Introduction
There is an obligatory system for notifying professional diseases,1 defined according to current regulations2 as a disease contracted as a result of work and recorded in the corresponding professional disease chart. The new professional diseases chart of 2006,3 which updates the previous one,4,5 includes 6 sections related to occupational risks (chemical, physical and biological contaminants, and situations of exposure to physical workloads) and the list of occupations or work tasks that can be a cause of these diseases.
An important novelty of the new notification system of professional diseases is that it considers doctors of the National Health System as potential notifiers in the register. Indeed, as explicitly established in the guidelines, when doctors of the National Health System, whilst carrying out their professional duties, are aware of the existence of a disease which is included in the aforementioned table, they must notify it through the competent authority of each autonomous community to the management or collaborating unit of the Social Security responsible for the protection of the professional needs of the worker affected.
Many experts believe that this collaboration could play a decisive role in increasing the capacity of highlighting work related health problems, to a large extent ignored beyond the injuries and death due to work accidents.
In a recent review6 it was observed that total deaths caused by occupational diseases could be, according to estimates in other countries, between 5 and 20 times higher than mortality due to work accidents.
In a previous study,7 applying the risks attributable to deaths due to occupational diseases calculated by Finnish investigators,8 we estimated that in 2005 there were 16 000 deaths caused by occupational exposure in Spain, mainly tumours (more than 9000 deaths) and cardiovascular diseases (around 3600). The objective of this paper is to estimate the impact of occupational diseases in Spain, in terms of their incidence and prevalence, in order to compare them with the notifications actually made.
Methods
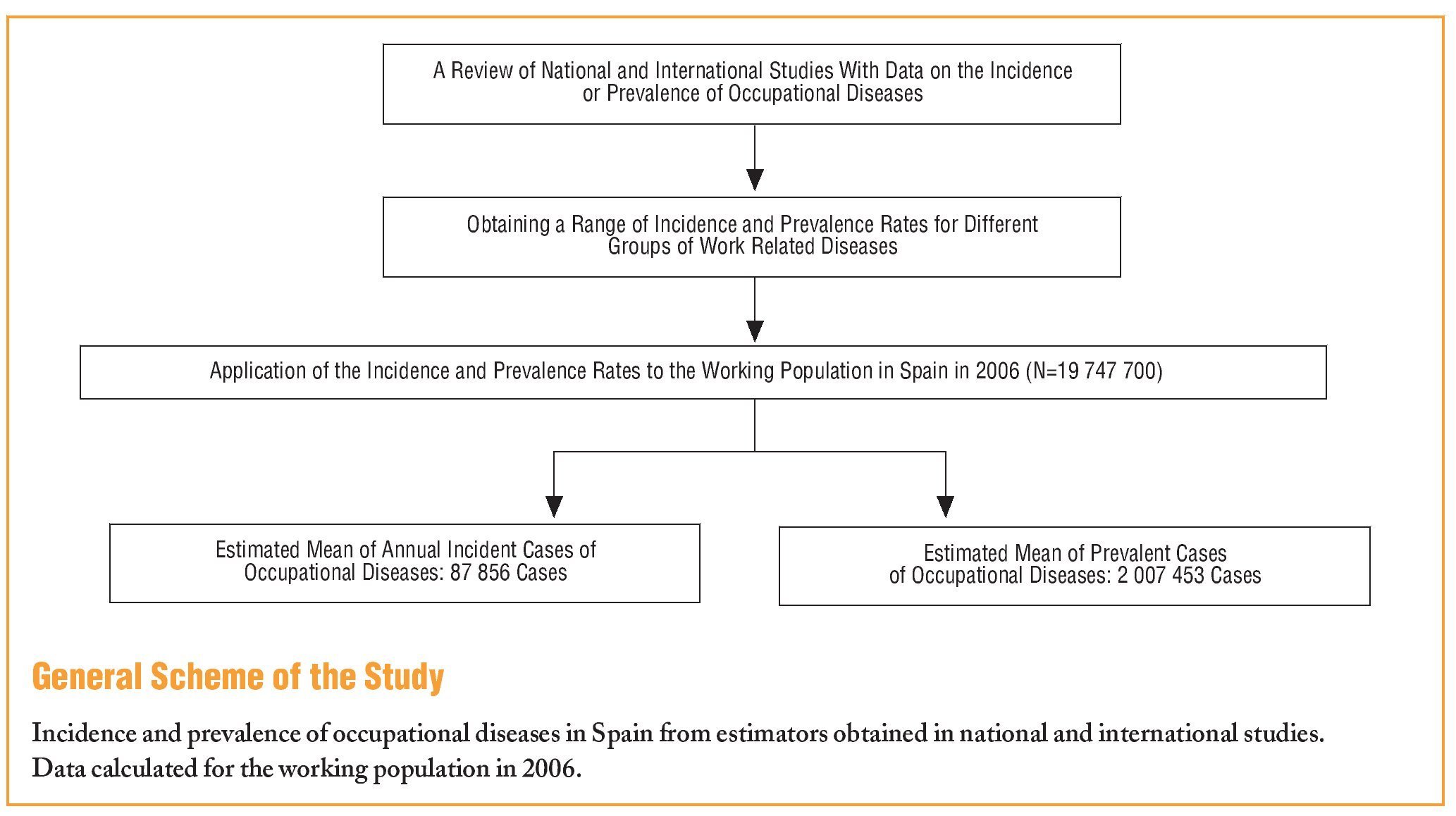
Estimations of Incidence
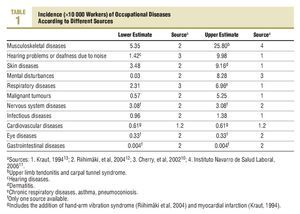
A search was made of the papers in the scientific literature that presented data on the incidence of occupational diseases in the working population. A large part of the studies found were based on voluntary sentinel events of occupational origin notification systems, the British system called THOR (The Health and Occupation Reporting Network), being one of the most experienced and complete.9 This system includes a series of programs aimed at the notification of different types of diseases (respiratory, dermatological, musculoskeletal, infections, psychiatric, etc), and the doctors are voluntary notifier specialists in each of the corresponding areas.10
On the other hand, one of the most common and better established sentinel occupational diseases notification systems in our country is the Programa de Vigilancia Epidemiológica en Salud Laboral (Epidemiological Vigilance in Occupational Health Program (Occupational Health Medical Sentinel Network) of the Navarre Institute of Occupational Health.11 The doctors from the primary care centres participate in this system, with a coverage of about 75% of the Navarre working population.
The Finnish occupational diseases register, recognised as one of the most complete and reliable in the world, also enables the incidences for a series of occupational diseases to be calculated.12
Lastly, some years ago one of the few studies, actually Canadian, that estimated the incidence of a wide group of occupational diseases for a general population, was published.13 The author calculated the incidence rates of occupational diseases in Canada, which was based, on the compensation for occupational diseases statistics in Canada, data from a voluntary notification system of occupational diseases, and on the data on the incidence of some groups of principal diseases available in previous epidemiological studies.
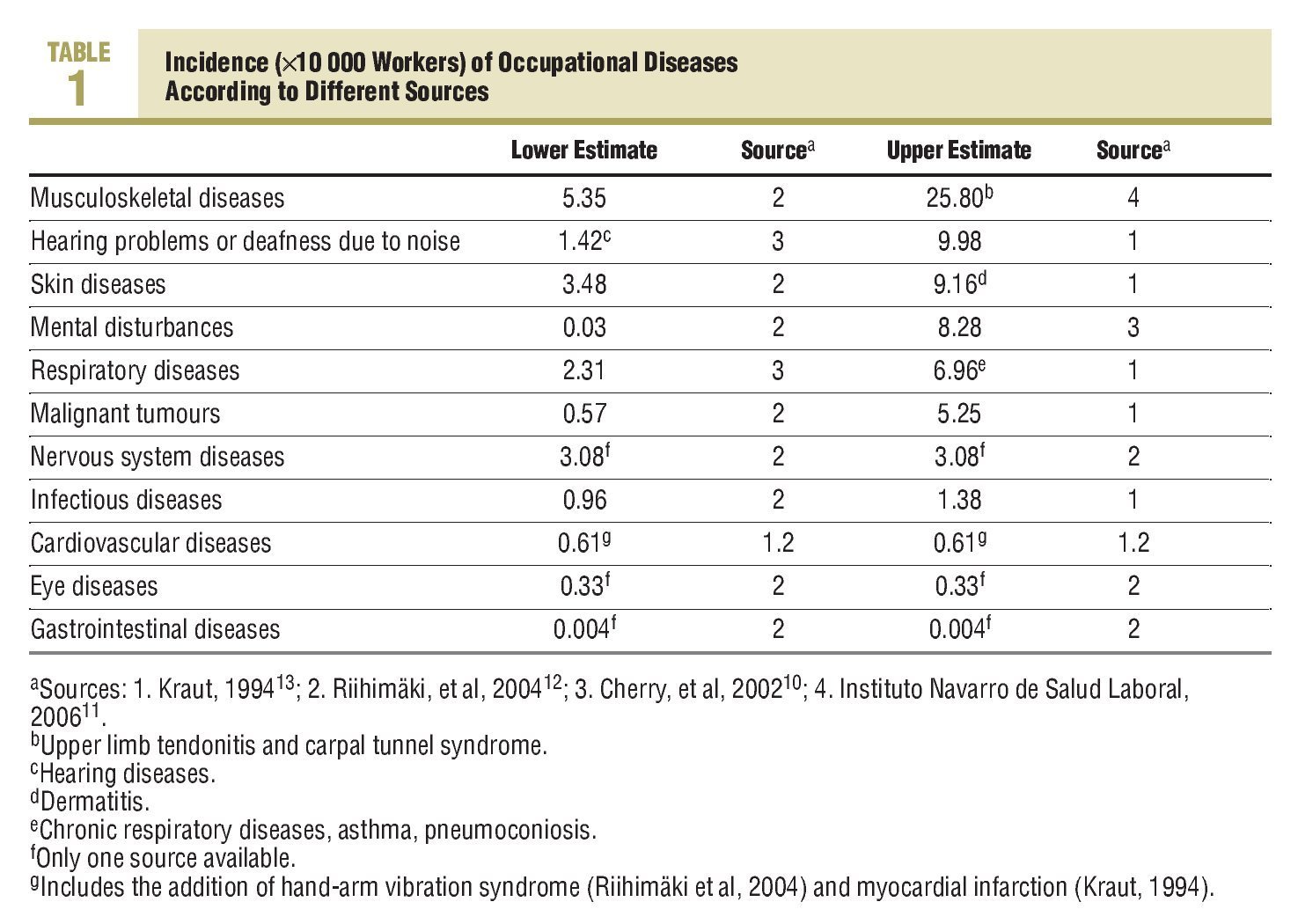
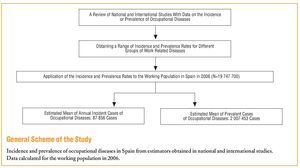
With the information available in these 4 sources,10-13 we have constructed a range of incidences for different categories of large groups of occupational diseases, as presented in Table 1. The number of incident cases of occupational diseases occurring in Spain for each disease group has been calculated, applying these incidences to the mean population working in Spain in 2006.14
Estimations of Prevalence
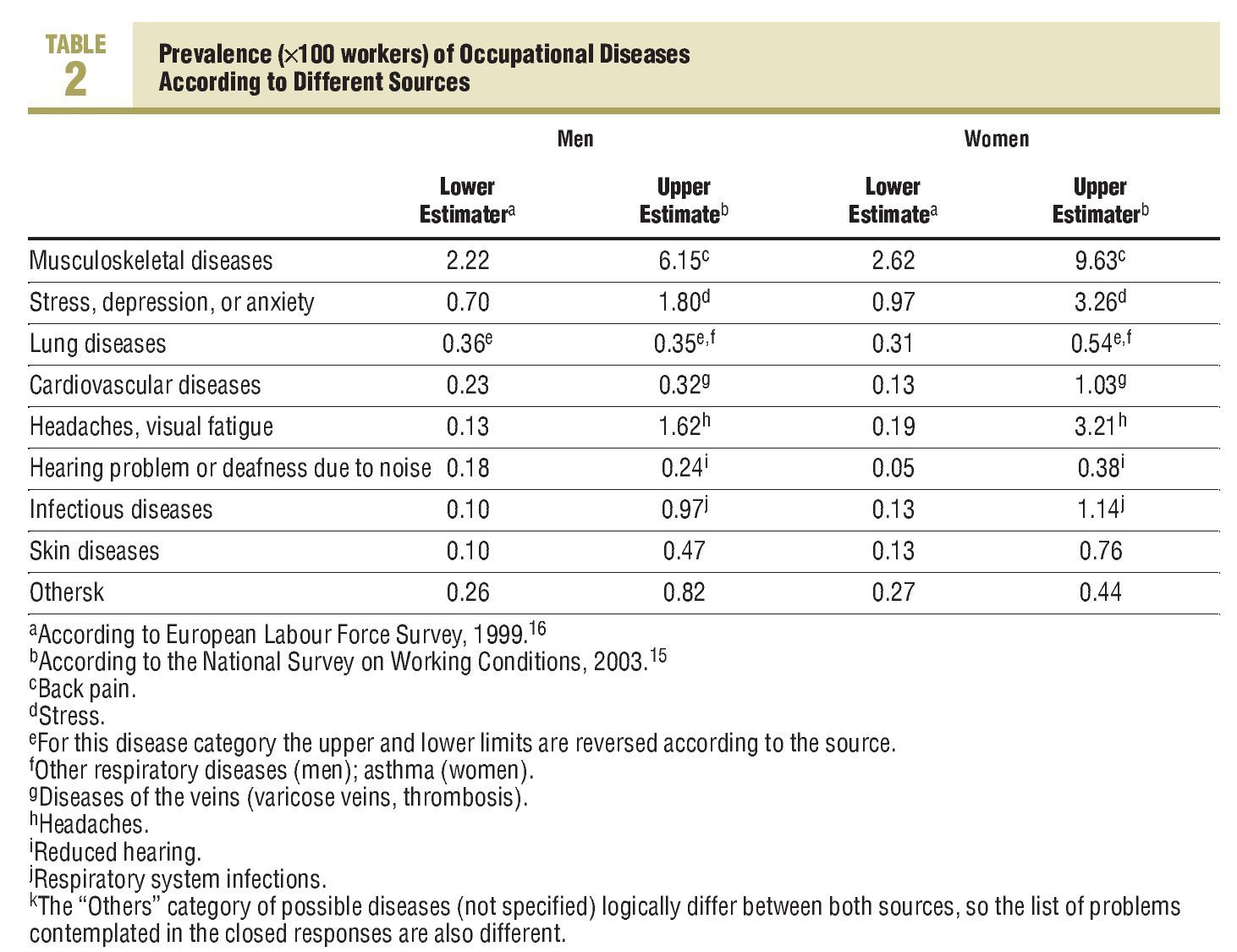
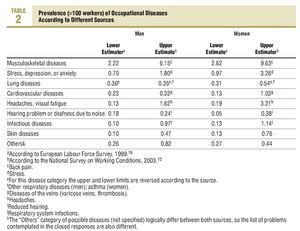
The estimations of the prevalence of occupational diseases have been based on information recorded in 2 sources: the V National Survey of Working Conditions (VENCT) from Spain and the European Labour Force Survey (LFS) from 1999. The ENCT is carried out periodically on a representative sample of the working population in Spain. In the fifth ENCT of 2003,15 questions on a series of symptoms and health problems suffered by the workers were included, asking them whether these processes they identified were related to exposures occurring during work. For its part, the LFS of 1999,16 carried out on representative samples of workers from different European countries, also introduced a series of questions on health problems related to work. For the calculation of prevalent cases of occupational diseases occurring in Spain, the prevalences estimated in these 2 sources for different disease groups (Table 2) have been applied to the mean population working in Spain in 2006.14
Results
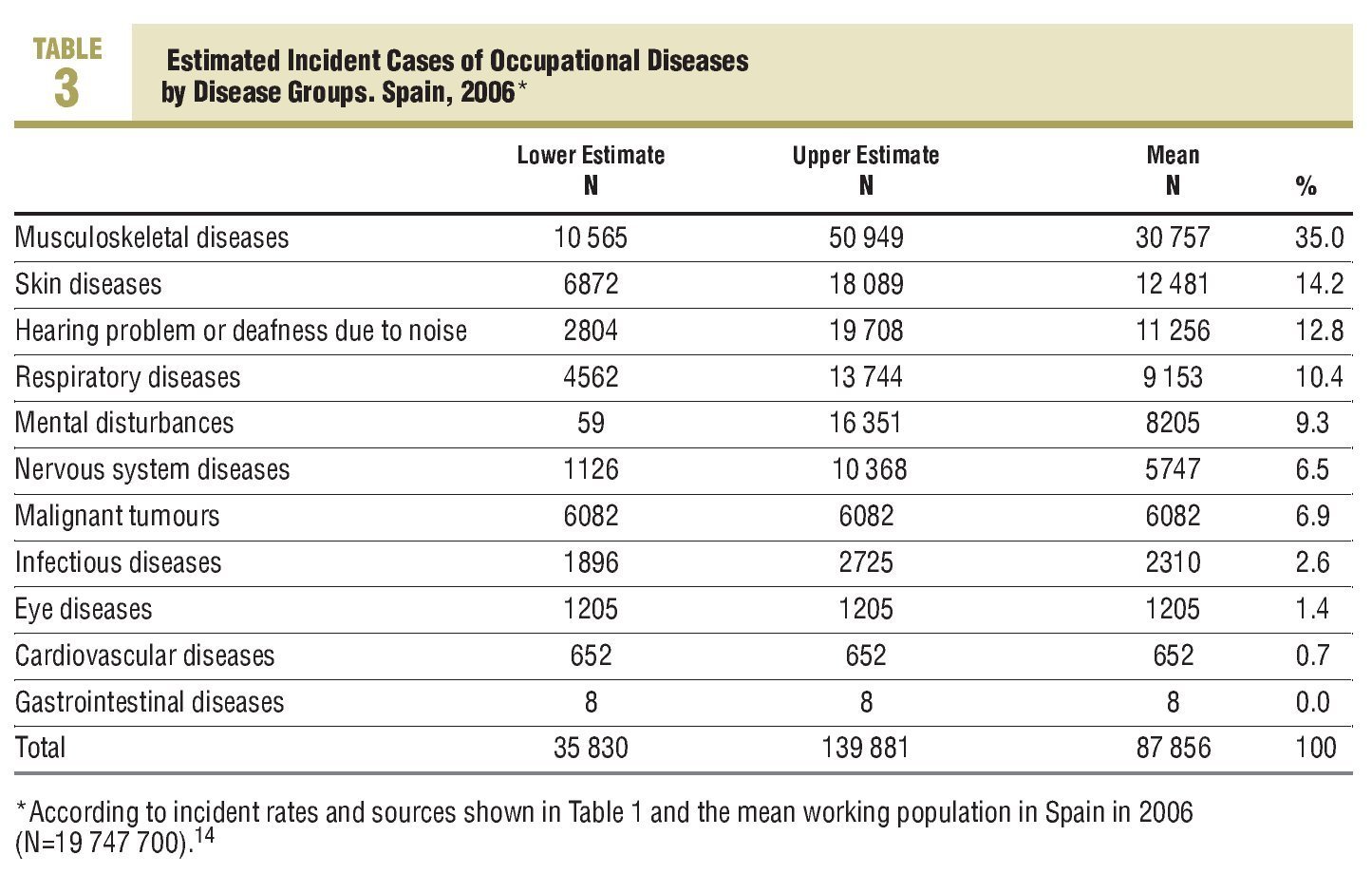
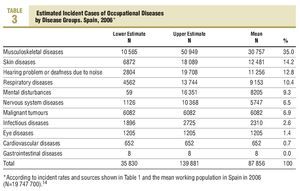
The estimations of incident cases of occupational diseases in Spain in the year 2006 are shown in Table 3. The range (according to lower and upper estimations, Table 1) and the mean are included in the Table. Overall, we can estimate that a mean of around 90 000 new work related diseases occur each year. By order of frequency, the greatest number of incident cases would occur in the musculoskeletal group of diseases, followed by skin diseases and loss of hearing due to noise. The respiratory diseases and mental disturbances of work origin also have notable incidences.
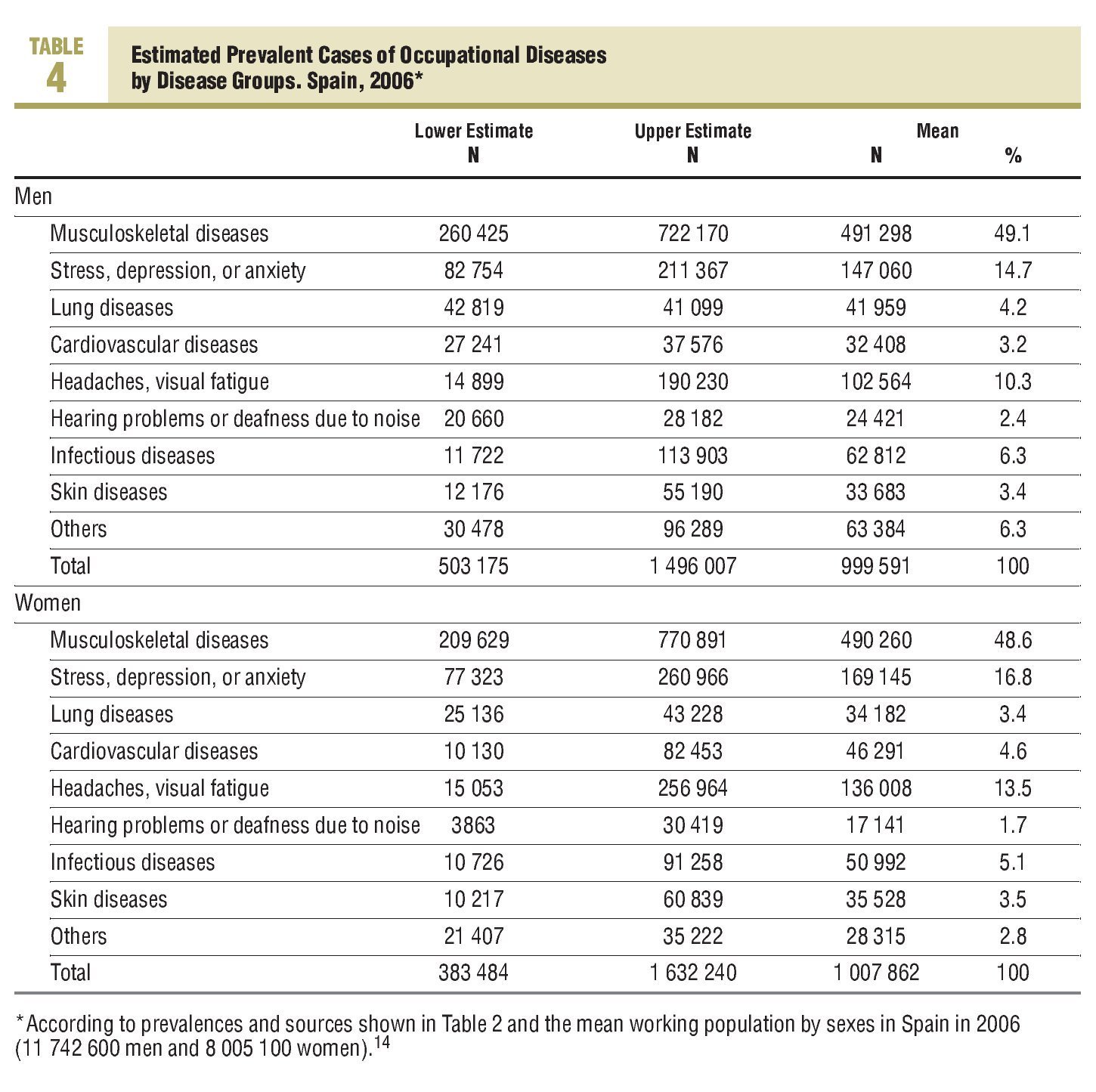
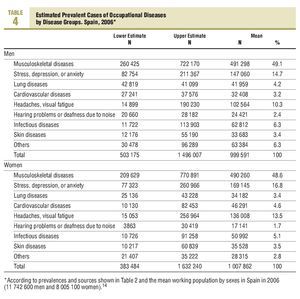
For its part, the estimation of prevalent cases of work-related diseases for both sexes is shown in Table 4. According to the mean estimations, around 1 million workers and a similar figure of workers annually suffer diseases and health problems associated with their work.
Practically half of these problems, both in men and women, are musculoskeletal diseases. The next category in frequency in males are problems with psychological well-being (stress, anxiety, depression), also second in importance and somewhat more common in women.
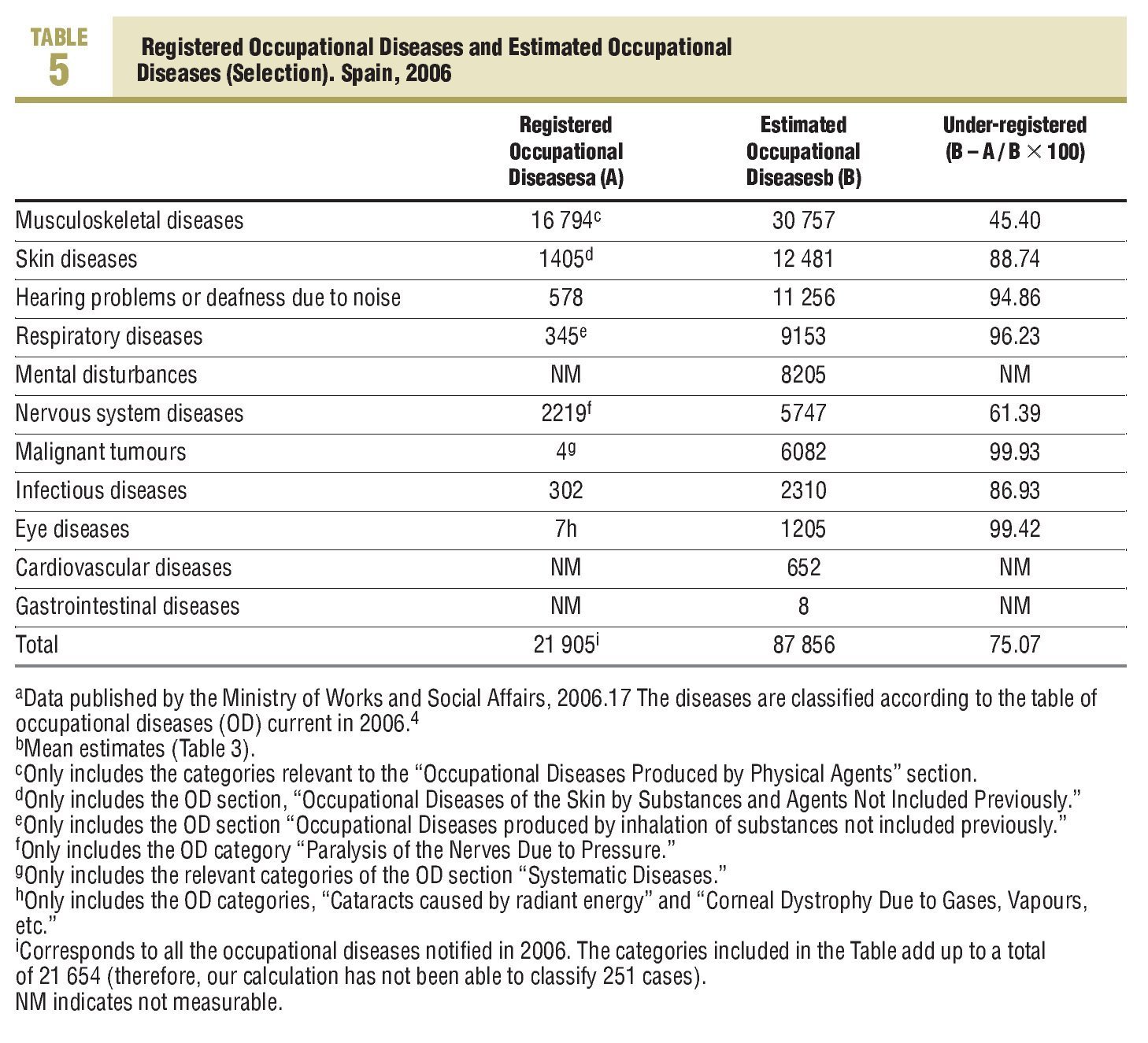
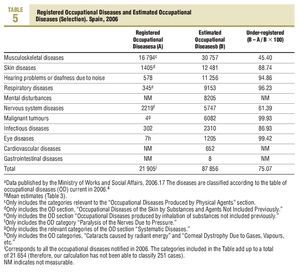
Lastly, in Table 5, the under-registration of occupational diseases is calculated from the comparison of our mean incidence estimations with the data from the official statistics from the Ministry of Work and Social Affairs.17 As can be seen in the Table, the mean under-registration of occupational disease incidents in the year 2006 would be 75%. By disease categories, the lack of knowledge of well recognised occupational problems, such as deafness caused by noise, should be noted.
The under-registration of some more serious diseases, such as malignant tumours or cardiovascular diseases is also worth mentioning.
Discusión
According to our estimations, around 90 000 incident cases of diseases due to occupational exposure are diagnosed annually. Also, around 2 million workers suffer from some health disorder related to their working conditions. Practically 3 out of every 4 cases may not be recognised as an occupational disease and this under-recording may mainly affect the more serious diseases group. In fact, 99.8% (N=21 865) of all the occupational diseases recognised in Spain in the year of the study were described as mild or not involving sick leave.17 Only 40 serious cases of occupational diseases were recognised in the whole of Spain in 2006, and none were fatal.
It is essential to know the impact and distribution of work-related diseases to adequately plan the necessary preventive and healthcare strategies to minimise the dangers of work on health.18
The deficiencies of the official notification system, a unique systematic monitoring source in this sense, are generally recognised by all the experts in occupational health.19
The compensatory character of the system, rather than being a public health monitor, the limitations on being based on a closed list of diseases, despite its recent update,3,5 and some unidentified problems in the notification circuit, which probably might explain the unusual decrease in the number of occupational diseases notified since the new regulations20 came into force, are at the root of these deficiencies.
The calculations made in this work are not without limitations. Except in 2 cases (the Sentinel Occupational Diseases Monitoring System of the Navarre Occupational Health Institute and the National Survey on Working Conditions), the rest of the sources used come from observations and estimations made for populations of other countries. However, in general, they may be considered as comparable environments to Spanish ones, possibly even better as regards working conditions. Some basic indicators (eg, occupational risk) are clearly worse in Spain compared with Finland or the Europe-15 group,21 where some of the sources used come from.12,16 On the other hand the British and Navarre registers have limitations both in spectrum of diseases covered, as well as regards the voluntary nature of the notification system.9-11 The fact is that one of the principal sources for incidence estimation, the Canadian study,13 on the other hand, on being based on information available in 1989, may have introduced distortions in the estimations, since exposure situations to occupational risks may very likely change with time. Another point to consider is the variability in the estimators used to calculate the incidence and prevalence data for different diseases. For example, the estimated incidence for occupational musculoskeletal diseases is 5 times higher in the Canadian study13 when compared to the data of the Finnish register.12
This dispersion may be partly due to real differences in the incidence of the diseases in the different countries, but we also believe that it mainly shows the difficulties in recognising the multiple causes and largely non-specific occupational diseases. In the present article we have adopted a conservative approach by mainly using mean estimations. Well planned follow-up studies would be needed, which should include representative working populations in our country, to be able to make more precise estimations. Despite all these limitations, the overall assessment of the different sources of error that could have affected the results presented in this study, suggest to us that our estimations more likely undervalue the real dimension of the problem. The occupational health medical sentinel networks, as promoted by the Navarre Occupational Health Institute, have shown the frequency with which occupational diseases (such as upper limb tendonitis, carpal tunnel syndrome, asthma, or occupational dermatoses), are dealt with by the Public Health System, without being recognised as occupational diseases.22 Some authors have estimated that 16% of the problems seen in primary care centres are probably related to working conditions.23 The new regulations on occupational diseases allows doctors in the health system to take part in recognising occupational diseases, somewhat necessary to adequately treat and prevent these processes. However, to put this function into operation will not be an easy task. Firstly, training in occupational health of doctors in general medicine as well as those in the different specialities (with the logical exception of occupational medicine) is completely insufficient.24 It would also require the development of support structures by the Health Administration which would make it easier for doctors to carry out the functions of recognising and notifying cases, as well as occupational health units which function in some autonomous communities, but not in all, and not always with the appropriate functions.25
All in all, the recognition of the work origin of a large part of the diseases seen in the Public Health System is absolutely necessary, due to its implications in terms of derived costs and compensation, and the rights of the workers, as well as to implement suitable preventive measures. In this sense, primary care doctors should play a fundamental role, always having the necessary support and resources. We believe that it would be a very positive step to open a debate as regards the opportunities and obstacles to approach this task, and that journals, such as ATENCION PRIMARIA, would be a very valuable forum to channel and communicate the different opinions on this matter.
For the time being, with the present article, we hope we have contributed to highlight the importance and impact of work related health problems in Spain and it leads to the steps necessary to improve the current situation.
What Is Known About the Subject
•In the workplace there are exposures that produce risk factors which can lead to health and wellbeing problems for the workers.
•The system for registering occupational diseases in Spain, despite its recent update, is recognisably limited for evaluating the frequency and characteristics of occupational diseases in our country.
What This Study Contributes
•It has been estimated that in the year 2006 in Spain there were around 90 000 incident cases of occupational diseases.
•Approximately 2 million workers have some health problem related to their working conditions.
•It is necessary to highlight the impact of occupational diseases as a public health problem in Spain in order to approach their prevention and care properly.
Spanish version available www.elsevier.es/268.975
A commentary follow this article (pág. 445)
Study partially supported by a grant from the Ministry of Work and Social Affairs (Reference FIPROS 2005-10).
Correspondence: A.M. García. ISTAS. Almirante, 3, 4.ª.
46003 Valencia. España.
E-mail: anagar@uv.es
Manuscript received January 7, 2008.
Manuscript accepted for publication February 11, 2008.