes, the available literature is relatively sparse. A couple multi centered and prospective trials7,8 from the United States have asked this question before and answered it in a favorable manner for obese liver transplant patients, as well as some smaller studies.10,11 We aimed at answering the question of outcome differences between obese and non-obese patients in a Canadian population, as the American experience may not necessarily be generalizable to all nations. We can conclude, however, that, as others have observed, the incidence of morbidity is increased, however mortality outcomes following liver transplantation for selected patients with severe obesity are similar to non-obese recipients. These patients, however, must be carefully monitored for potential postoperative complications such as wound dehiscence and infection.