To analyse non-work-related sickness absence (NWR-SA) due to inguinal hernia and the factors related to its duration, paying particular attention to the pre-surgical period of NWR-SA.
Materials and methodsA prospective cohort study was conducted on 1003 workers with an episode of NWR-SA due to an inguinal hernia, belonging to the insured population of a mutual insurance company. We assessed the duration of the NWR-SA episodes and the main demographic, occupational and clinical variables potentially related to it. Cox regression analyses were conducted to establish the predictors of NWR-SA duration.
ResultsThe mean duration of NWR-SA due to inguinal hernia was 68.6 days. After multivariate analysis (Cox regression), having a pre-surgical period of NWR-SA (HR=0.35; 95%CI, 0.28–0.43), manual occupations (HR=0.68; 95%CI, 0.49–0.95), construction sector (HR=0.71; 95%CI, 0.58–0.88), direct payment methods by a Mutual Insurance Company during sick leave in self-employed workers (HR=0.58; 95%CI, 0.41–0.82), or employees (HR=0.51; 95%CI, 0.36–0.72), comorbidity (HR=0.45; 95%CI, 0.34–0.59), and surgery performed under an entity other than the Public Health System or a Mutual Insurance Company (HR=0.76; 95%CI, 0.59–0.97) was associated with longer NWR-SA. With a Mutual Insurance Company the surgery was always performed with a pre-surgery period of NWR-SA (mean duration=47±39.6days); this was associated with shorter periods of post-surgical NWR-SA (P=.001).
ConclusionsThe NWR-SA due to inguinal hernia is a multifactorial phenomenon in which the pre-surgery period plays an important role. The collaboration between organisations involved in the management of NWR-SA seems to be an effective strategy for reducing its duration.
Analizar la incapacidad temporal por contingencias comunes (ITCC) debida a hernia inguinal y los factores relacionados con su duración, prestando especial atención al periodo pre-quirúrgico de ITCC.
Material y métodosEstudio de una cohorte prospectiva de 1.003 trabajadores con un episodio de ITCC por hernia inguinal, pertenecientes a la población protegida de una mutua de accidentes de trabajo y enfermedades profesionales. Se evaluaron la duración de la ITCC y las principales variables demográficas, laborales y clínicas potencialmente relacionadas con esta. Se establecieron predictores de la duración de la ITCC mediante regresión de Cox.
ResultadosLa duración media de la ITCC por hernia inguinal fue de 68,6 días. Tras el análisis multivariante, tener periodo pre-quirúrgico de ITCC (HR=0,35; IC 95%: 0,28-0,43), ocupaciones manuales (HR=0,68; IC 95%: 0,49–0,95), sector Construcción (HR=0,71; IC 95%: 0,58–0,88), modalidad de pago directo por la mutua en trabajadores por cuenta propia (HR=0,58; IC 95%: 0,41–0,82) o ajena (HR=0,51; IC 95%: 0,36–0,72), presencia de comorbilidad (HR=0,45; IC 95%: 0,34–0,59) y realización de la cirugía por una entidad distinta del Sistema Público de Salud o la mutua (HR=0,76; IC 95%: 0,59-0,97) se asociaron con bajas más largas. La mutua realizó la cirugía, siempre en presencia de periodo de ITCC pre-quirúrgica (duración media=47±39,6 días); asociándose periodos de ITCC post-quirúrgica más breves (p=0,001).
ConclusionesLa ITCC por hernia inguinal es un fenómeno multifactorial en el que el periodo pre-quirúrgico desempeña un papel importante. La colaboración entre entidades implicadas en la gestión de la ITCC parece resultar una estrategia efectiva para reducir su duración.
Temporary incapacity to work due to common contingencies (ITCC) is covered under our Social Security system to provide financial benefits to workers registered under the system who are temporarily unable to continue their work due to a non-work-related health problem.1 Mutual insurance companies for work-related accidents and illnesses work with the Social Security to manage these benefits from the sixteenth day of sick leave for companies who opt for this setup,2 offering their specialist resources to assess a worker's inability to work through periodic follow-up appointments and providing diagnostic tests or treatment to hasten a solution to the health problem and bring the worker back to work. These possibilities are particularly important as the healthcare resources of the public health system (SPS) are overburdened with general healthcare resulting in downtime as a consequence of unnecessary waiting during the ITCC process.3,4
Inguinal hernia is a common problem5 and its surgical treatment is amongst the most frequent in general surgery.6 Hernia repair usually causes periods of ITCC and rather than being considered a “simple procedure,” it is now one which should be studied in depth in order to improve aspects such as the patient's return to work,7,8 since the convalescence period is of considerable interest both socioeconomically and in terms of health management.6 Several standards and recommendations have been suggested in this regard, but these vary significantly.9–11
Research to date suggests the return to work would be earlier after laparoscopy than after open surgery,8,9,12,13 and amongst self-employed14 and younger workers.13 By contrast, manual occupations,13,15 lower educational levels,15 lower incomes,15 certain types of insurance coverage16 and previous symptoms of depression15 may be associated with longer periods of ITCC. Workers’ expectations in relation to the sick leave have also been highlighted as a significant predictive factor.17
However, many of the abovementioned findings originate from socio-economical and cultural contexts which are different to our own8,9,13,16 and focus exclusively on recovery after surgery. Factors in relation to the presurgical period, such as waiting list times,3 have not as yet been researched.
The objective of this study was to analyse the duration of ITCC due to inguinal hernia and the factors relating to its duration, paying particular attention to the role of the presurgical period within the episode of ITCC.
Materials and MethodsThis work formed part of a larger study about the duration of ITCC in relation to the most frequent illnesses and the factors predictive of its duration18 which was undertaken amongst the protected population of a mutual insurance company for work-related accidents and illnesses that work with the Social Security. The study methodology has been widely described elsewhere.2,18,19
DesignA prospective cohort and consecutive sampling design.
SubjectsThe sample for this study comprised 1003 subjects who had started an episode of ITCC sick leave due to a diagnosis of inguinal hernia (CIE-9-MC 550).20 The patients were monitored in person until the end of the episode.
VariablesA large number of variables were assessed during the patient interviews.
The study's dependent variable was the total duration of the episode of temporary incapacity (DTOT=return-to-work date−sick leave date+1). This was divided into 2 components:
- a.
Duration of the presurgical period (DPRE=date of operation−sick leave date).
- b.
Duration after surgery (DPOST=return-to-work date−date of operation+1).
The following were used as covariables:
- -
Socio-demographic: gender; age; level of education; nationality; marital status.
- -
Employment: activity sector; occupation (manual work, non-manual work); type of contract (temporary, indefinite); method of payment during sick leave (pago delegado (company paid benefit refunded by the Social Security) [corresponding to the General Social Security Scheme]; direct payment to the self-employed worker [self-employment]; direct payment to the employed worker [unemployment during sick leave]); level of income (regulatory base used to calculate financial benefits during ITCC, categorised under 4 levels).
- -
Clinical and administrative: whether or not there was a presurgical ITCC period; comorbidities (co-diagnoses, mentioned by the patient during consultation and endorsed by a report from the public health services (SPS) or the mutual insurance company's own doctor); the entity performing the surgery (SPS; mutual insurance company; other, e.g. private insurance); location of the hernia (unilateral, bilateral); whether or not mesh was used during surgery.
Descriptive statistics were obtained for all the variables. The association of the covariables as to whether or not there had been a presurgical period (chi-square test) was analysed, and the durations of ITCC were compared according to them (Student's t-test; variance analysis). Finally a Cox regression model was constructed in stages, with DTOT as the variable criterion, which was adjusted depending on whether there had or had not been a presurgical period, and for the remaining covariables which were significantly associated with the duration of ITCC (DTOT, DPRE or DPOST). The association of a covariable with the duration of ITCC was expressed by means of hazard ratio (HR) and its confidence intervals (CI). HR<1 implied a lower likelihood of return to work and longer episodes of ITCC. The interaction between variables was not entered into the model. Compliance with each covariable's proportional hazards assumption was checked using log graphics (−log ST) against the follow-up time.
The SPSS v17.0 software was used for the statistical analysis.
Ethical AspectsThe study conformed to the Helsinki Declaration.
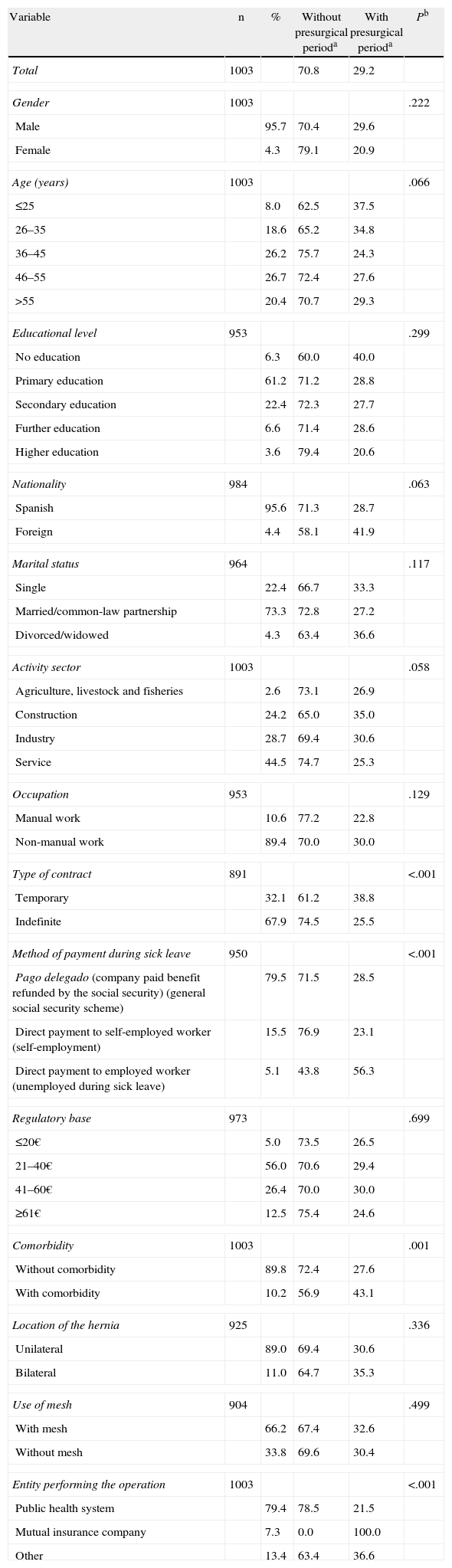
ResultsTable 1 shows the demographic, employment and clinical characteristics of the sample and the variables that were associated with a greater proportion of workers with a presurgical ITCC period.
Demographic, Employment and Clinical Characteristics of the Sample and the Likelihood of There Being a Presurgical Period During the Episode of Temporary Incapacity due to Common Contingencies.
| Variable | n | % | Without presurgical perioda | With presurgical perioda | Pb |
| Total | 1003 | 70.8 | 29.2 | ||
| Gender | 1003 | .222 | |||
| Male | 95.7 | 70.4 | 29.6 | ||
| Female | 4.3 | 79.1 | 20.9 | ||
| Age (years) | 1003 | .066 | |||
| ≤25 | 8.0 | 62.5 | 37.5 | ||
| 26–35 | 18.6 | 65.2 | 34.8 | ||
| 36–45 | 26.2 | 75.7 | 24.3 | ||
| 46–55 | 26.7 | 72.4 | 27.6 | ||
| >55 | 20.4 | 70.7 | 29.3 | ||
| Educational level | 953 | .299 | |||
| No education | 6.3 | 60.0 | 40.0 | ||
| Primary education | 61.2 | 71.2 | 28.8 | ||
| Secondary education | 22.4 | 72.3 | 27.7 | ||
| Further education | 6.6 | 71.4 | 28.6 | ||
| Higher education | 3.6 | 79.4 | 20.6 | ||
| Nationality | 984 | .063 | |||
| Spanish | 95.6 | 71.3 | 28.7 | ||
| Foreign | 4.4 | 58.1 | 41.9 | ||
| Marital status | 964 | .117 | |||
| Single | 22.4 | 66.7 | 33.3 | ||
| Married/common-law partnership | 73.3 | 72.8 | 27.2 | ||
| Divorced/widowed | 4.3 | 63.4 | 36.6 | ||
| Activity sector | 1003 | .058 | |||
| Agriculture, livestock and fisheries | 2.6 | 73.1 | 26.9 | ||
| Construction | 24.2 | 65.0 | 35.0 | ||
| Industry | 28.7 | 69.4 | 30.6 | ||
| Service | 44.5 | 74.7 | 25.3 | ||
| Occupation | 953 | .129 | |||
| Manual work | 10.6 | 77.2 | 22.8 | ||
| Non-manual work | 89.4 | 70.0 | 30.0 | ||
| Type of contract | 891 | <.001 | |||
| Temporary | 32.1 | 61.2 | 38.8 | ||
| Indefinite | 67.9 | 74.5 | 25.5 | ||
| Method of payment during sick leave | 950 | <.001 | |||
| Pago delegado (company paid benefit refunded by the social security) (general social security scheme) | 79.5 | 71.5 | 28.5 | ||
| Direct payment to self-employed worker (self-employment) | 15.5 | 76.9 | 23.1 | ||
| Direct payment to employed worker (unemployed during sick leave) | 5.1 | 43.8 | 56.3 | ||
| Regulatory base | 973 | .699 | |||
| ≤20€ | 5.0 | 73.5 | 26.5 | ||
| 21–40€ | 56.0 | 70.6 | 29.4 | ||
| 41–60€ | 26.4 | 70.0 | 30.0 | ||
| ≥61€ | 12.5 | 75.4 | 24.6 | ||
| Comorbidity | 1003 | .001 | |||
| Without comorbidity | 89.8 | 72.4 | 27.6 | ||
| With comorbidity | 10.2 | 56.9 | 43.1 | ||
| Location of the hernia | 925 | .336 | |||
| Unilateral | 89.0 | 69.4 | 30.6 | ||
| Bilateral | 11.0 | 64.7 | 35.3 | ||
| Use of mesh | 904 | .499 | |||
| With mesh | 66.2 | 67.4 | 32.6 | ||
| Without mesh | 33.8 | 69.6 | 30.4 | ||
| Entity performing the operation | 1003 | <.001 | |||
| Public health system | 79.4 | 78.5 | 21.5 | ||
| Mutual insurance company | 7.3 | 0.0 | 100.0 | ||
| Other | 13.4 | 63.4 | 36.6 | ||
ITCC: temporary incapacity due to common contingencies (ITCC); P: P-value associated with the value of the chi-squared statistic; presurgical period: period of time prior to surgery, during the ITCC episode.
The percentage of patients with a presurgical ITCC period was significantly higher when the contracts were temporary, in the direct payment method during sick leave for self-employed workers (unemployment during the sick leave) and when a comorbidity was present (P<.01). A presurgical ITCC period was also associated with the entity performing the surgery. At all times when there was a presurgical ITCC period, the mutual insurance company became involved in the process and took charge of the surgery. In these cases, the mean duration of the presurgical period was 47 days (±39.6; Table 2).
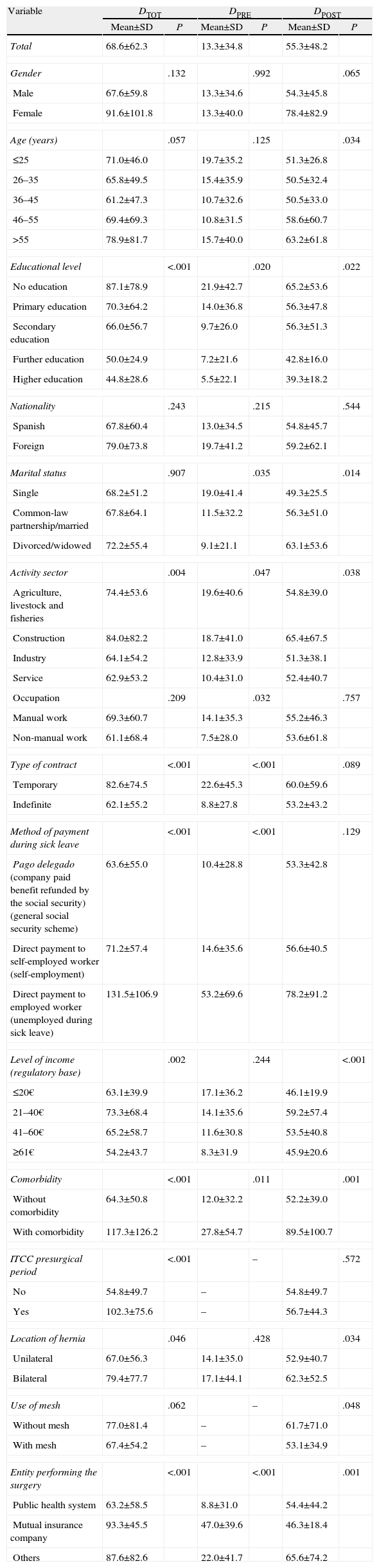
Bivariate Association of Demographic, Employment and Clinical Variables With the Total Duration of Temporary Incapacity due to Common Contingencies, the Presurgical Period and the Duration of the Period After Surgery.
| Variable | DTOT | DPRE | DPOST | |||
| Mean±SD | P | Mean±SD | P | Mean±SD | P | |
| Total | 68.6±62.3 | 13.3±34.8 | 55.3±48.2 | |||
| Gender | .132 | .992 | .065 | |||
| Male | 67.6±59.8 | 13.3±34.6 | 54.3±45.8 | |||
| Female | 91.6±101.8 | 13.3±40.0 | 78.4±82.9 | |||
| Age (years) | .057 | .125 | .034 | |||
| ≤25 | 71.0±46.0 | 19.7±35.2 | 51.3±26.8 | |||
| 26–35 | 65.8±49.5 | 15.4±35.9 | 50.5±32.4 | |||
| 36–45 | 61.2±47.3 | 10.7±32.6 | 50.5±33.0 | |||
| 46–55 | 69.4±69.3 | 10.8±31.5 | 58.6±60.7 | |||
| >55 | 78.9±81.7 | 15.7±40.0 | 63.2±61.8 | |||
| Educational level | <.001 | .020 | .022 | |||
| No education | 87.1±78.9 | 21.9±42.7 | 65.2±53.6 | |||
| Primary education | 70.3±64.2 | 14.0±36.8 | 56.3±47.8 | |||
| Secondary education | 66.0±56.7 | 9.7±26.0 | 56.3±51.3 | |||
| Further education | 50.0±24.9 | 7.2±21.6 | 42.8±16.0 | |||
| Higher education | 44.8±28.6 | 5.5±22.1 | 39.3±18.2 | |||
| Nationality | .243 | .215 | .544 | |||
| Spanish | 67.8±60.4 | 13.0±34.5 | 54.8±45.7 | |||
| Foreign | 79.0±73.8 | 19.7±41.2 | 59.2±62.1 | |||
| Marital status | .907 | .035 | .014 | |||
| Single | 68.2±51.2 | 19.0±41.4 | 49.3±25.5 | |||
| Common-law partnership/married | 67.8±64.1 | 11.5±32.2 | 56.3±51.0 | |||
| Divorced/widowed | 72.2±55.4 | 9.1±21.1 | 63.1±53.6 | |||
| Activity sector | .004 | .047 | .038 | |||
| Agriculture, livestock and fisheries | 74.4±53.6 | 19.6±40.6 | 54.8±39.0 | |||
| Construction | 84.0±82.2 | 18.7±41.0 | 65.4±67.5 | |||
| Industry | 64.1±54.2 | 12.8±33.9 | 51.3±38.1 | |||
| Service | 62.9±53.2 | 10.4±31.0 | 52.4±40.7 | |||
| Occupation | .209 | .032 | .757 | |||
| Manual work | 69.3±60.7 | 14.1±35.3 | 55.2±46.3 | |||
| Non-manual work | 61.1±68.4 | 7.5±28.0 | 53.6±61.8 | |||
| Type of contract | <.001 | <.001 | .089 | |||
| Temporary | 82.6±74.5 | 22.6±45.3 | 60.0±59.6 | |||
| Indefinite | 62.1±55.2 | 8.8±27.8 | 53.2±43.2 | |||
| Method of payment during sick leave | <.001 | <.001 | .129 | |||
| Pago delegado (company paid benefit refunded by the social security) (general social security scheme) | 63.6±55.0 | 10.4±28.8 | 53.3±42.8 | |||
| Direct payment to self-employed worker (self-employment) | 71.2±57.4 | 14.6±35.6 | 56.6±40.5 | |||
| Direct payment to employed worker (unemployed during sick leave) | 131.5±106.9 | 53.2±69.6 | 78.2±91.2 | |||
| Level of income (regulatory base) | .002 | .244 | <.001 | |||
| ≤20€ | 63.1±39.9 | 17.1±36.2 | 46.1±19.9 | |||
| 21–40€ | 73.3±68.4 | 14.1±35.6 | 59.2±57.4 | |||
| 41–60€ | 65.2±58.7 | 11.6±30.8 | 53.5±40.8 | |||
| ≥61€ | 54.2±43.7 | 8.3±31.9 | 45.9±20.6 | |||
| Comorbidity | <.001 | .011 | .001 | |||
| Without comorbidity | 64.3±50.8 | 12.0±32.2 | 52.2±39.0 | |||
| With comorbidity | 117.3±126.2 | 27.8±54.7 | 89.5±100.7 | |||
| ITCC presurgical period | <.001 | – | .572 | |||
| No | 54.8±49.7 | – | 54.8±49.7 | |||
| Yes | 102.3±75.6 | – | 56.7±44.3 | |||
| Location of hernia | .046 | .428 | .034 | |||
| Unilateral | 67.0±56.3 | 14.1±35.0 | 52.9±40.7 | |||
| Bilateral | 79.4±77.7 | 17.1±44.1 | 62.3±52.5 | |||
| Use of mesh | .062 | – | .048 | |||
| Without mesh | 77.0±81.4 | – | 61.7±71.0 | |||
| With mesh | 67.4±54.2 | – | 53.1±34.9 | |||
| Entity performing the surgery | <.001 | <.001 | .001 | |||
| Public health system | 63.2±58.5 | 8.8±31.0 | 54.4±44.2 | |||
| Mutual insurance company | 93.3±45.5 | 47.0±39.6 | 46.3±18.4 | |||
| Others | 87.6±82.6 | 22.0±41.7 | 65.6±74.2 | |||
SD: standard deviation; DPOST: duration of the period post-surgery, result of subtracting the date of surgery plus one day from the return-to-work date; DPRE: duration of the presurgical period during the episode of ITCC, result of subtracting the sick leave date from the date of surgery; DTOT: total duration of the episode of ITCC, result of subtracting the date of sick leave from the return-to-work date and adding one day; ITCC: temporary incapacity due to common contingencies (ITCC); P-value: associated with the bivariate analyses of the durations according to the patient's demographic, employment and clinical variables: Student's t-test for the dichotomous covariables and variance analysis of a factor for the covariables with more than 2 levels.
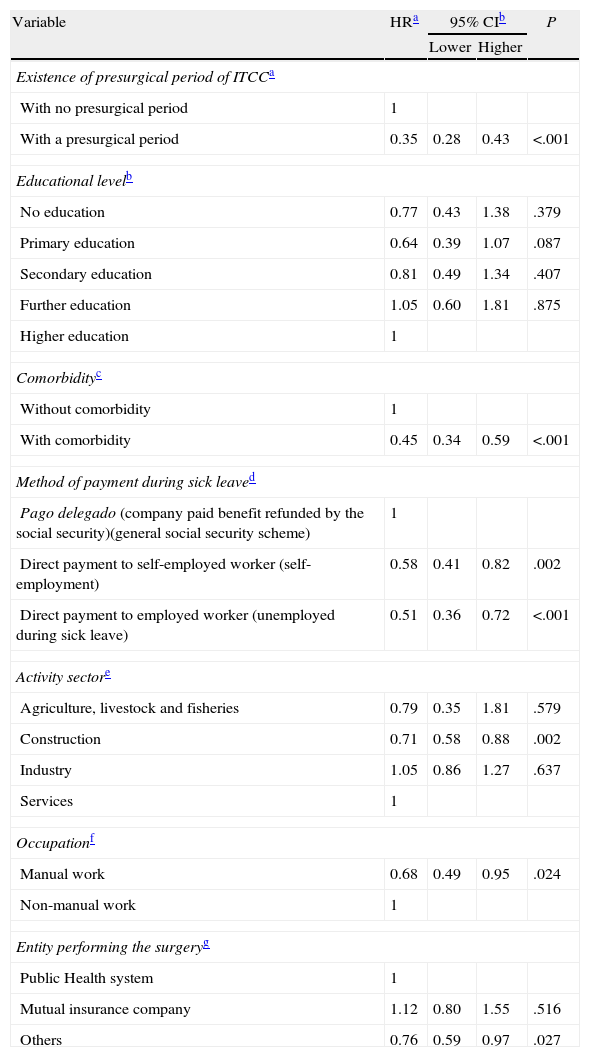
Table 2 shows the results of the bivariate analyses of the duration of ITCC according to the demographic, employment and clinical variables studied. Once the multivariate analysis was adjusted by all the predictors which were significantly associated with the total duration or one of its components–construction workers vs service sector workers, manual workers, those receiving direct payment from the mutual insurance company (workers who were unemployed during the sick leave and self-employed workers), the presence of comorbidities, the existence of a presurgical ITCC period and the surgery having been performed by an entity other than the SPS or the mutual insurance company – they were associated with a longer final duration of the episode (Table 3).
Adjusted Association of Demographic, Employment and Clinical Variables, With the Duration of the Temporary Incapacity due to Common Contingencies, Calculated Using a Cox Regression Model in Stages (Forwards).
| Variable | HRa | 95% CIb | P | |
| Lower | Higher | |||
| Existence of presurgical period of ITCCa | ||||
| With no presurgical period | 1 | |||
| With a presurgical period | 0.35 | 0.28 | 0.43 | <.001 |
| Educational levelb | ||||
| No education | 0.77 | 0.43 | 1.38 | .379 |
| Primary education | 0.64 | 0.39 | 1.07 | .087 |
| Secondary education | 0.81 | 0.49 | 1.34 | .407 |
| Further education | 1.05 | 0.60 | 1.81 | .875 |
| Higher education | 1 | |||
| Comorbidityc | ||||
| Without comorbidity | 1 | |||
| With comorbidity | 0.45 | 0.34 | 0.59 | <.001 |
| Method of payment during sick leaved | ||||
| Pago delegado (company paid benefit refunded by the social security)(general social security scheme) | 1 | |||
| Direct payment to self-employed worker (self-employment) | 0.58 | 0.41 | 0.82 | .002 |
| Direct payment to employed worker (unemployed during sick leave) | 0.51 | 0.36 | 0.72 | <.001 |
| Activity sectore | ||||
| Agriculture, livestock and fisheries | 0.79 | 0.35 | 1.81 | .579 |
| Construction | 0.71 | 0.58 | 0.88 | .002 |
| Industry | 1.05 | 0.86 | 1.27 | .637 |
| Services | 1 | |||
| Occupationf | ||||
| Manual work | 0.68 | 0.49 | 0.95 | .024 |
| Non-manual work | 1 | |||
| Entity performing the surgeryg | ||||
| Public Health system | 1 | |||
| Mutual insurance company | 1.12 | 0.80 | 1.55 | .516 |
| Others | 0.76 | 0.59 | 0.97 | .027 |
95% CI: 95% confidence interval; ITCC: temporary incapacity due to common contingencies; HR: adjusted hazard ratio; HR>1: greater likelihood of return to work, lower duration of ITCC; HR<1: lower probability of return to work, greater duration of ITCC
Our data indicate that the mean duration of sick leave due to inguinal hernia is in excess of 2 months, and approximately 3 out of every 10 patients start their sick leave prior to surgery. This is very much higher than available standards.9–11 Periods of presurgical ITCC, far from being brief, can even exceed the recovery time required after surgery.
Although these presurgical periods of ITCC and the duration of the ITCC might be largely linked to the type of work the worker does or with the presence of comorbidities, other factors appear to be associated to a greater extent with unstable contractual conditions and it is possible that ITCC is being used as a “recourse” benefit for problems other than those it is meant to cover (e.g. type of contract, method of payment). This multiplicity of factors matches previous studies.13–16 The data presented on the presurgical period of ITCC due to inguinal hernia raise issues in terms of health management. It is worth considering, in the absence of other medical conditions, that a period of ITCC prior to hernia repair as lengthy as that described in this study might not be justified medically. Hernias could have been present for years, and can be fully compatible with normal activity. Recent reviews in this same regard call into question whether available scientific evidence would lead to the conclusion that, in the absence of any previous vulnerability, mechanical occupational exposure could, on its own, cause a hernia and whether an early return to work after its surgical repair can be associated with a greater risk of recurrence.21,22
Our findings regarding the real situation of ITCC due to inguinal hernia are also very far removed from the recommendations on resuming fully normal activity after repair from a surgical point of view. The European Hernia Society indicate that it is not necessary to temporarily stop lifting loads, taking part in sports or work after hernia surgery. According to this clinical practice guide, probably a limitation on heavy weight lifting for 2–3 weeks is enough.6 In Spain, consensus work by expert surgeons, using the Delphi technique, reached unanimity on proposing a standard return-to-work time of 30 days for work requiring physical effort and 21 days if the work is sedentary.11 In any event, the data obtained in the present study highlight the need for scientific knowledge, and expert recommendations with regard to resuming normal activity in the context of surgical hernia repair should be transferred to the areas of healthcare and primary health care management and the mutual insurance companies for work-related accidents and illnesses. The scope for action in this regard extends from training or knowledge dissemination activities to the inclusion in the discharge summary after surgery of specific recommendations on resuming activity. Previous studies have shown that these specific recommendations on the part of the surgeon regarding a short period of convalescence after the operation have been shown to be an efficient strategy for encouraging a return to work.17 It is clear that those who manage the processes of ITCC due to inguinal repair (primary health care doctors and doctors from the mutual insurance companies for work-related accidents and illnesses) need to thoroughly review the medical justification for this situation being extended longer than the weeks immediately following surgery.
The results regarding the entity performing the surgery are of particular interest. Our data suggest that the patient's health care itinerary within the SPS for the most part works efficiently. However, a significant number of patients are given sick leave well before it is possible to perform the surgery and they have to wait in this situation without being able to return to work. The mutual insurance company provides their own care resources for this particular subgroup of patients. The results of the analysis of the ITCC components reveal that, once the presurgical period has been eliminated, the recovery times of patients operated under the mutual insurance companies are even lower than when the surgery is performed by other entities. Therefore, the intervention of the mutual insurance company appears to be an effective strategy towards patient recovery and towards bringing the ITCC process to an end.
Among the strengths of this study is the fact that this was a prospective study with well-planned and highly structured data collection, and that the role of the presurgical period in this type of process is an aspect which has hardly been studied.
One of the main limitations of the study concerned the sample selection: workers who were being followed up by a mutual insurance company because of an episode of ITCC. Nevertheless, it is worth highlighting that the majority of the working population are covered by mutual insurance companies for work-related accidents and illnesses in this regard.2,3 Furthermore, it is desirable that future research should include variables such as the expectations of patients themselves, the specific type of surgery, whether the hernias are recurrent and a detailed analysis of comorbidities.
In conclusion, in order to be able to understand ITCC for inguinal hernias, variables other than clinical variables need to be considered, which include a far broader socio-labour context and efficient management of the patient's healthcare itinerary.
FundingResearch into the area of social protection was financed by a grant received under Order TIN/1902/2009 of 10 July (awards for the Promotion of Research into Social Protection–FIPROS–).
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ruiz-Moraga M, Catalina-Romero C, Martínez-Muñoz P, Cobo-Santiago MD, González-López M, Cabrera-Sierra M, et al. Periodo prequirúrgico y duración de la incapacidad temporal por contingencias comunes en la hernia inguinal. Cir Esp. 2014;92:269–276.