The presence of BAV is associated with a high incidence of valve dysfunction, proximal aortic dilatation, and an increased incidence of acute aortic events. Current recommendations include an earlier threshold for surgical correction and the use of valve-sparing operations in patients with bicuspid valve insufficiency. However, the reported durability of BAV repair does not appear to be as good as for the tricuspid aortic valve. It may be related to connective tissue disorder, which is often the main feature of BAV. The progressive annular dilatation caused by annulo-aortic ectasia may affect the repair stability, but precise data are still lacking.
17 years long term follow-up of 206 patients I performed BAV repair showed that circumferential annuloplasty significantly improved repair durability.1,2 It has also confirmed the preoperative phenotype as a significant predictor for freedom from redo operation. It has recently been suggested that symmetrical preoperative commissural orientation imposes better postoperative durability.1 It was confirmed with my studies comparing different techniques of annuloplasty.3,4 In spite of inferior durability due to progression of recurrent moderate AR and higher gradients in subcomissural annuloplasty group, they may still present good clinical outcome still a safe and repeatable technique provided properly executed during operation.5 Both conclusions are fundament of my technique with two essential elements which is a annuloplasty, preferably in circular fashion and aiming at 180° symmetry postoperatively.
All the operations followed a similar protocol described previously.6–8 They are presented online in MMCTS format.9,10 Briefly, in all cases, the chest was opened via median sternotomy. A standard-setting cardiopulmonary bypass was initiated, and the myocardium was protected with either blood or del Nido cardioplegia. First, alignment of leaflets, the effective and geometric height of each leaflet. The central leaflet coaptation and individual leaflet prolapse were evaluated by measuring effective coaptation or relative to root leaflet height. Secondly, the relative lengths of the leaflet free margins were assessed by suturing two noduli Arantii together and identifying leaflets with excessively stretched, elongated segments producing prolapse. Then, the fused leaflet anatomy was evaluated. In the case of concomitant bicuspid aortopathy, either aortic root reimplantation or STJ remodeling with supracoronary ascending aortic replacement for ascending aortic diameter ≥45mm were performed. Sizing of the aortic graft, and the external ring is based on the height of leaflets and the height of the subcommissural triangle between the left and non-coronary sinuses and the non-coronary leaflet, according to the El-Khoury and David-Feindel formulas. The commissures are located at 160–180° angles during root remodeling or valve reimplantation to maintain the symmetry of the repaired BAV and to enhance the fused leaflet mobility. In internal annuloplasty, the non-fused leaflet serves as a reference, and its free-edge length (FEL) is measured with a ball sizer that predicts required ring diameter (D) as: D=FEL/1.5.11
The enlarged aortic annulus is stabilized using either subcommissural plication or annuloplasty (SCA) or circumferential annuloplasty techniques: the internal ring annuloplasty or external annuloplasty (EA). SCA was performed with two braided 2-0 pledgeted stitches to narrow two subcommissural triangles, in its upper half to avoid gradient.12,13 Internal ring annuloplasty for bicuspid aortic valve is commercially available as HAART 200™. The bicuspid ring has circular base geometry with 180° sub-commissural posts that flare outward by 10°. The ring is sutured to the valve annulus with 9 trans-annular horizontal mattress sutures – shown in blue. The ring is sized to keep inter-commissural distance constant, but it moves the dilated sinuses centrally to improve leaflet coaptation. Due to 180° symmetry, the ring is able to remodel the annulus by its diameter reduction as well as increase fused leaflet mobility. The EA procedure consisted of the placement of a circular line of six to eight interrupted pledgeted 2-0 braided sutures from inside of the aorta, with another five along the fibrotic part of the annulus and additional ones at the bottom of the third subcommissural triangle and leaflet nadir, supported by a Dacron ring placed from the outside. In other circumstances, EA was part of the reimplantation procedure,5 or when used as a partial supporting ring of fibrotic annulus (55% of circumference), supported with internal goretex suture annuloplasty to avoid deep anterior dissection and coronary mobilization.14
The sinotubular junction (STJ) remodeling was part of the supracoronary Dacron graft implantation. The sizing of the Dacron graft in EA cases were identical. However when internal annuloplasty used, STJ is determined by ring size +7mm. Aorta distal to anastomosis is further secured by wrapping inside the same dacron prosthesis.
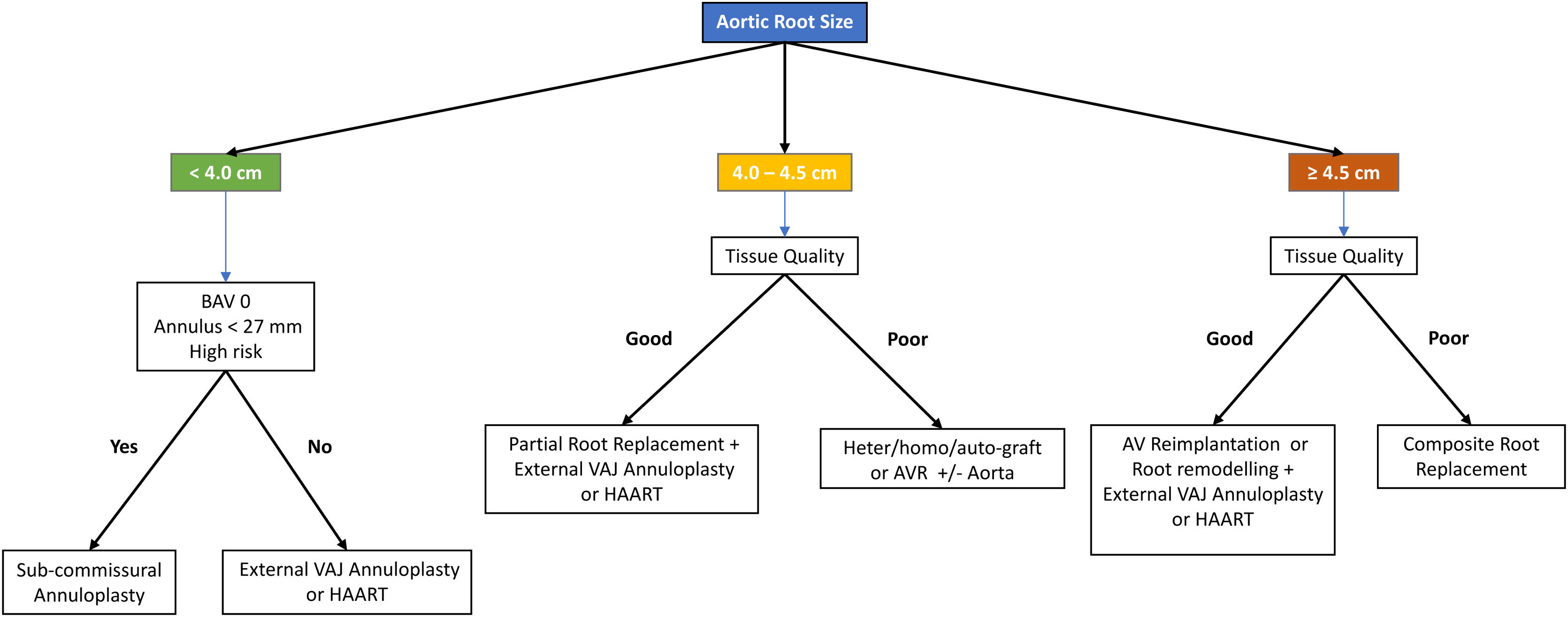
All patients are having various aortic annulus and aortic root procedures, including ones without any type of annuloplasty with or without root remodeling, or with subcommissural plication annuloplasty with or without STJ remodeling or aortic root remodeling, and with circumferential external or internal annuloplasty with concomitant STJ and root remodeling or as an integral part of reimplantation procedure. The proposed algorithm of decision-making in choosing annuloplasty, root and ascending aorta procedure with regard to root size is presented in Fig. 1.
The leaflet repair techniques included prolapse management, raphe excision, enhanced with a patch reconstruction when tissue quality required. The Gore-Tex leaflet stabilization with Gore 7-0 or plication with monofilament 6-0 was added when necessary to correct the remaining prolapse. In all BAV repair cases, the alignment of leaflets was first, followed by the annuloplasty and the final leaflet repair. Strategy of leaflets repair followed classification by Sievers and BAV Consortium.15,16
In BAV type 0 repair, or two-sinus type, both leaflets prolapse has been treated by symmetrical plication to achieve proper effective height.
In BAV type 1 repair, or fused type both symmetric and asymmetric subtype, correction of the reference, non-fused leaflet prolapse, are being addressed first. The correct height of the reference leaflet is determined with the specially designed caliper measuring. The aim is to achieve an effective height greater than 9mm or equal to 50% of the leaflet or root height. This leaflet repair has guided the extent of fused leaflet management. Leaflet shaving is often added to release the leaflet retraction. Root repair and its plication at the leaflet fusion level were performed, as described earlier. In BAV type 1, very asymmetrical type, the linear closure of the major cleft longer than leaflets fusion was carried out, followed by the prolapse plication.
In BAV type 2-unicuspid, a commissurotomy of a minor right-noncoronary commissural fusion is performed converting anatomy to bicuspid type 1 or fused BAV repair. When both major commissural fusions are present resulting in elevated gradient patient are not selected for the repair.
A transesophageal echocardiogram (TEE) is routinely performed three times, before Heart Team, in surgery before the initiation of cardiopulmonary bypass, and at the end of every surgical procedure. The coaptation height is considered acceptable if it was ≥4mm after aortic valve repair and effective height above 9mm.
Conflict of interestNone.