Esophagectomy remains a procedure associated with major complications and a significant risk of mortality.1 Rates of complications reflect a combination of factors including appropriate selection of surgery, technical expertise, and standards of perioperative care.2 Complications are the single greatest factors of increasing resource utilization and costs after the treatment of esophageal cancer.3 Accurate measurement of postoperative complications is necessary to allow comparisons between surgeons and centers to be made, to inform data synthesis (meta-analyses), and to provide patients with information for decision-making.2 If outcomes are not accurately defined, measured and reported, estimates may be misleading resulting in outcome reporting bias.
In a systematic review on over 57,000 esophagectomies, Blencowe and colleagues2 found that no single complication was reported in all papers, and less than 40% of the studies provided a precise definition of complications. Anastomotic leak was commonly reported (81%) but using 22 different definitions. Severity grading was used in less than one third of cases although in all instances these were simply divided into minor or major categories. Even mortality itself may be misleading because, if only 30-day mortality is reported, this may underestimate the actual mortality rate by a factor of 4 compared with in-hospital mortality or 90-day mortality.4,5 Attempts to develop the definitions and grade of complications for specific procedures are lacking, with the exception of a consensus for the definition of pancreatic fistula and delayed gastric emptying after pancreatic surgery by the International Study Group of Pancreatic Surgery (ISGPS) in recent years.6,7
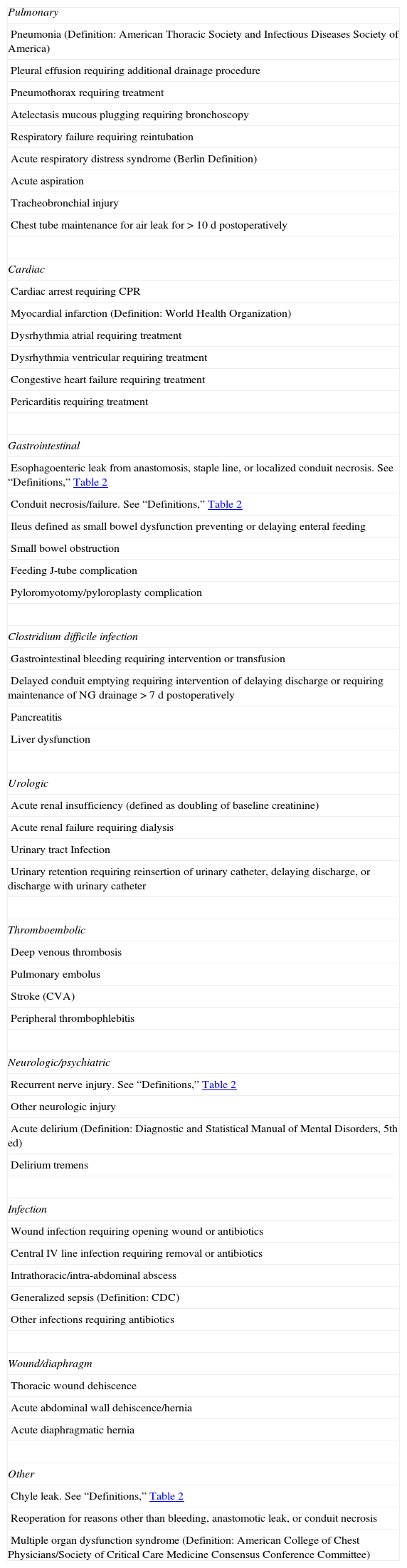
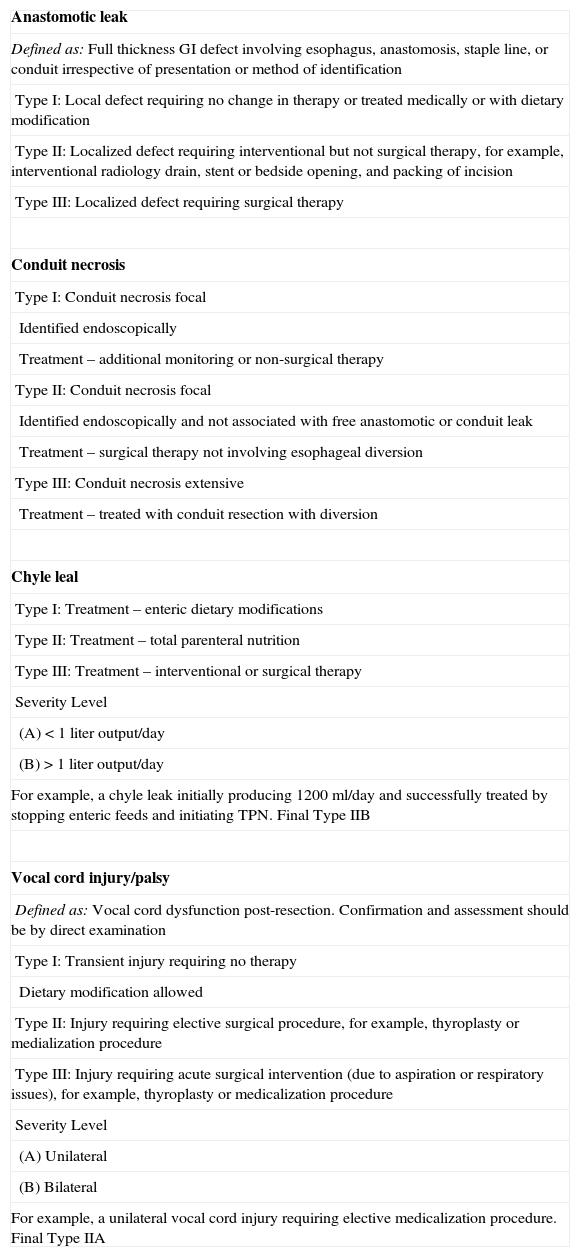
A study recently published in Annals of Surgery8 by Donald Low and the Esophagectomy Complications Consensus Group (ECCG) entitled “International consensus on standardization of data collection for complications associated with esophagectomy” represents the first consistent project within a surgical specialty whereby 21 experienced surgeons from 14 countries arrived at a consensus on a standard definition of complications and quality measures to consider after esophagectomy by means of Delphi surveys and group meetings. A standardized list of possible complications is given in the first Table 1 below (with permission of Annals of Surgery). Other information that should not be overlooked when reporting the outcomes of esophagectomy are severity stratification with the Dindo-Clavien system, hospital readmissions, changes in level of care (returning to ICU), blood utilization and destination on discharge. Another issue addressed by the ECCG involved constructing simple but clinically meaningful definitions of 4 common “surgical complications”: anastomotic leak, conduit necrosis, chyle leak, and vocal cord palsy, as shown in the second Table 2 below (with permission of Annals of Surgery).
Complications Basis Platform.
| Pulmonary |
| Pneumonia (Definition: American Thoracic Society and Infectious Diseases Society of America) |
| Pleural effusion requiring additional drainage procedure |
| Pneumothorax requiring treatment |
| Atelectasis mucous plugging requiring bronchoscopy |
| Respiratory failure requiring reintubation |
| Acute respiratory distress syndrome (Berlin Definition) |
| Acute aspiration |
| Tracheobronchial injury |
| Chest tube maintenance for air leak for > 10 d postoperatively |
| Cardiac |
| Cardiac arrest requiring CPR |
| Myocardial infarction (Definition: World Health Organization) |
| Dysrhythmia atrial requiring treatment |
| Dysrhythmia ventricular requiring treatment |
| Congestive heart failure requiring treatment |
| Pericarditis requiring treatment |
| Gastrointestinal |
| Esophagoenteric leak from anastomosis, staple line, or localized conduit necrosis. See “Definitions,” Table 2 |
| Conduit necrosis/failure. See “Definitions,” Table 2 |
| Ileus defined as small bowel dysfunction preventing or delaying enteral feeding |
| Small bowel obstruction |
| Feeding J-tube complication |
| Pyloromyotomy/pyloroplasty complication |
| Clostridium difficile infection |
| Gastrointestinal bleeding requiring intervention or transfusion |
| Delayed conduit emptying requiring intervention of delaying discharge or requiring maintenance of NG drainage > 7 d postoperatively |
| Pancreatitis |
| Liver dysfunction |
| Urologic |
| Acute renal insufficiency (defined as doubling of baseline creatinine) |
| Acute renal failure requiring dialysis |
| Urinary tract Infection |
| Urinary retention requiring reinsertion of urinary catheter, delaying discharge, or discharge with urinary catheter |
| Thromboembolic |
| Deep venous thrombosis |
| Pulmonary embolus |
| Stroke (CVA) |
| Peripheral thrombophlebitis |
| Neurologic/psychiatric |
| Recurrent nerve injury. See “Definitions,” Table 2 |
| Other neurologic injury |
| Acute delirium (Definition: Diagnostic and Statistical Manual of Mental Disorders, 5th ed) |
| Delirium tremens |
| Infection |
| Wound infection requiring opening wound or antibiotics |
| Central IV line infection requiring removal or antibiotics |
| Intrathoracic/intra-abdominal abscess |
| Generalized sepsis (Definition: CDC) |
| Other infections requiring antibiotics |
| Wound/diaphragm |
| Thoracic wound dehiscence |
| Acute abdominal wall dehiscence/hernia |
| Acute diaphragmatic hernia |
| Other |
| Chyle leak. See “Definitions,” Table 2 |
| Reoperation for reasons other than bleeding, anastomotic leak, or conduit necrosis |
| Multiple organ dysfunction syndrome (Definition: American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference Committee) |
Definitions.
| Anastomotic leak |
| Defined as: Full thickness GI defect involving esophagus, anastomosis, staple line, or conduit irrespective of presentation or method of identification |
| Type I: Local defect requiring no change in therapy or treated medically or with dietary modification |
| Type II: Localized defect requiring interventional but not surgical therapy, for example, interventional radiology drain, stent or bedside opening, and packing of incision |
| Type III: Localized defect requiring surgical therapy |
| Conduit necrosis |
| Type I: Conduit necrosis focal |
| Identified endoscopically |
| Treatment – additional monitoring or non-surgical therapy |
| Type II: Conduit necrosis focal |
| Identified endoscopically and not associated with free anastomotic or conduit leak |
| Treatment – surgical therapy not involving esophageal diversion |
| Type III: Conduit necrosis extensive |
| Treatment – treated with conduit resection with diversion |
| Chyle leal |
| Type I: Treatment – enteric dietary modifications |
| Type II: Treatment – total parenteral nutrition |
| Type III: Treatment – interventional or surgical therapy |
| Severity Level |
| (A) < 1 liter output/day |
| (B) > 1 liter output/day |
| For example, a chyle leak initially producing 1200ml/day and successfully treated by stopping enteric feeds and initiating TPN. Final Type IIB |
| Vocal cord injury/palsy |
| Defined as: Vocal cord dysfunction post-resection. Confirmation and assessment should be by direct examination |
| Type I: Transient injury requiring no therapy |
| Dietary modification allowed |
| Type II: Injury requiring elective surgical procedure, for example, thyroplasty or medialization procedure |
| Type III: Injury requiring acute surgical intervention (due to aspiration or respiratory issues), for example, thyroplasty or medicalization procedure |
| Severity Level |
| (A) Unilateral |
| (B) Bilateral |
| For example, a unilateral vocal cord injury requiring elective medicalization procedure. Final Type IIA |
*Does not include elective insertion of additional surgical or interventional chest drains.
GI indicates gastrointestinal; TPN, total parenteral nutrition.
In this short time since the publication of the paper, the complications platform and the quality measures as well as the definitions have already been reviewed by one subspecialty (Society of Thoracic Surgeons), and one national database (Netherlands). It is being considered for inclusion in two additional national databases, as well as the EURECCA Upper GI project. It is also currently being utilized in the Neo-AEGIS international trial comparing neoadjuvant chemotherapy versus chemoradiotherapy in the treatment of esophageal cancer. A website (www.esodata.org) has recently been developed for data collection for the beta test of the ECCG complications project. This is the first attempt that we are aware of to collect international data prospectively in any type of surgical subspecialty. This project can set a precedent, to establish a new methodology for conducting international prospective assessments. We are aware that other subspecialties are also interested in developing a similar project for their specific diseases.
The outcomes of the ECCG project were presented to the International Society for Diseases of the Esophagus (ISDE) executive in 2015. It is currently planned that the results of the Beta test will be presented at the ISDE Biannual meeting in 2016. Ultimately, it is hoped that additional prospective international studies will be done using the website but under the auspices of a committee of the ISDE.
Centralization of esophageal and gastric cancer surgery in Spain is already a reality in Catalonia and Navarra. Since 2011 the EURECCA Upper GI project is collecting the outcomes of these procedures in both autonomous communities and there is agreement to use this new set of complications definitions for reporting the results in the coming future. There is no doubt that with the increasingly implementation of audits to assess surgical outcomes after complex procedures and the emergence of better designed surgical trials it will become mandatory that standardized complications reporting criteria be established for specific complex procedures as we now have available for esophagectomy.
Please cite this article as: Pera M, Low DE. Consenso para definir y dar a conocer las complicaciones de la esofagectomía: un paso importante para la utilización de un lenguaje común. Cir Esp. 2015;93:549–551.