[1]K.A.A. Fox, S.G. Goodman, W. Klein, D. Brieger, Steg PhG, O. Dabbous, Á. Avezum, for the GRACE Investigators.
Management of acute coronary syndromes. Variations in practice and outcome. Findings from the Global Registry of Acute Coronary Events (GRACE).
Eur Heart J, 23 (2002), pp. 1177-1189
[2]C.B. Granger, P.G. Steg, E. Peterson, J. López-Sendón, F. Van de Werf, E. Kline-Rogers, J. Allegrone, O. Dabbous, W. Klein, K.A.A. Fox, K. Eagle, for the GRACE Investigators.
Medication performance measures and mortality following acute coronary syndromes.
Am J Med, 118 (2005), pp. 858-865
[3]T. Jernberg, P. Johanson, C. Held, B. Svennblad, J. Lindbäck, L. Wallentin, for SWEDEHEART/RIKS-HIA.
Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction.
JAMA, 305 (2011), pp. 1677-1684
[4]L.J. Morrison, R.W. Neumar, J.L. Zimmerman, M.S. Link, L.K. Newby, P.W. McMullan Jr., T. Vanden Hoek, C.C. Halverson, L. Doering, M.A. Peberdy, D.P. Edelson, on behalf of the American Heart Association Emergency Cardiovascular Care Committee.
Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association.
Circulation, 127 (2013), pp. 1538-1563
[5]A. Cabadés, L. López-Bescós, F. Arós, A. Loma-Osorio, X. Bosch, P. Pabón, J. Marrugat.
Variability in the management and prognosis at short- and medium-term of myocardial infarct in Spain: the PRIAMHO study. Registration Project of Hospital Acute Myocardial Infarct.
Rev Esp Cardiol, 52 (1999), pp. 767-775
[6]Cleland JGF, Swedberg K, Cohen-Solal A, Cosin-Aguilar J, Dietz R, Follath F, Gavazzi A, Hobbs R, Korewicki J, Madeira HC, Preda I, van Gilst WH, Widimsky J, Mareev V, for The study group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology, Mason J, Freemantle N, Eastaugh J. The Euro Heart Failure Survey of the EUROHEART Survey Programme. A survey on the quality of care among patients with heart failure in Europe. Eur J Heart Fail 2000; 2:123-132.
[7]H. Tunstall-Pedoe, K. Kuulasmaa, M. Mahonen, H. Tolonen, E. Ruokokoski, P. Amouyel.
Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease.
Lancet, 353 (1999), pp. 1547-1557
[8]K.A. Fox, D.V. Cokkinos, J. Deckers, U. Keil, A. Maggioni, G. Steg.
The ENACT study: a pan-European survey of acute coronary syndromes. European Network for Acute Coronary Treatment.
Eur Heart J, 17 (2000), pp. 1440-1449
[9]D. Hasdai, S. Behar, L. Wallentin, N. Danchin, A.G. Gitt, E. Boersma, P.M. Fioretti, M. Simoons, A. Battler.
A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin. The Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS).
Eur Heart J, 23 (2002), pp. 1190-1201
[10]K.A.A. Fox, S.G. Goodman, F.A. Anderson, C.B. Granger, M. Moscucci, M.D. Flather, F. Spencer, A. Budaj, O.H. Dabbous, J.M. Gore, on behalf of the GRACE Investigators.
From guidelines to clinical practice: the impact of hospital and geographical characteristics on temporal trends in the management of acute coronary syndromes. The Global Registry of Acute Coronary Events (GRACE).
Eur Heart J, 24 (2003), pp. 1414-1424
[11]M. Komagda, F. Follath, K. Swedberg, J. Cleland, J.C. Aguilar, A. Cohen-Solal, R. Dietz, A. Gavazzi, W.H. Van Gilst, R. Hobbs, J. Korewicki, H.C. Madeira, V.S. Moiseyev, I. Preda, J. Widimsky, N. Freemantle, J. Eastaugh, J. Mason.
Study Group on Diagnosis of the Working Group onHeart Failure of the European Society of Cardiology. The EuroHeart Failure Survey Programme – a survey on the quality of care among patients with heart failure in Europe. Part 2: Treatment.
Eur Heart J, 24 (2003), pp. 464-474
[12]K.A. Eagle, E. Kline-Rogers, S.G. Goodman, E.P. Gurfinkel, Á. Avezum, M.D. Flather, C.B. Granger, S. Erickson, K. White, Steg PhG, for the GRACE Investigators.
Adherence to evidence-based therapies after discharge for acute coronary syndromes. An ongoing, prospective, observational study.
Am J Med, 117 (2004), pp. 73-81
[13]Admission-based in-hospital case-fatality rates within 30 days after admission for AMI, 2009 Health at a Glance: Europe 2012 - (OECD 2012. doi.org/10.1787/888932704874.
[14]E. Puymirat, A. Battler, J. Birkhead, H. Bueno, P. Clemmensen, Y. Cottin, K.A. Fox, B. Gorenek, C. Hamm, K. Huber, M. Lettino, B. Lindahl, C. Müller, A. Parkhomenko, S. Price, T. Quinn, F. Schiele, M. Simoons, G. Tatu-Chitoiu, M. Tubaro, C. Vrints, D. Zahger, U. Zeymer, N. Danchin.
EHS 2009 snapshot participants. Euro Heart Survey 2009 Snapshot: regional variations in presentation and management of patients with AMI in 47 countries.
Eur Heart J Acute Cardiovasc Care, 4 (2013), pp. 359-370
[15]Z. Reiner, D. De Bacquer, K. Kotseva, C. Prugger, G. De Backer, D. Wood, on behalf of The EUROASPIRE, III, Study Group.
Treatment potential for dyslipidaemia management in patients with coronary heart disease across Europe: Findings from the EUROASPIRE III survey.
Atherosclerosis, 231 (2013), pp. 300-307
[16]V. Bertomeu, A. Cequier, J. Bernal, F. Alfonso, M.P. Anguita, J. Muñizf, J.A. Barrabe, D. García-Dorado, J. Goicolea, F. Elola.
In-hospital mortality due to acute myocardial infarction. Relevance of type of hospital and care provided. RECALCAR study.
Rev Esp Cardiol, 66 (2013), pp. 935-942
[17]R.O. Bonow, F.A. Masoudi, J.S. Rumsfeld, E. Delong, N.A. Estes, 3rd, D.C. Goff Jr., K. Grady, L.A. Green, A.R. Loth, E.D. Peterson, I.L. Piña, M.J. Radford, D.M. Shahian.
ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures.
Circulation, 118 (2008), pp. 2662-2666
[18]J.L. Maeda.
Evidence-based heart failure performance measures and clinical outcomes: a systematic review.
J Card Fail, 16 (2010), pp. 411-418
[20]R.M. Werner, E.T. Bradlow.
Relationship between medicare's hospital compare performance measures and mortality rates.
JAMA, 305 (2011), pp. 1677-1684
[22]H.M. Krumholz, Y. Wang, J.A. Mattera, Y. Wang, L.F. Han, M.J. Ingber, S. Roman, S.L. Normand.
An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure.
Circulation, 113 (2006), pp. 1693-1701
[23]W.R. Lewis, E.D. Peterson, C.P. Cannon, D.M. Super, K.A. LaBresh, K. Quealy, L. Liang, G.C. Fonarow.
An organized approach to improvement in guideline adherence for acute myocardial infarction: results with the Get With The Guidelines quality improvement program.
Arch Intern Med, 168 (2008), pp. 1813-1819
[24]J.M. Austin, A.K. Jha, P.S. Romano, S.J. Singer, T.J. Vogus, R.M. Wachter, P.J. Pronovost.
National hospital ratings systems share few common scores and may generate confusion instead of clarity.
Health Affairs, 34 (2015), pp. 423-430
[25]N.S. Bardach, J.J. Wang, S. De Leon, S.C. Shih, J. Boscardin, E. Goldman, A. Dudley.
Effect of Pay-for-Performance Incentives on Quality of Care in Small Practices With Electronic Health Records. A Randomized Trial.
JAMA, 310 (2013), pp. 1051-1059
[26]P. Chatterjee, K.E. Joynt.
Do cardiology quality measures actually improve patient outcomes?.
J Am Heart Assoc, 3 (2014),
[27]J. Chen, M.J. Radfor, Y. Wang, T.A. Marciniak, H.M. Krumholz.
Do ‘America's best hospitals’ perform better for acute myocardial infarction?.
N Engl J Med, 340 (1999), pp. 286-292
[28]A.D. Simms, P.D. Baxter, B.A. Cattle, P.D. Batin, J.I. Wilson, R.M. West, A.S. Hall, C.F. Weston, J.E. Deanfield, K.A. Fox, K.P. Gale.
An assessment of composite measures of hospital performance and associated mortality for patients with acute myocardial infarction. Analysis of individual hospital performance and outcome for the National Institute for Cardiovascular Outcomes Research (NICOR).
Eur Hear J Acute Cardiovasc Care, 2 (2012), pp. 9-18
[34]A. Scott, P. Sivey, D. Ait Ouakrim, L. Willenberg, L. Naccarella, J. Furler, D. Young.
The effect of financial incentives on the quality of health care provided by primary care physicians.
Cochrane Database Syst Rev, 9 (2011),
[35]S.K. Houle, F.A. McAlister, C.A. Jackevicius, A.W. Chuck, R.T. Tsuyuki.
Does performance-based remuneration for individual health care practitioners affect patient care?. A systematic review.
Ann Intern Med, 157 (2012), pp. 889-899
[36]P.S. Douglas, R.G. Brindis.
A question of quality: why national benchmarking?.
J Am Coll Cardiol, 47 (2006), pp. 1076-1078
[37]G.M. Auton.
Using benchmarking techniques to improve efficiency and quality in cardiology services: Part one and two.
J Cardiovasc Manag, 5 (1994),
[38]K.A. Fox, P.G. Steg, K.A. Eagle, S.G. Goodman, F.A. Anderson Jr., C.B. Granger, M.D. Flather, A. Budaj, A. Quill, J.M. Gore.
GRACE Investigators. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006.
JAMA, 297 (2007), pp. 1892-1900
[39]Instituto de informacion sanitaria. Ministerio de Sanidad. Servicios Sociales e Igualdad. Indicadores clave del Sistema Nacional de Salud.
www.msssi.gob.es (28 January 2015).
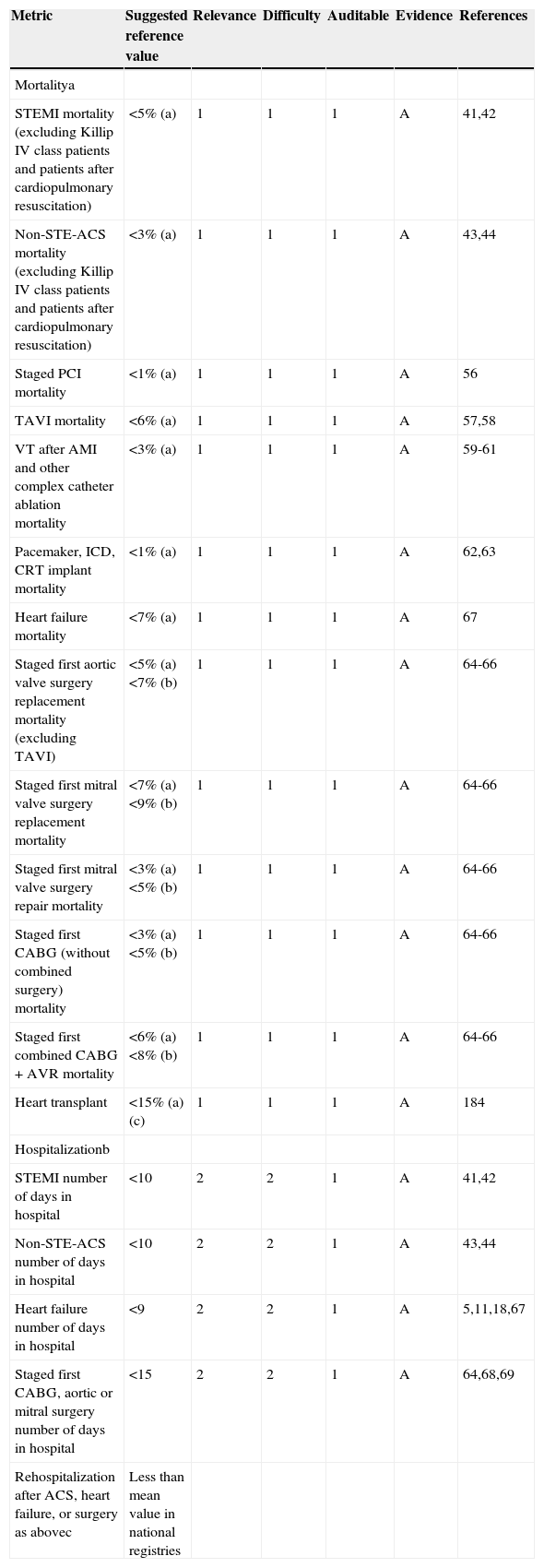
[41]P.G. Steg, S.K. James, D. Atar, L.P. Badano, C. Blömstrom-Lundqvist, M.A. Borger, C. Di Mario, K. Dickstein, G. Ducrocq, F. Fernandez-Aviles, A.H. Gershlick, P. Giannuzzi, S. Halvorsen, K. Huber, P. Juni, A. Kastrati, J. Knuuti, M.J. Lenzen, K.W. Mahaffey, M. Valgimigli, A. van ‘t Hof, P. Widimsky, D. Zahger.
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation.
Eur Heart J, 33 (2012), pp. 2569-2619
[42]P.T. O’Gara, F.G. Kushner, D.D. Ascheim, D.E. Casey Jr., M.K. Chung, J.A. de Lemos, S.M. Ettinger, J.C. Fang, F.M. Fesmire, B.A. Franklin, C.B. Granger, H.M. Krumholz, J.A. Linderbaum, D.A. Morrow, L.K. Newby, J.P. Ornato, N. Ou, M.J. Radford, J.E. Tamis-Holland, C.L. Tommaso, C.M. Tracy, Y.J. Woo, D.X. Zhao.
2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.
J Am Coll Cardiol, 61 (2013), pp. e78-e140
[43]C.W. Hamm, J.P. Bassand, S. Agewall, J. Bax, E. Boersma, H. Bueno, P. Caso, D. Dudek, S. Gielen, K. Huber, M. Ohman, M.C. Petrie, F. Sonntag, M.S. Uva, R.F. Storey, W. Wijns, D. Zahger.
ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC).
Eur Heart J, 32 (2011), pp. 2999-3054
[44]E.A. Amsterdam, N.K. Wenger, R.G. Brindis, D.E. Casey Jr., T.G. Ganiats, D.R. Holmes Jr., A.S. Jaffe, H. Jneid, R.F. Kelly, M.C. Kontos, G.N. Levine, P.R. Liebson, D. Mukherjee, E.D. Peterson, M.S. Sabatine, R.W. Smalling, S.J. Zieman.
2014 /ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
J Am Coll Cardiol, 64 (2014), pp. e139-e228
[45]J. McMurray, S. Adamopoulos, S. Anker, A. Auricchio, M. Böhm, K. Dickstein, V. Falk, G. Filippatos, C. Fonseca, M. Gomez-Sanchez, T. Jaarsma, L. Køber, G. Lip, A. Maggioni, A. Parkhomenko, B. Pieske, B. Popescu, P. Rønnevik, F. Rutten, J. Schwitter, P. Seferovic, J. Stepinska, P. Trindade, A. Voors, F. Zannad, A. Zeiher.
ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC.
Eur Heart J, 33 (2012), pp. 1787-1847
[46]C.W. Yancy, M. Jessup, B. Bozkurt, J. Butler, D.E. Casey, M.H. Drazner, G.C. Fonarow, S.A. Geraci, T. Horwich, J.L. Januzzi, M.R. Johnson, E.K. Kasper, W.C. Levy, F.A. Masoudi, P.E. McBride, J.J.V. McMurray, J.E. Mitchell, P.N. Peterson, B. Riegel, F. Sam, L.W. Stevenson, W.H.W. Tang, E.J. Tsai, B.L. Wilkoff.
2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.
Circulation, 128 (2013), pp. e240-e327
[47]K.A. Hicks, J.E. Tcheng, B. Bozkurt, B.R. Chaitman, D.E. Cutlip, A. Farb, G. Fonarow, J. Jacobs, M. Jaff, J.H. Lichtman, M. Limacher, K. Mahaffey, R. Mehran, S. Nissen, E.E. Smith, S. Targum.
2014 ACC/AHA Key Data Elements and Definitions for Cardiovascular Endpoint Events in Clinical Trials. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards).
Circulation 2015; 131. Published online before print 29 December, (2014),
[48]K. Thygesen, J.S. Alpert, H.D. White, A.S. Jaffe, H.A. Katus, F.S. Apple, B. Lindahl, D.A. Morrow, B.A. Chaitman, P.M. Clemmensen, P. Johanson, H. Hod, R. Underwood, J.J. Bax, R.O. Bonow, F. Pinto, R.J. Gibbons, K.A. Fox, D. Atar, L.K. Newby, M. Galvani, C.W. Hamm, B.F. Uretsky, P.G. Steg, W. Wijns, J.P. Bassand, P. Menasché, J. Ravkilde, E.M. Ohman, E.M. Antman, L.C. Wallentin, P.W. Armstrong, M.L. Simoons, J.L. Januzzi, M.S. Nieminen, M. Gheorghiade, G. Filippatos, R.V. Luepker, S.P. Fortmann, W.D. Rosamond, D. Levy, D. Wood, S.C. Smith, D. Hu, J.L. Lopez-Sendon, R.M. Robertson, D. Weaver, M. Tendera, A.A. Bove, A.N. Parkhomenko, E.J. Vasilieva, S. Mendis.
ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction.
Eur Heart J, 33 (2012), pp. 2551-2567
[49]Y. Hong, K.A. LaBresh.
Overview of the American Heart Association ‘Get With the Guidelines’ Programs: coronary heart disease, stroke, and heart failure.
Crit Pathw Cardiol, 5 (2006), pp. 179-186
[50]A.C. Anyanwu, F. Filsoufi, S.P. Salzberg, D.J. Bronster, D.H. Adams.
Epidemiology of stroke after cardiac surgery in the current era.
J Thorac Cardiovasc Surg, 134 (2007), pp. 1121-1127
[51]D.M. Shahian, S.M. O’Brien, G. Filardo, V.A. Ferraris, C.K. Haan, J.B. Rich, S.L. Normand, E.R. DeLong, C.M. Shewan, R.S. Dokholyan, E.D. Peterson, F.H. Edwards, R.P. Anderson.
Society of Thoracic Surgeons Quality Measurement Task Force. The Society of Thoracic Surgeons 2008 Cardiac Surgery Risk Models: Part 1—coronary artery bypass grafting surgery.
Ann Thorac Surg, 88 (2009), pp. S2-S22
[52]G.C. Fonarow, M.J. Alberts, J.P. Broderick, E.C. Jauch, D.O. Kleindorfer, J.R. Saver, P. Solis, R. Suter, L.H. Schwamm.
Stroke outcomes measures must be appropriately risk adjusted to ensure quality care of patients. A presidential advisory from the American Heart Association/American Stroke Association.
Stroke, 45 (2014), pp. 1589-1601
[53]Q. Li, S.G. Goodman, R.T. Yan, J.M. Gore, P. Polasek, K. Lai, C. Baer, R.J. Goldberg, A. Pinter, K. Ahmad, J.M. Kornder, A.T. Yan.
Global Registry of Acute Coronary Events and the Canadian Registry of Acute Coronary Events Investigators. Pre-hospital cardiac arrest in acute coronary syndromes: insights from the Global Registry of Acute Coronary Events and the Canadian Registry of Acute Coronary Events.
Cardiology, 126 (2013), pp. 27-34
[54]H.H. Awad, F.A. Anderson Jr., J.M. Gore, S.G. Goodman, R.J. Goldberg.
Cardiogenic shock complicating acute coronary syndromes: insights from the Global Registry of Acute Coronary Events.
Am Heart J, 163 (2012), pp. 963-971
[55]K.A. Fox, K.A. Eagle, J.M. Gore, P.G. Steg, F.A. Anderson.
GRACE and GRACE2 Investigators. The Global Registry of Acute Coronary Events, 1999 to 2009 – GRACE.
Heart, 96 (2010), pp. 1095-1101
[56]Harold JG, Bass TA, Bashore TM, Brindis RG, Brush JE Jr, Burke JA, Dehmer GJ, Deychak YA, Jneid H, Jollis JG, Landzberg JS, Levine GN, McClurken JB, Messenger JC, Moussa ID, Muhlestein JB, Pomerantz RM, Sanborn TA, Sivaram CA, White CJ, Williams ES. American College of Cardiology Foundation; American Heart Association; Society of Cardiovascular Angiography and Interventions. ACCF/AHA/SCAI 2013 Update of the Clinical Competence Statement on Coronary Artery Interventional Procedures. This document is available on the World Wide Web sites of the American College of Cardiology (
http://www.cardiosource.org), the American Heart Association (
http://my.americanheart.org), and the Society for Cardiovascular Angiography and Interventions (
http://www.scai.org), Copublished: JACC, Circulation, Cath Cardiovasc Interventions. 2013 (6 February 2015).
[57]Schymik G, Würth A, Bramlage P, Herbinger T, Heimeshoff M, Pilz L, Schymik JS, Wondraschek R, Süselbeck T, Gerhardus J, Luik A, Gonska BD, Posival H, Schmitt C, Schröfel H. Long-Term Results of Transapical Versus Transfemoral TAVI in a Real World Population of 1000 Patients With Severe Symptomatic Aortic Stenosis. Circ Cardiovasc Interv 2014; 8. doi:10.1161/CIRCINTERVENTIONS. 113.000761.
[58]M. Sabaté, S. Cánovas, E. García, R. Hernández Antolín, L. Maroto, J.M. Hernández, L. Maroto, J.M. Hernández, J.H. Alonso Briales, A.J. Muñoz García, E. Gutiérrez-Ibañes, J. JRodríguez-Roda.
TAVI National Group colaborators. Predictores de mortalidad hospitalaria y a medio plazo tras el reemplazo valvular aórtico transcatéter: datos del registro nacional TAVI 2010-2011.
Rev Esp Cardiol, 66 (2013), pp. 949-958
[59]E.M. Aliot, W.G. Stevenson, J.M. Almendral Garrote, F. Bogun, H. Calkins, E. Delacretaz, P. Della Bella, G. Hindricks, P. Jaïs, M.E. Josephson, J. Kautzner, G.N. Kay, K.H. Kuck, B.B. Lerman, F. Marchlinski, V. Reddy, M.J. Schalij, R. Schilling, K. Soejima, D. Wilber.
EHRA/HRS Expert consensus on catheter ablation of ventricular arrhythmia.
Heart Europace, 11 (2009), pp. 771-817
[60]D.F. Katz, M.P. Turakhia, W.H. Sauer, W.S. Tzou, R.R. Heath, M.M. Zipse, R.G. Aleong, P.D. Varosy, D.P. Kao.
Safety of ventricular tachycardia ablation in clinical practice: findings from 9.699 hospital discharge records.
Circ Arrhythm Electrophysiol, 8 (2015), pp. 362-370
[61]W.G. Stevenson, D.J. Wilber, A. Natale, W.M. Jackman, F.E. Marchlinski, T. Talbert, M.D. Gonzalez, S.J. Worley, E.G. Daoud, C. Hwang, C. Schuger, T.E. Bump, M. Jazayeri, G.F. Tomassoni, H.A. Kopelman, K. Soejima, H. Nakagawa, for the Multicenter Thermocool VT Ablation Trial Investigators.
Irrigated radiofrequency catheter ablation guided by electroanatomic mapping for recurrent ventricular tachycardia after myocardial infarction: the multicenter thermocool ventricular tachycardia ablation trial.
Circulation, 118 (2008), pp. 2773-2782
[62]M. Brignole, A. Auricchio, G. Baron-Esquivias, P. Bordachar, G. Boriani, O.A. Breithardt, J. Cleland, J.C. Deharo, V. Delgado, P.M. Elliott, B. Gorenek, C.W. Israel, C. Leclercq, C. Linde, L. Mont, L. Padeletti, R. Sutton, P. Vardas.
2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy.
Eur Heart J, 34 (2013), pp. 2281-2329
[63]J.V. Freeman, Y. Wang, J.P. Curtis, P.A. Heidenreich, M.A. Hlatky.
The relation between hospital procedure volume and complications of cardioverter defibrillator implantation from the implantable cardioverter-defibrillator registry.
J Am Coll Cardiol, 56 (2010), pp. 1133-1139
[64]L.D. Hillis, P.K. Smith, J.L. Anderson, J.A. Bittl, C.R. Bridges, J.G. Byrne, J.E. Cigarroa, V.J. Disesa, L.F. Hiratzka, A.M. Hutter Jr., M.E. Jessen, E.C. Keeley, S.J. Lahey, R.A. Lange, M.J. London, M.J. Mack, M.R. Patel, J.D. Puskas, J.F. Sabik, O. Selnes, D.M. Shahian, J.C. Trost, M.D. Winniford.
Association Task Force on Practice Guidelines 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart.
Circulation, 124 (2011), pp. 2610-2642
[65]Josa M, Cortina JM, Mestres C, Pereda D, Walton P, Kinsman R. First report of the Spanish Quality Adult Cardiovascular Surgery Project 2013. Published by SECTCV and Dendrite Clinical System Ltd. Henley-on-Thames. ISBN 978-84-9926-504-9.
[66]T. Centella, F. Hornero.
Cirugía Cardiovascular en España en el año 2012. Registro de intervenciones de la Sociedad Española de Cirugía Torácica-Cardiovascular.
Cir Cardiov, 21 (2014), pp. 18-36
[67]R.O. Bonow, T.G. Ganiats, C.T. Beam, K. Blake, D.E. Casey, S.J. Goodlin, K.L. Grady, R.F. Hundley, M. Jessup, T.E. Lynn, F.A. Masoudi, D. Nilasena, I.L. Piña, P.D. Rockswold, L.B. Sadwin, J.D. Sikkema, C.A. Sincak, J. Spertus, P.J. Torcson, E. Torres, M.V. Williams, J.B. Wong.
ACCF/AHA/AMA-PCPI 2011 Performance Measures for Adults With Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association–Physician Consortium for Performance Improvement.
J Am Coll Cardiol, 59 (2012), pp. 1812-1832
[68]R.J. Gibbons, S. Smith, E. Antman.
American College of Cardiology/American Heart Association Clinical Practice Guidelines: Part I. Where do they come from?.
Circulation, 107 (2003), pp. 2979-2986
[69]R.J. Gibbons, S. Smith, E. Antman.
American College of Cardiology/American Heart AssociationClinical Practice Guidelines: Part II. Evolutionary Changes in a Continuous Quality Improvement Project.
Circulation, 107 (2003), pp. 3101-3107
[70]K.A. Fox, O.H. Dabbous, R.J. Goldberg, K.S. Pieper, K.A. Eagle, F. Van de Werf, A. Avezum, S.G. Goodman, M.D. Flather, F.A. Anderson Jr., C.B. Granger.
Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE).
Br Med J, 333 (2006), pp. 1091
[71]D.A. Morrow, E.M. Antman, A. Charlesworth, R. Cairns, S.A. Murphy, J.A. de Lemos, R.P. Giugliano, C.H. McCabe, E. Braunwald.
TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy.
Circulation, 102 (2000), pp. 2031-2037
[72]S.A. Euroscore2Nashef, F. Roques, L.D. Sharples, J. Nilsson, C. Smith, A.R. Goldstone, U. Lockowandt.
5246 EuroSCORE II.
Eur J Cardiothorac Surg, 41 (2012), pp. 734-744
[74]Papadopoulou SL, Girasis C, Dharampal A, Farooq V, Onuma Y, Rossi A, Morel MA, Krestin GP, 5255 Serruys PW, de Feyter PJ, Garcia Garcia HM. CT-SYNTAX score: a feasibility and reproducibility Study. JACC Cardiovasc Imaging 2013; 6:413-415.
[75]S.J. Pocock, C.A. Ariti, J.J. McMurray, A. Maggioni, L. Køber, I.B. Squire, K. Swedberg, J. Dobson, K.K. Poppe, G.A. Whalley, R.N. Doughty.
Meta-Analysis Global Group in Chronic Heart Failure. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies.
Eur Heart J, 34 (2013), pp. 1404-1413
[76]P.N. Peterson, J.S. Rumsfeld, L. Liang, N.M. Albert, A.F. Hernandez, E.D. Peterson, G.C. Fonarow, F.A. Masoudi.
American Heart Association Get With the Guidelines-Heart Failure Program. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program.
Circ Cardiovasc Qual Outcomes, 3 (2010), pp. 25-32
[77]K. Rahimi, D. Bennett, N. Conrad, T.M. Williams, J. Basu, J. Dwight, M. Woodward, A. Patel, J. McMurray, S. MacMahon.
Risk prediction in patients with heart failure. A Systematic Review and Analysis.
J Am Coll Cardiol HF, 2 (2014), pp. 440-446
[79]J.L. Anderson, Co-Chair, P.A. Heidenreich, Co-Chair, P.G. Barnett, M.A. Creager, G.C. Fonarow, R.J. Gibbons, J.L. Halperin, M.A. Hlatky, A.K. Jacobs, D.B. Mark, F.A. Masoudi, E.D. Peterson, L.J. Shaw.
A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. ACC/AHA Statement on Cost/Value Methodology in Clinical Practice Guidelines and Performance Measures.
J Am Coll Cardiol, 63 (2014), pp. 2304-2322
[81]E.D. Peterson, P.M. Ho, M. Barton, C. Beam, L.H. Burgess, D.E. Casey Jr., J.P. Drozda Jr., G.C. Fonarow, D. Goff Jr., K.L. Grady, D.E. King, M.L. King, F.A. Masoudi, D.R. Nielsen, S. Stanko.
ACC/AHA/AACVPR/AAFP/ANA concepts for clinician-patient shared accountability in performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures.
Circulation, 130 (2014), pp. 1984-1994
[82]W.R. Lewis, J.P. Piccini, M.P. Turakhia, A.B. Curtis, M. Fang, R.E. Suter, R.L.2nd Page, G.C. Fonarow.
Get With The Guidelines AFIB: novel quality improvement registry for hospitalized patients with atrial fibrillation.
Circ Cardiovasc Qual Outcomes, 7 (2014), pp. 770-777
[83]M.P. Dorsch, J.M. Lose, R.J. DiDomenico.
The effect of cardiovascular credentialed pharmacists on process measures and outcomes in myocardial infarction and heart failure.
Pharmacotherapy, 34 (2014), pp. 803-808
[84]J. Drozda Jr., J.V. Messer, J. Spertus, B. Abramowitz, K. Alexander, C.T. Beam, R.O. Bonow, J.S. Burkiewicz, M. Crouch, D.C. Goff Jr., R. Hellman, T.3rd James, M.L. King, E.A. Machado Jr., E. Ortiz, M. O’Toole, S.D. Persell, J.M. Pines, F.J. Rybicki, L.B. Sadwin, J.D. Sikkema, P.K. Smith, P.J. Torcson, J.B. Wong.
ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement.
J Am Coll Cardiol., 58 (2011), pp. 316-336
[85]I.J. Kullo, J.F. Trejo-Gutierrez, F. Lopez-Jimenez, R.J. Thomas, T.G. Allison, S.L. Mulvagh, A.M. Arruda-Olson, S.N. Hayes, A.W. Pollak, S.L. Kopecky, R.T. Hurst.
A perspective on the New American College of Cardiology/American Heart Association guidelines for cardiovascular risk assessment.
Mayo Clin Proc, 89 (2014), pp. 1244-1256
[86]R.D. Kociol, B.G. Hammill, G.C. Fonarow, P.A. Heidenreich, A.S. Go, E.D. Peterson, L.H. Curtis, A.F. Hernandez.
Associations between use of the hospitalist model and quality of care and outcomes of older patients hospitalized for heart failure.
JACC Heart Fail, 1 (2013), pp. 445-453
[87]S.V. Arnold, F.A. Masoudi, J.S. Rumsfeld, Y. Li, P.G. Jones, J.A. Spertus.
Derivation and validation of a risk standardization model for benchmarking hospital performance for health-related quality of life outcomes after acute myocardial infarction.
Circulation., 129 (2014), pp. 313-320
[88]R.O. Bonow, P.S. Douglas, A.E. Buxton, D.J. Cohen, J.P. Curtis, E. Delong, J.P. Drozda Jr., T.B. Ferguson Jr., P.A. Heidenreich, R.C. Hendel, F.A. Masoudi, E.D. Peterson, A.J. Taylor.
American College of Cardiology Foundation; American Heart Association Task Force on Performance Measures. ACCF/AHA methodology for the development of quality measures for cardiovascular technology: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures.
Circulation, 124 (2011), pp. 1483-1502
[89]P. Deewania.
Gaps in Guideline Implementation. A Cause for Concern, Time for Action.
J Am Coll Cardiol, 65 (2015), pp. 278-280
[90]Y. Hasin, N. Danchin, G.S. Filippatos, M. Heras, U. Janssens, J. Leor, M. Nahir, A. Parkhomenko, K. Thygesen, M. Tubaro, L.C. Wallentin, I. Zakke.
Working Group on Acute Cardiac Care of the European Society of Cardiology. Recommendations for the structure, organization, and operation of intensive cardiac care units.
Eur Heart J, 26 (2005), pp. 1676-1682
[91]D.A. Morrow, J.C. Fang, D.J. Fintel, C.B. Granger, J.N. Katz, F.G. Kushner, J.K. Kuvin, J. Lopez-Sendon, D. McAreavey, B. Nallamothu, R.L. Page, I.I. Parrillo, J.E. Peterson, P.E.C. Winkelman.
Evolution of Critical Care Cardiology: Transformation of the Cardiovascular Intensive Care Unit and the Emerging Need for New Medical Staffing and Training Models A Scientific Statement From the American Heart Association.
Circulation, 126 (2012), pp. 1408-1428
[92]P. Ballo, F. Bandini, I. Capecchi, L. Chiodi, G. Ferro, A. Fortini, G. Giuliani, G. Landini, R. Laureano, M. Milli, G. Nenci, F. Pizzarelli, G.M. Santoro, P. Vannelli, C. Cappelletti, A. Zuppiroli.
American College of Cardiology Foundation; American Society of Echocardiography. Application of 2011 American College of Cardiology Foundation/American Society of Echocardiography appropriateness use criteria in hospitalized patients referred for transthoracic echocardiography in a community setting.
J Am Soc Echocardiogr, 25 (2012), pp. 589-598
[93]M. Garbi, T. McDonagh, B. Cosyns, C. Bucciarelli-Ducci, T. Edvardsen, A. Kitsiou, K. Nieman, P. Lancellotti.
EACVI Imaging Task Force. Appropriateness criteria for cardiovascular imaging use in heart failure: report of literature review.
Eur Heart J Cardiovasc Imaging, 16 (2015), pp. 147-153
[94]J.V. Tu, A. Chu, L.R. Donovan, D.T. Ko, G.L. Booth, K. Tu, L.C. Maclagan, H. Guo, P.C. Austin, W. Hogg, M.K. Kapral, H.C. Wijeysundera, C.L. Atzema, A.S. Gershon, D.A. Alter, D.S. Lee, C.A. Jackevicius, R.S. Bhatia, J.A. Udell, M.R. Rezai, T.A. Stukel.
The Cardiovascular Health in Ambulatory Care Research Team (CANHEART): Using Big Data to Measure and Improve Cardiovascular Health and Healthcare Services.
Circ Cardiovasc Qual Outcomes., 8 (2015), pp. 204-212
[95]F.A. McAlister, J. Wang, L. Donovan, D.S. Lee, P.W. Armstrong, J.V. Tu.
The influence of patient goals of care on performance measures in patients hospitalized for heart failure: an analysis of the EFFECT registry.
Circ Heart Fail., 8 (2015), pp. 481-488
[96]J.G. Jollis, C.B. Granger, T.D. Henry, E.M. Antman, P.B. Berger, P.H. Moyer, F.D. Pratt, I.C. Rokos, A.R. Acuña, M.L. Roettig, A.K. Jacobs.
Systems of care for ST-segment-elevation myocardial infarction: a report From the American Heart Association's Mission: Lifeline.
Circ Cardiovasc Qual Outcomes, 5 (2012), pp. 423-428
[97]I.R. Dégano, I. Subirana, M. Torre, M. Grau, J. Vila, D. Fusco, I. Kirchberger, J. Ferrières, A. Malmivaara, A. Azevedo, C. Meisinger, V. Bongard, D. Farmakis, M. Davoli, U. Häkkinen, C. Araújo, J. Lekakis, R. Elosua, J. Marrugat, on behalf of the EURHOBOP investigators.
A European benchmarking system to evaluate in-hospital mortality rates in acute coronary syndrome: The EURHOBOP project.
Int J Cardiol, 182 (2015), pp. 509-516
[98]J. López-Sendón, P. Mills, H. Weber, R. Michels, C. Di Mario, G. Philippatos, M. Geras, J.L. Merino, D. Pennell, H. Sochor.
Recommendations on Sub-speciality Accreditation in Cardiology. By The Coordination Task Force on Subspeciality Accreditation of the European Board for the Speciality of Cardiology.
Eur Heart J, 28 (2007), pp. 2163-2171
[100]European Union of Medical Spacielists.
www.uems.eu (Consulted 21 February 2015).
[101]B.A. Popescu, A. Stefanidis, P. Nihoyannopoulos, K.F. Fox, S. Ray, N. Cardim, F. Rigo, L.P. Badano, A.G. Fraser, F. Pinto, J.L. Zamorano, G. Habib, G. Maurer, P. Lancellotti, M.J. Andrade, E. Donal, T. Edvardsen, A. Varga.
Updated standards and processes for accreditation of echocardiographic laboratories from The European Association of Cardiovascular Imaging.
Eur Heart J Cardiovasc Imaging, 15 (2014), pp. 717-727
[102]J.L. Anderson, E.M. Antman, J.G. Harold, M. Jessup, P. O’Gara, F.J. Pinto, P.E. Vardas, J.L. Zamorano.
Clinical practice guidelines on perioperative cardiovascular evaluation collaborative efforts among the ACC.
AHA, and ESC. Circulation, 130 (2014), pp. 2213-2214
[103]S. Fihn, J.C. Blankenship, K.P. Alexander, J.A. Bittl, J. Byrne, B.J. Fletcher, G.C. Fonarow, R.A. Lange, G.L. Levine, T.M. Maddox, S.S. Naidu, E.M. Ohman, P.K. Smith.
2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease.
Circulation, 130 (2014), pp. 1749-1767
[104]D.K. Arnett, R.A. Goodman, J.L. Halperin, J.L. Anderson, A.K. Parekh, W.A. Zoghbi.
AHA/ACC/HHS strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions from the American Heart Association.
American College of Cardiology, and US Department of Health and Human Services. Circulation, 130 (2014), pp. 1662-1667
[105]R.A. Nishimura, K.M. Otto, R.O. Bonow, B.A. Carabello, J.P. Erwin III, R.A. Guyton, P.T. O’Gara, C.E. Ruiz, N.J. Skubas, P. Sorajja, T.M. Sundt III, J.D. Thomas.
ACC/AHA Task Force Members. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
Circulation, 129 (2014), pp. 2440-2492
[106]S. Konstantinides, A. Torbicki, G. Agnelli, N. Danchin, D. Fitzmaurice, N. Galie, J.S. Gibbs, M. Huisman, M. Humbert, N. Kucher, I. Lang, M. Lankeit, J. Lekakis, C. Maack, E. Mayer, N. Meneveau, A. Perrier, P. Pruszczyk, L.H. Rasmussen, T.H. Schindler, P. Svitil, A. Vonk Noordegraaf, J.L. Zamorano, M. Zompatori.
2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism.
Eur Heart J, 35 (2014), pp. 3033-3080
[107]P.M. Elliott, A. Anastasakis, M.A. Borger, M. Borggrefe, F. Cecchi, Charron Ph, A.A. Hagege, A. Lafont, G. Limongelli, H. Mahrholdt, W. McKenna, J. Mogensen, P. Nihoyannopoulos, S. Nistri, G.P. Pieper, B. Pieske, C. Rapezzi, H. Frans, J. Rutten, C. Tillmanns, H. Watkins.
2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy.
Eur Heart J, 35 (2014), pp. 2733-2779
[108]R. Erbel, V. Aboyans, C. Boileau, E. Bossone, R. Di Bartolomeo, H. Eggebrecht, A. Evangelista, V. Falk, H. Frank, O. Gaemperli, M. Grabenwöger, A. Haverich, B. Iung, A. Manolis, F. Meijboom, K.A. Nienaber, M. Roffi, H. Rousseau, U. Sechtem, P.A. Sirnes, R. von Allmen, K.J.M. Vrints.
2014 ESC Guidelines on the diagnosis and treatment of aortic diseases.
Eur Heart J, 35 (2014), pp. 2873-2926
[109]S.D. Kristensen, S. Anker, J. Knuuti, A. Saraste, H.E. Bøtker, S. De Hert, I. Ford, J.R. Gonzalez-Juanatey, S. Pocock, S. Price, M. Roffi, P.A. Sirnes, M. Sousa-Uva, V. Voudris, C. Funck-Brentano.
2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management.
Eur Heart J, 35 (2014), pp. 2383-2431
[110]L. Rydén, P.J. Grant, S. Anker, C. Berne, F. Cosentino, N. Danchin, C. Deaton, J. Escaned, H.P. Hammes, H. Huikuri, M. Marre, N. Marx, L. Mellbin, J. Ostergren, C. Patrono, P. Seferovic, M. Sousa Uva, M.R. Taskinen, M. Tendera, J. Tuomilehto, P. Valensi, J.L. Zamorano.
ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD.
Eur Heart J, 34 (2013), pp. 3035-3087
[111]G. Task Force MembersMontalescot, U. Sechtem, S. Achenbach, F. Andreotti, C. Arden, A. Budaj, R. Bugiardini, F. Crea, T. Cuisset, C. Di Mario, J.R. Ferreira, B.J. Gersh, A.K. Gitt, J.S. Hulot, N. Marx, L.H. Opie, M. Pfisterer, E. Prescott, F. Ruschitzka, M. Sabaté, R. Senior, D.P. Taggart, E.E. van der Wall, C.J. Vrints, E.S.C. Committee for Practice Guidelines, J.L. Zamorano, S. Achenbach, H. Baumgartner, J.J. Bax, H. Bueno, V. Dean, C. Deaton, C. Erol, R. Fagard, R. Ferrari, D. Hasdai, A.W. Hoes, P. Kirchhof, J. Knuuti, P. Kolh, P. Lancellotti, A. Linhart, P. Nihoyannopoulos, M.F. Piepoli, P. Ponikowski, P.A. Sirnes, J.L. Tamargo, M. Tendera, A. Torbicki, W. Wijns, S. Windecker, Document Reviewers, J. Knuuti, M. Valgimigli, H. Bueno, M.J. Claeys, N. Donner-Banzhoff, C. Erol, H. Frank, C. Funck-Brentano, O. Gaemperli, J.R. Gonzalez-Juanatey, M. Hamilos, D. Hasdai, S. Husted, S.K. James, K. Kervinen, P. Kolh, S.D. Kristensen, P. Lancellotti, A.P. Maggioni, M.F. Piepoli, A.R. Pries, F. Romeo, L. Rydén, M.L. Simoons, P.A. Sirnes, P.G. Steg, A. Timmis, W. Wijns, S. Windecker, A. Yildirir, J.L. Zamorano.
2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology.
Eur Heart J, 34 (2013), pp. 2949-3003
[112]G. Mancia, R. Fagard, K. Narkiewicz, J. Redon, A. Zanchetti, M. Böhm, T. Christiaens, R. Cifkova, G. De Backer, A. Dominiczak, M. Galderisi, D.E. Grobbee, T. Jaarsma, P. Kirchhof, S.E. Kjeldsen, S. Laurent, A.J. Manolis, P.M. Nilsson, L.M. Ruilope, R.E. Schmieder, P.A. Sirnes, P. Sleight, M. Viigimaa, B. Waeber, F. Zannad, J. Redon, A. Dominiczak, K. Narkiewicz, P.M. Nilsson, M. Burnier, M. Viigimaa, E. Ambrosioni, M. Caufield, A. Coca, M.H. Olsen, R.E. Schmieder, C. Tsioufis, P. van de Borne, J.L. Zamorano, S. Achenbach, H. Baumgartner, J.J. Bax, H. Bueno, V. Dean, C. Deaton, C. Erol, R. Fagard, R. Ferrari, D. Hasdai, A.W. Hoes, P. Kirchhof, J. Knuuti, P. Kolh, P. Lancellotti, A. Linhart, P. Nihoyannopoulos, M.F. Piepoli, P. Ponikowski, P.A. Sirnes, J.L. Tamargo, M. Tendera, A. Torbicki, W. Wijns, S. Windecker, D.L. Clement, A. Coca, T.C. Gillebert, M. Tendera, E.A. Rosei, E. Ambrosioni, S.D. Anker, J. Bauersachs, J.B. Hitij, M. Caulfield, M. De Buyzere, S. De Geest, G.A. Derumeaux, S. Erdine, C. Farsang, C. Funck-Brentano, V. Gerc, G. Germano, S. Gielen, H. Haller, A.W. Hoes, J. Jordan, T. Kahan, M. Komajda, D. Lovic, H. Mahrholdt, M.H. Olsen, J. Ostergren, G. Parati, J. Perk, J. Polonia, B.A. Popescu, Z. Reiner, L. Rydén, Y. Sirenko, A. Stanton, H. Struijker-Boudier, C. Tsioufis, P. van de Borne, C. Vlachopoulos, M. Volpe, D.A. Wood.
2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC).
Eur Heart J, 34 (2013), pp. 2159-2219
[113]H. Baumgartner, P. Bonhoeffer, N. De Groot, F. de Haan, J. Deanfield, N. Galie, M. Gatzoulis, K. Gohlke-Baerwolf, H. Kaemmerer, K. Kilner, F. Meijboom, B. Mulder, E. Oechslin, J.A. Oliver Serraf, A. Szatmari, E. Thaulow, P.R. Vouhe, E. Walma.
ESC Guidelines for the management of grown-up congenital heart disease.
Eur Heart J, 31 (2010), pp. 2915-2957
[114]A. Moya, R. Sutton, F. Ammirati, J.J. Blanc, M. Brignole, J.B. Dahm, J.C. Deharo, J. Gajek, K. Gjesdal, A. Krahn, M. Massin, M. Pepi, T. Pezawas, R. Ruiz Granell, F. Sarasin, A. Ungar, G. van Dijk, E. Wlama, W. Wieling.
Guidelines for the diagnosis and management of syncope (version 2009).
Eur Heart J, 30 (2009), pp. 2631-2671
[115]N. Galié, M.M. Hoeper, M. Humbert, A. Torbicki, J.L. Vachiery, A.J. Barbera, M. Beghetti, P. Corris, S. Gaine, J.S. Gibbs, M.A. Gomez-Sanchez, G. Jondeau, W. Klepetko, C. Opitz, A. Peacock, L. Rubin, M. Zellweger, G. Simonneau.
Guidelines for the diagnosis and treatment of pulmonary hypertension.
Eur Heart J, 30 (2009), pp. 2493-2537
[116]B. Maisch, P. Spherovic, A.D. Ristic, R. Erbel, R. Rienmuller, Y. Adler, W. Tomkowski, G. Thiene, H. Magdi.
Yacoub guidelines on the diagnosis and management of pericardial diseases.
Eur Heart J, 25 (2004), pp. 1-28
[117]J. López-Sendón, K. Swedberg, J. McMurray, J. Tamargo, A.P. Maggioni, H. Dargie, M. Tendera, F. Waagstein, J. Kiekshus, P. Lechat, C. Torp-Pedersen.
Expert consensus document on angiotensin converting enzyme inhibitors in cardiovascular disease. The task Force on ACE-inhibitors of the European Society of Cardiology.
Eur Heart J, 25 (2004), pp. 1454-1470
[118]J. López-Sendón, K. Swedberg, J. McMurray, J. Tamargo, A.P. Maggioni, H. Dargie, M. Tendera, F. Waagstein, J. Kiekshus, P. Lechat, C. Torp-Pedersen.
Expert consensus document on beta-adrenergic receptor blockers. The task Force on betablockers of the European Society of Cardiology. European Society of Cardiology consensus statement.
Eur Heart J, 25 (2004), pp. 1341-1362
[119]P.M. Seferovic, S. Stoerk, G. Filippatos, V. Mareev, A. Kavoliuniene, A.D. Ristic, P. Ponikowski, J. McMurray, A. Maggioni, F. Ruschitzka, D.J. van Veldhuisen, A. Coats, M. Piepoli, T. McDonagh, J. Riley, A. Hoes, B. Pieske, M. Dobric, Z. Papp, A. Mebazaa, J. Parissis, T. Ben Gal, D. Vinereanu, D. Brito, J. Altenberger, P. Gatzov, I. Milinkovic, J. Hradec, J.N. Trochu, O. Amir, B. Moura, M. Lainscak, J. Comin, G. Wikström, S. Anker.
Organization of heart failure management in European Society of Cardiology member countries: survey of the Heart Failure Association of the European Society of Cardiology in collaboration with the Heart Failure National Societies/Working Groups.
Eur J Heart Fail, 15 (2013), pp. 947-959
[120]Sánchez Fernández PL, A¿lvarez Rodríguez J, Casado Flores I, Botas Rodrguez J, de Alba Montero JM, del Corral Torres E, Honrubia Fernández T, Huertas Alcázar P, Goicolea Rupérez J, Hernández Antolin RA, Jiménez Mena M, López de Sá y Areses E, Martín Reyes R, Salanova González GS. Reperfusión del infarto agudo de miocardio con elevación de ST en Codigo Infarto en la comunidad de Madrid. Plan Estratégico CARDIOLOGIA 2011-2015.
http://www.madrid.org/cs/Satellite?blobcol=urldata&blobheader=application%2Fpdf&blobheadername1=Content-disposition&blobheadername2=cadena&blobheadervalue1=filename%3DLibro+Codigo+infarto.pdf&blobheadervalue2=language%3Des%26site%3DPortalSalud&blobkey=id&blobtable=MungoBlobs&blobwhere=1352853918919&ssbinary=true.
[121]F. Breuckmann, M. Hochadel, H. Darius, E. Giannitsis, T. Münzel, L.S. Maier, C. Schmitt, B. Schumacher, G. Heusch, T. Voigtländer, H. Mudra, J. Senges.
Guideline-adherence and perspectives in the acute management of unstable angina – initial results from the German chest pain unit registry.
[122]P.S. Douglas, J. Chen, L. Gillam, R. Hendel, W.G. Hundley, F. Masoudi, M.R. Patel, E. Peterson.
Achieving quality in cardiovascular imaging II Proceedings form the ACC-Duke University Medical Center Think Tank on quality in cardiovascular imaging.
JACC Cardiovascular Imaging, 2 (2009), pp. 231-240
[123]R.F. Stainback.
Overview of quality in cardiovascular imaging and procedures for clinicians: focus on appropriate-use-criteria guidelines.
Methodist Debakey Cardiovasc J, 10 (2014), pp. 178-184
[124]P.S. Douglas, J.M. DeCara, R.B. Devereux, S. Duckworth, J.M. Gardin, W.A. Jaber, A.J. Morehead, J.K. Oh, M.H. Picard, S.D. Solomon, K. Wei, N.J. Weissman.
American Society of Echocardiography Standards; American College of Cardiology Foundation. Echocardiographic imaging in clinical trials: American Society of Echocardiography Standards for echocardiography core laboratories: endorsed by the American College of Cardiology Foundation.
J Am Soc Echocardiogr, 22 (2009), pp. 755-765
[125]T. Ryan, W.F. Armstrong, B.K. Khandheria.
American Society of Echocardiography. Task Force 4: training in echocardiography.
J Am Coll Cardiol, 51 (2008), pp. 361-367
[126]J.D. Thomas, W.A. Zoghbi, G.A. Beller, R.O. Bonow, M.J. Budoff, M.D. Cerqueira, M.A. Creager, P.S. Douglas, V. Fuster, M.J. Garcia, D.R. Holmes Jr., W.J. Manning, G.M. Pohost, T.J. Ryan, W.A. Van Decker, S.E. Wiegers.
American College of CArdiology Foundation (ACCF); American Heart Association (AHA); American College of Physicians (ACP) Task Force on Clinical Competence and Training. ACCF 2008 Training Statement on Multimodality Noninvasive Cardiovascular Imaging A Report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training Developed in Collaboration With the American Society of Echocardiography, the American Society of Nuclear Cardiology, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society for Vascular Medicine.
J Am Coll Cardiol, 53 (2009), pp. 125-146
[128]S. Plein, J. Schulz-Menger, A. Almeida, H. Mahrholdt, F. Rademakers, D. Pennell, E. Nagel, J. Schwitter, M. Lombardi.
Working Group on Cardiovascular Magnetic Resonance, European Society of Cardiology. Training and accreditation in cardiovascular magnetic resonance in Europe: a position statement of the working group on cardiovascular magnetic resonance of the ESC.
Eur Heart J, 32 (2011), pp. 793-798
[129]M.H. Picard, D. Adams, S.M. Bierig, J.M. Dent, P.S. Douglas, L.D. Gillam, A.M. Keller, D.J. Malenka, F.A. Masoudi, M. McCulloch, P.A. Pellikka, P.J. Peters, R.F. Stainback, G.M. Strachan, W.A. Zoghbi.
American Society of Echocardiography. American Society of Echocardiography recommendations for quality echocardiography laboratory operations.
J Am Soc Echocardiogr, 24 (2011), pp. 1-10
[132]A.J. Taylor, M. Cerqueira, J.M. Hodgson, D. Mark, J. Min, P. O’Gara, G.D. Rubin.
American College of Cardiology Foundation Appropriate Use Criteria Task Force; Society of Cardiovascular Computed Tomography; American College of Radiology; American Heart Association; American Society of Echocardiography; American Society of Nuclear Cardiology; North American Society for Cardiovascular Imaging; Society for Cardiovascular Angiography and Interventions; Society for Cardiovascular Magnetic Resonance. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance.
Circulation, 122 (2010), pp. e525-e555
[133]S. Voros, J.J. Rivera, D.S. Berman, R. Blankstein, M.J. Budoff, R.C. Cury, M.Y. Desai, D. Dey, S.S. Halliburton, H.S. Hecht, K. Nasir, R.D. Santos, M.D. Shapiro, A.J. Taylor, U.S. Valeti, P.M. Young, G. Weissman.
Society for Atherosclerosis Imaging and Prevention Tomographic Imaging and Prevention Councils; Society of Cardiovascular Computed Tomography. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography.
J Cardiovasc Comput Tomogr, 5 (2011), pp. 75-83
[134]P.S. Douglas, B. Khandheria, R.F. Stainback, N.J. Weissman, E.D. Peterson, R.C. Hendel, R.F. Stainback, M. Blaivas, R.D. Des Prez, L.D. Gillam, T. Golash, L.F. Hiratzka, W.G. Kussmaul, A.J. Labovitz, J. Lindenfeld, F.A. Masoudi, P.H. Mayo, D. Porembka, J.A. Spertus, L.S. Wann, S.E. Wiegers, R.G. Brindis, P.S. Douglas, M.R. Patel, M.J. Wolk, J.M. Allen.
American College of Cardiology Foundation Appropriateness Criteria Task Force; American Society of Echocardiography; American College of Emergency Physicians; American Heart Association; American Society of Nuclear Cardiology; Society for Cardiovascular Angiography and Interventions; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance. ACCF/ASE/ACEP/AHA/ASNC/SCAI/SCCT/SCMR 2008 appropriateness criteria for stress echocardiography.
Circulation, 117 (2008), pp. 1478-1497
[135]T.R. Porter, S. Abdelmoneim, J.T. Belcik, M.L. McCulloch, S.L. Mulvagh, J.J. Olson, C. Porcelli, G.M. Tsutsui, K.W. Wei.
Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography.
J Am Soc Echocardiogr, 27 (2014), pp. 797-810
[136]J. Case, T. Bateman.
Taking the perfect nuclear image: quality control, acquisition, and processing techniques for cardiac SPECT, PET, and hybrid imaging.
J Nucl Cardiol, 20 (2013), pp. 807-891
[137]R. Smith-Bindman, J. Lipson, R. Marcus, K.P. Kim, M. Mahesh, R. Gould, A. Berrington de González, D.L. Miglioretti.
Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer.
Arch Intern Med, 169 (2009), pp. 2078-2086
[138]M. Senni, P. Parrella, R. De Maria, C. Cottini, M. Böhm, P. Ponikowski, G. Filippatos, C. Tribouilloy, A. Di Lenarda, F. Oliva, G. Pulignano, M. Cicoira, S. Nodari, M. Porcu, G. Cioffi, D. Gabrielli, O. Parodi, P. Ferrazzi, A. Gavazzi.
Predicting heart failure outcome from cardiac and comorbid conditions: the 3C-HF score.
Int J Cardiol, 163 (2013), pp. 206-211
[139]A. Sionis, J.M. Ruiz-Nodar, A. Fernández-Ortiz, F. Marín, E. Abu-Assi, O. Díaz-Castro, I.J. Nuñez-Gil, R.M. Lidón.
Update on ischemic heart disease and intensive cardiac care. Rev Esp Cardiol (Engl Ed), 68 (2015), pp. 234-241
[140]T.M. Bashore, S. Balter, A. Barac, J.G. Byrne, J.J. Cavendish, C.E. Chambers, J.B. Hermiller Jr., S. Kinlay, J.S. Landzberg, W.K. Laskey, C.R. McKay, J.M. Miller, D.J. Moliterno, J.W. Moore, S.M. Oliver-McNeil, J.J. Popma, C.L. Tommaso.
2012 American College of Cardiology Foundation/Society for Cardiovascular Angiography and Interventions Expert Consensus Document on Cardiac Catheterization Laboratory Standards Update.
J Am Coll Cardiol, 59 (2012), pp. 2221-2305
[141]N. Patel, G.L. De Maria, G. Kassimis, K. Rahimi, D. Bennett, P. Ludman, A.P. Banning.
Outcomes After Emergency Percutaneous Coronary Intervention in Patients With Unprotected Left Main Stem Occlusion. The BCIS National Audit of Percutaneous Coronary Intervention 6-Year Experience.
J Am Coll Cardiol Intv, 7 (2014), pp. 969-980
[142]G.J. Dehmer, J.C. Blankenship, M. Cilingiroglu, J. Dwyer, D. Feldman, T. Gardner, C.L. Gardner, M. Singh.
SCAI/ACC/AHA expert consensus document: 2014 update on percutaneous coronary intervention without on-site surgical backup.
Circulation, 129 (2014), pp. 2610-2626
[143]T.A. Sanborn, J.E. Tcheng, H.V. Anderson, C.E. Chambers, S.L. Cheatham, M.V. DeCaro, J.C. Durack, A.D. Everett, J.B. Gordon, W.E. Hammond, Z.M. Hijazi, V.S. Kashyap, M. Knudtson, M.J. Landzberg, M.A. Martinez-Rios, L.A. Riggs, K. Hian Sim, D.J. Slotwiner, H. Solomon, W.Y. Szeto, B.H. Weiner, W.S. Weintraub, J.R. Windle.
ACC/AHA/SCAI 2014 health policy statement on structured reporting for the cardiac catheterization laboratory a report of the American College of Cardiology Clinical Quality Committee.
Circulation, 129 (2014), pp. 2578-2609
[144]D.L. Miller, S. Balter, R.G. Dixon, B. Nikolic, G. Bartal, J.F. Cardella, for the Society of Interventional Radiology Standards of Practice Committee.
Quality improvement guidelines for recording patient radiation dose in the medical record for fluoroscopically guided procedures.
J Vasc Interv Radiol, 23 (2012), pp. 11-18
[145]S.S. Jolly, S. Yusuf, J. Cairns, K. Niemelä, D. Xavier, P. Widimsky, A. Budaj, M. Niemelä, V. Valentin, B.S. Lewis, A. Avezum, P.G. Steg, S.V. Rao, P. Gao, R. Afzal, C.D. Joyner, S. Chrolavicius, S.R. Mehta.
RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial.
Lancet, 377 (2011), pp. 1409-1420
[146]A. Vahanian, O. Alfieri, F. Andreotti, M.J. Antunes, G. BarÓn-Esquivias, H. Baumgartner, M.A. Borger, T.P. Carrel, M. De Bonis, A. Evangelista, V. Falk, B. Iung, P. Lancellotti, L. Pierard, S. Price, H.J. Schäfers, G. Schuler, J. Stepinska, K. Swedberg, J. Takkenberg, U.O. Von Oppell, S. Windecker, J.L. Zamorano, M. Zembala.
Guidelines on the management of valvular heart disease.
Eur Heart J, 33 (2012), pp. 2451-2496
[147]A. Aggarwal, D. Dai, J.S. Rumsfeld, L.W. Klein, M.T. Roe.
American College of Cardiology National Cardiovascular Data Registry. Incidence and predictors of stroke associated with percutaneous coronary intervention.
Am J Cardiol, 104 (2009), pp. 349-353
[148]P.G. Steg, K.A. Fox, K.A. Eagle, M. Furman, F. Van de Werf, G. Montalescot, S.G. Goodman, A. Avezum, W. Huang, J.M. Gore.
Global Registry of Acute Coronary Events (GRACE) Investigators. Mortality following placement of drug-eluting and bare-metal stents for ST-segment elevation acute myocardial infarction in the Global Registry of Acute Coronary Events.
Eur Heart J, 30 (2009), pp. 321-329
[149]S. Windecker, P. Kolh, F. Alfonso, J.F. Collet, J. Cremer, W. Falk, G. Filippatos, C. Hamm, S.J. Head, P. Jüni, P. Pieter Kappetein, A. Kastrati, J. Knuuti, U. Landmesser, G. Laufer, F.J. Neumann, D. Richter, P. Schauerte, M. Sousa Uva, S. Stefanini, D.P. Taggart, L. Torracca, M. Valgimigli, W. Wijns, A. Witkowski.
2014 ESC/EACTS Guidelines on myocardial revascularization.
Eur Heart J, 35 (2014), pp. 2541-2619
[150]H. Calkins, J. Brugada, D.L. Packer, R. Cappato, S.A. Chen, H.J. Crijns, R.J. Damiano Jr., D.W. Davies, D.E. Haines, M. Haissaguerre, Y. Iesaka, W. Jackman, P. Jais, H. Kottkamp, K.H. Kuck, B.D. Lindsay, F.E. Marchlinski, P.M. McCarthy, J.L. Mont, F. Morady, K. Nademanee, A. Natale, C. Pappone, E. Prystowsky, A. Raviele, J.N. Ruskin, R.J. Shemin.
HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation.
Heart Rhythm, 4 (2007), pp. 816-861
[151]Wann LS, Curtis AB, January CT, Ellenbogen KA, Lowe JE, Estes NA 3rd, Page RL, Ezekowitz MD, Slotwiner DJ, Jackman WM, Stevenson WG, Tracy CM; 2011 Writing Group Members, Fuster V, Rydén LE, Cannom DS, Le Heuzey JY, Crijns HJ, Lowe JE, Curtis AB, Olsson S, Ellenbogen KA, Prystowsky EN, Halperin JL, Tamargo JL, Kay GN, Wann L, 2006 Writing Committee Members, Jacobs AK, Anderson JL, Albert N, Hochman JS, Buller CE, Kushner FG, Creager MA, Ohman EM, Ettinger SM, Stevenson WG, Guyton RA, Tarkington LG, Halperin JL, Yancy CW, ACCF/AHA Task Force Members. 2011 ACCF/AHA/HRS Focused update on the management of patients with atrial fibrillation (Updating the 2006 Guideline): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011; 123:104-123.
[152]A. Deshmukh, N.J. Patel, S. Pant, N. Shah, A. Chothani, K. Mehta, P. Grover, V. Singh, S. Vallurupalli, G.T. Savani, A. Badheka, T. Tuliani, K. Dabhadkar, G. Dibu, Y.M. Reddy, A. Sewani, M. Kowalski, R. Mitrani, H. Paydak, J.F. Viles-Gonzalez.
In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010. Analysis of 93.801 procedures.
Circulation, 128 (2013), pp. 2104-2112
[153]A. Ferrero de Loma-Osorio, E. Díaz-Infante, A. Macías Gallego.
Registro Español de Ablación con Catéter. XII informe oficial de la Sección de Electrofisiología y Arritmias de la Sociedad Española de Cardiología.
Rev Esp Cardiol, 66 (2013), pp. 983-992
[154]K.H. Kuck, E. Wissner, A. Metzner.
How to Establish an Arrhythmia Unit in the 21st Century.
Rev Esp Cardiol, 65 (2012), pp. 92-96
[155]J. Brugada, F.J. Alzueta, A. Asso, J. Farré, J.J. Olalla, L. Tercedor.
Guías de práctica clínica de la Sociedad Española de Cardiología sobre requerimientos y equipamiento en electrofisiología.
Rev Esp Cardiol, 54 (2001), pp. 887-891
[156]Merino JL, Arribas F, Botto GL, Huikuri H, Kraemer LI, Linde C, Morgan JM, Schalij M, Simantirakis E, Wolpert C, Villard MC, Poirey J, Karaim-Fanchon S, Deront K; 2005-2007 Accreditation Committee of the European Heart Rhythm Association. Core curriculum for the heart rhythm specialist. Europace 2009; 11:iii 1-26.
[157]J.L. Merino, F. Arribas, M. Lopez Gil, X. Viñolas.
La arritmología como una especialidad dentro de la Cardiología: Sistema de acreditación en electrofisiología cardiaca intervencionista de la Sección de Electrofisiología y Arritmias de la Sociedad Española de Cardiología.
Rev Esp Cardiol, 10 (2010),
[159]C.T. January, L.S. Wann, J.S. Alpert, H. Calkins, J.E. Cigarroa, J.C. Cleveland Jr., J.B. Conti, P.T. Ellinor, M.D. Ezekowitz, M.E. Field, K.T. Murray, R.L. Sacco, W.G. Stevenson, P.J. Tchou, C.M. Tracy, C.W. Yancy.
ACC/AHA Task Force Members. 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society.
Circulation, 130 (2014), pp. 2071-2104
[160]A.M. Russo, R.F. Stainback, S.R. Bailey, A.E. Epstein, P.A. Heidenreich, M. Jessup, S. Kapa, M.S. Kremers, B.D. Lindsay, L.W. Stevenson.
ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implanted cardioverter-defibrillator and cardiac resynchronization therapy.
J Am Coll Cardiol, 61 (2013), pp. 1318-1368
[161]D.R. Holmes, J.B. Rich, W.A. Zoghbi, M.J. Mack.
The Heart Team of cardiovascular care.
J Am Coll Cardiol, 61 (2013), pp. 903-907
[162]Albert NM, Barnason S, Deswal A, Hernandez Kociol R, Lee E, Paul S, Ryan CJ, White-Williams, on behalf of the American Heart Association Complex Cardiovascular Patient and Family Care Committee of the Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Transitions of care in heart failure. A scientific statement from the American Heart Association. Circ Heart Fail 2015; 8:384-409.
[163]G.S. Francis, B.H. Greenberg, D.T. Hsu, B.E. Jaski, M. Jessup, M.M. LeWinter, F.D. Pagani, I.L. Piña, M.J. Semigran, M.N. Walsh, D.H. Wiener, J. Yancy, W. Clyde.
ACCF/AHA/ACP/HFSA/ISHLT 2010 clinical competence statement on management of patients with advanced heart failure and cardiac transplant. A report of the ACCF/AHA/ACP task force on clinical competence and training.
J Am Coll Cardiol, 56 (2010), pp. 424-453
[164]L.A. Allen, L.W. Stevenson, K.L. Grady, N.E. Goldstein, D.D. Matlock, R.M. Arnold, N.R. Cook, G.M. Felker, G.S. Francis, P.J. Hauptman, E.P. Havranek, H.M. Krumholz, D. Mancini, B. Riegel, J.A. Spertus.
Decision making in advanced heart failure a scientific statement from the American Heart Association.
Circulation, 125 (2012), pp. 1928-1952
[165]S.M. Campbell, S. Ludt, J. Van Lieshout, N. Boffin, M. Wensing, D. Petek, R. Grol, M.O. Roland.
Quality indicators for the prevention and management of cardiovascular disease in primary care in nine European countries.
Eur J Cardiovasc Prev Rehabil, 15 (2008), pp. 509-515
[166]J. Perk, B.G. de Backer, H. Gohlke, I. Graham, Z. Reiner, M. Verschuren, C. Albus, P. Benlian, G. Boysen, R. Cifkova, C. Deaton, S. Ebrahim, M. Fisher, G. Germano, R. Hobbs, A. Hoes, S. Karadeniz, A. Mezzani, E. Prescott, L. Ryden, M. Scherer, M. Syvanne, W.J. Scholte op Reimer, C. Vrints, D. Wood, J.L. Zamorano, F. Zannad.
European Guidelines on cardiovascular disease prevention in clinical practice (version 2012) The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR).
Eur Heart J, 33 (2012), pp. 1635-1701
[167]C. Falces, R. Andrea, M. Heras, C. Vehí, M. Sorribes, L. Sanchis, J. Cevallos, I. Menacho, S. Porcar, D. Font, M. Sabaté, J. Brugada.
Integración entre cardiología y atención primaria: impacto sobre la práctica clínica.
Rev Esp Cardiol, 64 (2011), pp. 564-571
[168]D.A. Wood, K. Kotseva, S. Connolly, C. Jennings, A. Mead, J. Jones, A. Holden, D. De Bacquer, T. Collier, G. De Backer, O. Faergeman.
EUROACTION Study Group, on behalf of EUROACTION Study Group. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomized controlled trial.
[169]C.K. Chow, S. Jolly, P. Rao-Melacini, K.A. Fox, S.S. Anand, S. Yusuf.
Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes.
Circulation, 121 (2010), pp. 750-758
[170]D.J. Kumbhani, G.C. Fonarow, C.P. Cannon, A.F. Hernandez, E.D. Peterson, W.F. Peacock, W.K. Laskey, P. Deedwania, M. Grau-Sepulveda, L.H. Schwamm, D.L. Bhatt.
Get With the Guidelines Steering Committee and Investigators. Temporal trends for secondary prevention measures among patients hospitalized with coronary artery disease. Temporal trends for secondary prevention measures among patients hospitalized with coronary artery disease.
Am J Med, 128 (2015), pp. e1-e9
[171]M.F. Piepoli, U. Corrà, S. Adamopoulos, W. Benzer, B. Bjarnason-Wehrens, M. Cupples, P. Dendale, P. Doherty, D. Gaita, S. Höfer, H. McGee, M. Mendes, J. Niebauer, N. Pogosova, E. Garcia-Porrero, B. Rauch, J.P. Schmid, P. Giannuzzi.
Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A Policy Statement from the Cardiac Rehabilitation Section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology.
Eur J Prev Cardiol, 21 (2012), pp. 664-681
[172]Authors/Task Force MembersRydén L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL; ESC Committee for Practice Guidelines (CPG), Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document Reviewers, De Backer G, Sirnes PA, Ezquerra EA, Avogaro A, Badimon L, Baranova E, Baumgartner H, Betteridge J, Ceriello A, Fagard R, Funck-Brentano C, Gulba DC, Hasdai D, Hoes AW, Kjekshus JK, Knuuti J, Kolh P, Lev E, Mueller C, Neyses L, Nilsson PM, Perk J, Ponikowski P, Reiner Z, Sattar N, Schächinger V, Scheen A, Schirmer H, Strömberg A, Sudzhaeva S, Tamargo JL, Viigimaa M, Vlachopoulos C, Xuereb RG. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013; 34:3035-3087.
[173]R. Estruch, E. Ros, J. Salas-Salvadó, M.I. Covas, D. Corella, F. Arós, E. Gómez-Gracia, V. Ruiz-Gutiérrez, M. Fiol, J. Lapetra, R.M. Lamuela-Raventos, L. Serra-Majem, X. Pintó, J. Basora, M.A. Muñoz, J.V. Sorlí, J.A. Martínez, M.A. Martínez-González.
PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet.
N Engl J Med, 368 (2013), pp. 1279-1290
[174]European Association for Cardiovascular Prevention & RehabilitationReiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D, ESC Committee for Practice Guidelines (CPG) 2008-2010 and 2010-2012 Committees. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011; 32:1769-1818.
[175]K. Kotseva, D. Wood, G. De Backer, D. De Bacquer.
EUROASPIRE III Study Group. Use and effects of cardiac rehabilitation in patients with coronary heart disease: results from the EUROASPIRE III survey.
Eur J Prev Cardiol, 20 (2013), pp. 817-826
[176]L.F. Hamm, B.K. Sanderson, P.A. Ades, K. Berra, L.A. Kaminsky, J.L. Roitman, M.A. Williams.
Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update: position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation.
J Cardiopulm Rehabil Prev, 31 (2011), pp. 2-10
[177]S.C. Smith Jr., E.J. Benjamin, R.O. Bonow, L.T. Braun, M.A. Creager, B.A. Franklin, R.J. Gibbons, S.M. Grundy, L.F. Hiratzka, D.W. Jones, D.M. Lloyd-Jones, M. Minissian, L. Mosca, E.D. Peterson, R.L. Sacco, J. Spertus, J.H. Stein, K.A. Taubert.
World Heart Federation and the Preventive Cardiovascular Nurses Association. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation.
Circulation, 124 (2011), pp. 2458-2473
[178]A. Kulik, M. Ruel, H. Jneid, B. Ferguson, L.F. Hiratzka, J.S. Ikonomidis, F. Lopez-Jimenez, S.M. McNallan, M. Patel, V. Roger, F.W. Sellke, D. Sica.
Zimmerman L, on behalf of the American Heart Association Council on Cardiovascular Surgery and Anesthesia. Secondary prevention after coronary artery bypass graft surgery a scientific statement from the American Heart Association.
Circulation, 131 (2015), pp. 927-964
[179]R.H. Eckel, J.M. Jakicic, J.D. Ard, J.M. de Jesus, N. Houston Miller, V.S. Hubbard, I.M. Lee, A.H. Lichtenstein, C.M. Loria, B.E. Millen, C.A. Nonas, F.M. Sacks, S.C. Smith Jr., L.P. Svetkey, T.A. Wadden, S.Z. Yanovski, K.A. Kendall, L.C. Morgan, M.G. Trisolini, G. Velasco, J. Wnek, J.L. Anderson, J.L. Halperin, N.M. Albert, B. Bozkurt, R.G. Brindis, L.H. Curtis, D. DeMets, J.S. Hochman, R.J. Kovacs, E.M. Ohman, S.J. Pressler, F.W. Sellke, W.K. Shen, S.C. Smith Jr., G.F. Tomaselli.
American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
Circulation, 129 (2014), pp. S76-S99
[180]N.J. Stone, J.G. Robinson, A.H. Lichtenstein, C.N. Bairey Merz, C.B. Blum, R.H. Eckel, A.C. Goldberg, D. Gordon, D. Levy, D.M. Lloyd-Jones, P. McBride, J.S. Schwartz, S.T. Shero, S.C. Smith Jr., K. Watson, P.W. Wilson, K.M. Eddleman, N.M. Jarrett, K. LaBresh, L. Nevo, J. Wnek, J.L. Anderson, J.L. Halperin, N.M. Albert, B. Bozkurt, R.G. Brindis, L.H. Curtis, D. DeMets, J.S. Hochman, R.J. Kovacs, E.M. Ohman, S.J. Pressler, F.W. Sellke, W.K. Shen, S.C. Smith Jr., G.F. Tomaselli.
American College ofCardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
Circulation, 129 (2014), pp. S1-S45
[181]D.M. Shahian, S.M. O’Brien, S.L. Normand, E.D. Peterson, F.H. Edwards.
Association of hospital coronary artery bypass volume with processes of care, mortality, morbidity, and the Society of Thoracic Surgeons composite quality score.
J Thorac Cardiovasc Surg, 139 (2010), pp. 273-282
[182]Society for Cardiothoracic Surgery In Great Britain And Ireland. Results of surgery in England as compare with other European countries.
www.scts.org/ (20 July 2015).
[184]González-Vílchez F, Gómez-Bueno M, Almenar L, Crespo-Leiro MG, Arizón JM, Martínez-Sellés M, Delgado J, Roig E, Lage E, Manito N, on behalf of the Spanish Heart Transplant Teams for the Spanish Heart Transplantation Registry. 24th Official Report of the Spanish Society of Cardiology Working Group on Heart Failure and Heart Transplantation (1984-2012). Rev Esp Cardiol 2013; 66:973-982.
[185]I. Ferreira-González, J.R. Marsal, F. Mitjavila, A. Parada, A. Ribera, P. Cascant, N. Soriano, P.L. Sánchez, F. Arós, M. Heras, H. Bueno, J. Marrugat, J. Cuñat, E. Civeira, G. Permanyer-Miralda.
Patient registries of acute coronary syndrome: assessing or biasing the clinical real world data?.
Circ Cardiovasc Qual Outcomes, 2 (2009), pp. 540-547
[186]Bufalino V, Bauman MA, Shubrook JH, Balch AJ, Boone C, Vennum K, Bradley S, Wender RC, Minners R, Arnett D, on behalf of the American Cancer Society, American Diabetes Association, and American Heart Association. Evolution of ‘The Guideline Advantage’ lessons learned from the front lines of outpatient performance measurement. Circ Cardiovasc Qual Outcomes 2014; 7:493-498.