95% of pancreatic tumors are epithelial; adenocarcinoma represents 85%–95% and neuroendocrine tumors <5% of primary neoplasms. Non-epithelial and non-neuroendocrine tumors are extremely rare (<0.1%).1
Treatment for malignant periampullary tumors involves pancreaticoduodenectomy (PD), when the aim is curative intent, or palliative care and symptom relief when there is locally unresectable or disseminated disease.
The objective of this communication is to present the case of a patient who underwent surgery for primary sarcoma of the head of the pancreas.
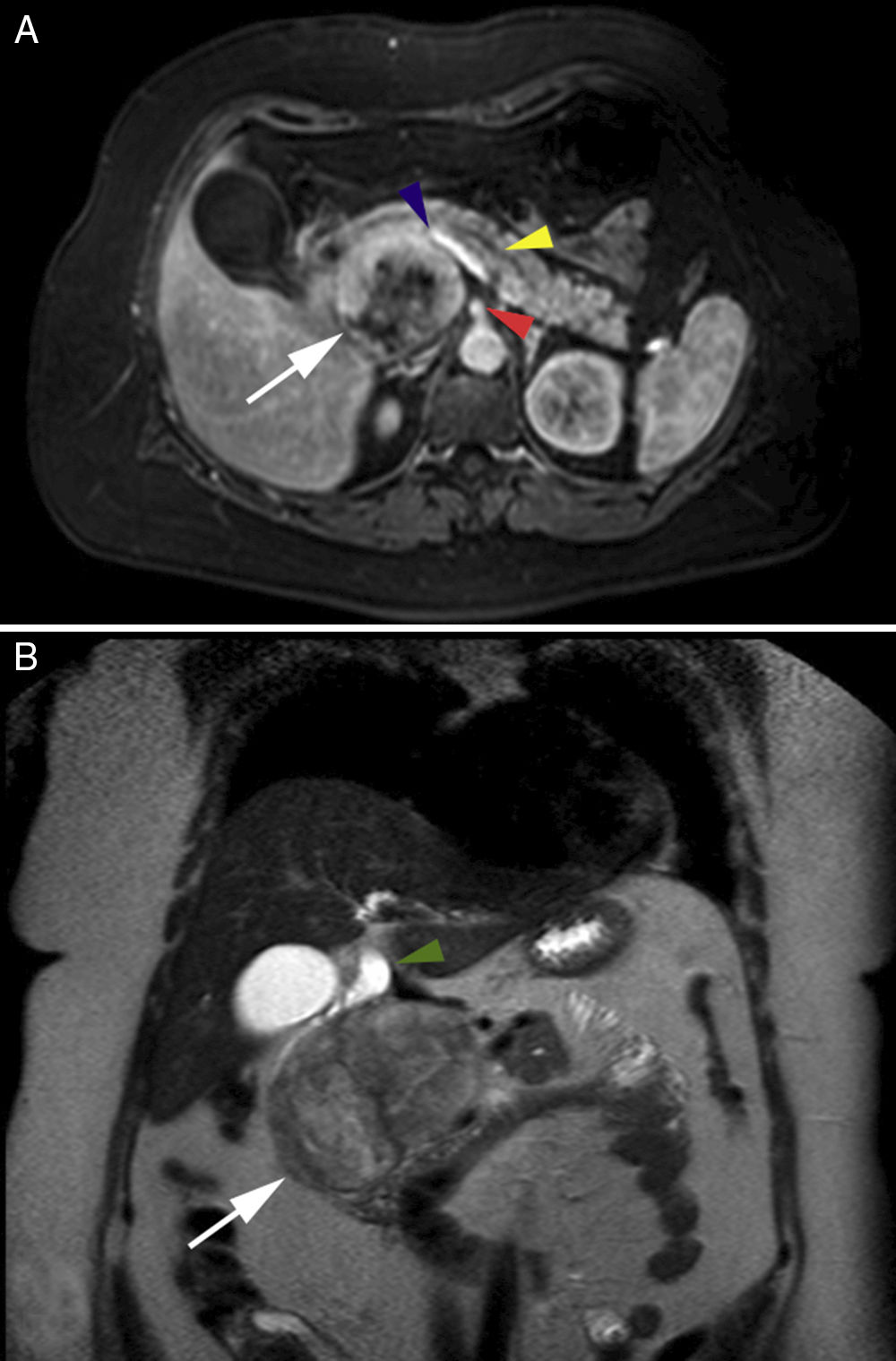
The patient is a 50-year-old woman with a medical history of Guillain-Barré syndrome, cesarean section and laparoscopic total hysterectomy due to cervical adenocarcinoma. She reported 2 weeks of jaundice and choluria, with no abdominal pain or weight loss. Examination revealed jaundice of the skin and mucous membranes, with a soft abdomen that was painless and presented no palpable masses. The altered hepatic profile showed: total bilirubin 6.7mg/dL, direct bilirubin 5.5mg/dL, alkaline phosphatase 840μ/L, GGT 547μ/L, GOT 254μ/L and GPT 410μ/L. Abdominal ultrasound showed a mass measuring 7.7cm×7.2cm×6.9cm that projected toward the head of the pancreas, with dilatation of the extrahepatic bile duct but no changes to the intrahepatic duct, diffuse hepatic steatosis or cholelithiasis. Thoracic, abdominal and pelvic computed tomography scans with contrast showed a well-demarcated right retroperitoneal perirenal mass in contact with the rear of the uncinate process of the pancreas, but giving the impression of a primary retroperitoneal mass; the bile duct was slightly dilated. Magnetic resonance imaging with gadolinium demonstrated a solid, cystic, heterogeneous tumor that appeared to originate in the head of the pancreas and the uncinate process, in contact with the superior mesenteric artery and the splenic–mesenteric–portal axis, with no vascular invasion (Fig. 1) but compressing the bile duct, whose extrahepatic segment was dilated (Fig. 1B).
(A) Axial magnetic resonance image showing retroperitoneal location of the lesion (white arrow), superior mesenteric artery (arrowhead), splenic–mesenteric–portal axis (arrowhead), dilated Wirsung duct (arrowhead); (B) Coronal magnetic resonance image with gadolinium showing heterogeneous characteristics of the lesion (white arrow) and the dilated bile duct (arrowhead).
The case was discussed in a multidisciplinary committee. Given the characteristics of the lesion (solid-cystic, heterogeneous, well-defined, large tumor size with a capsule image during the preoperative study, and symptomatic), we decided that there was no need to perform preoperative endosonography with needle aspiration or preoperative biliary drainage. With a preoperative diagnosis of pseudopapillary tumor of the pancreas, a disease typical of younger women, a PD was scheduled.
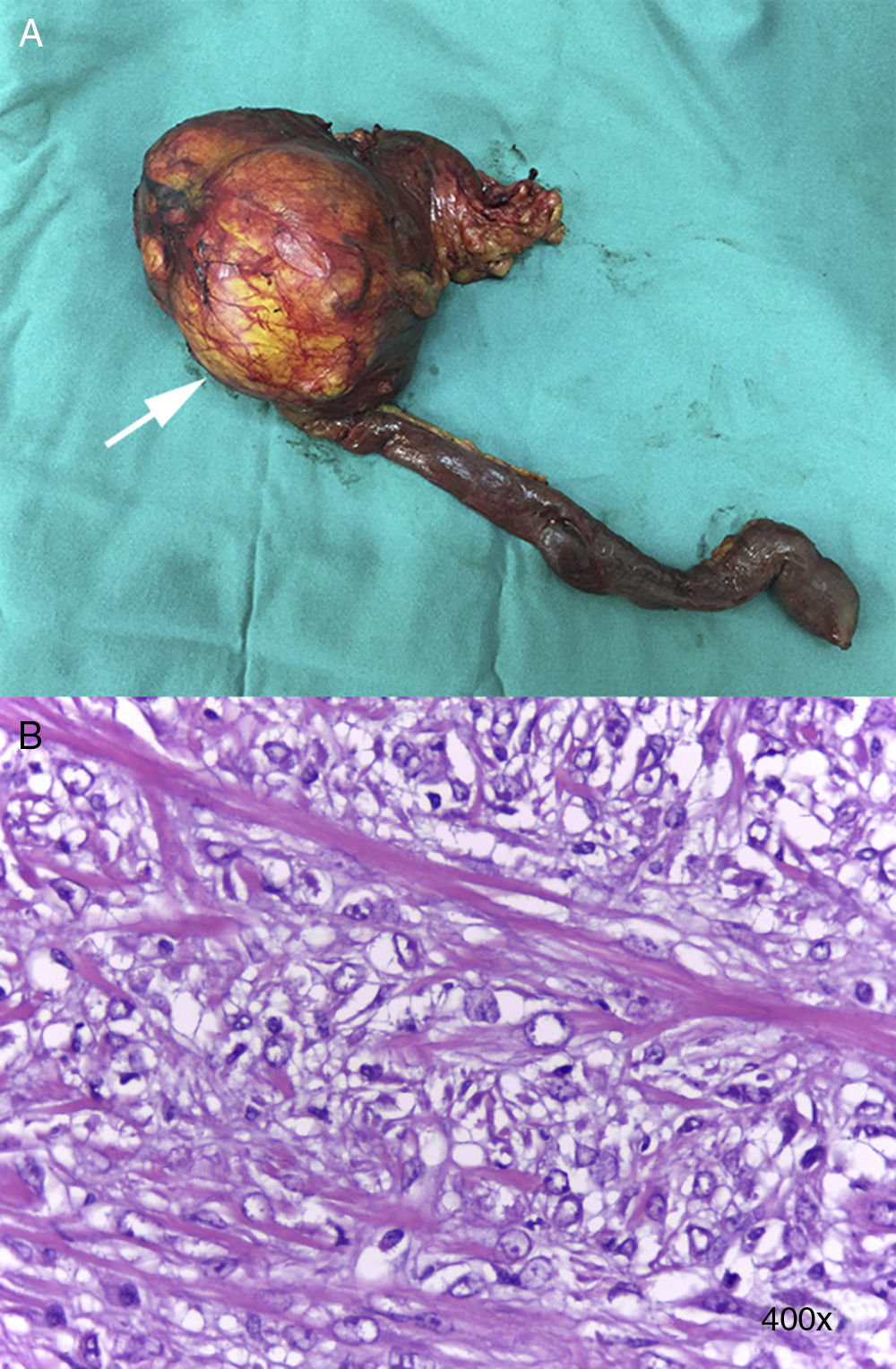
A supra- and infraumbilical midline laparotomy was performed, and the cavity was explored, finding no carcinomatosis. Palpation of the head of the pancreas detected a tumor measuring approximately 12cm in diameter in the uncinate process; the pancreas was hard and slightly atrophic, with a distended gallbladder. PD was performed with Child's loop reconstruction, duct-to-mucosa pancreaticojejunostomy with a transanastomotic stent (Blumgart technique), hepatic-jejunal anastomosis and end-to-side antecolic gastrointestinal anastomosis, leaving in 2 Jackson-Pratt® drains (Fig. 2A).
In the postoperative period, a type B pancreatic fistula (ISGPS2 classification2) developed, which was managed with intravenous antibiotics, providing a positive clinical response. The patient was discharged on the 8th postoperative day with oral antibiotics and a Jackson-Pratt® drain, which was withdrawn on the 14th postoperative day.
The histopathology study confirmed a well-defined tumor in the head of the pancreas (10×7cm) that was stromal in appearance and compatible with low-grade myofibroblastic sarcoma (G1), no perineural, vascular or lymphatic infiltration with free surgical margins, and 23 lymph nodes with no evidence of neoplasia (Fig. 2B). Immunohistochemistry for smooth muscle actin, S100, CD34, CD117, ALK and desmin was negative; Ki-67 (20%) and vimentin were positive, thereby confirming the diagnosis of myofibroblastic sarcoma. During the postoperative evaluation, we decided not to perform complementary treatments. The patient is currently under follow-up, showing no evidence of recurrence after 12 months.
Primary sarcomas of the pancreas are infrequent neoplasms that do not reach 300 reported cases.3 Most are found in the body or tail of the pancreas, and preoperative radiological diagnosis usually focuses on more common lesions, such as neuroendocrine or solid pseudopapillary tumors of the pancreas,3 as in our case.
Similar to other mesenchymal or visceral mesenchymal tumors, the treatment of primary sarcomas of the pancreas is surgical when the disease is localized. Neoplasm-free margins are an important prognostic factor for locoregional recurrence. In this type of tumors, radical surgeries would seem to be more indicated than conservative ones. However, this is not supported by scientific evidence because, as stated, the most relevant descriptive series do not exceed 20 cases.3
Clinical guidelines for the treatment of soft tissue and visceral sarcomas by the European Society of Medical Oncology (ESMO) do not recommend adjuvant radiotherapy in localized disease and complete resection; instead, it is recommended in lesions >5cm deep that are high-grade (G2-3) after resection with adequate surgical margins.4 To determine the risk for recurrence of this type of tumors, the degree of differentiation, tumor size, margin involvement and the extension of the resection should be considered identify exceptions to this recommendation. Primary sarcomas of the pancreas have a lower incidence of lymph node metastases than ductal adenocarcinoma, and the prognosis is much better with 5-year survival rates of 41%–50% in resected tumors.5
Please cite this article as: Muñoz Castro C, Sepulveda Diaz G, San Pedro Sánchez A, Lahsen Humeres JP. Sarcoma primario de páncreas: una indicación infrecuente de duodenopancreatectomía cefálica. Cir Esp. 2018;96:521–523.