Technical failure in pancreas transplant has been the main cause of the loss of grafts. In the last few years, the number of complications has reduced, and therefore the proportion of this problem.
ObjectivesThe Spanish Pancreas Transplant Group wanted to analyze the current situation with regard to surgical complications and their severity.
Materials and methodsA retrospective and multicenter study was performed. 10 centers participated, with a total of 410 pancreas transplant recipients between January and December 2013.
ResultsA total of 316 transplants were simultaneous with kidney, 66 after kidney, pancreas-only 10, 7 multivisceral and 11 retransplants. Surgical complication rates were 39% (n=161). A total of 7% vascular thrombosis, 13% bleeding, 6% the graft pancreatitis, 12% surgical infections and others to a lesser extent. Relaparotomy rate was 25%. The severity of complications were of type IIIb (13%), type II (12%), and type IVa (8.5%). Graft loss was 8%. Early mortality was 0.5%. The percentage of operations for late complications was 17%.
ConclusionsThe number of surgical complications after transplantation is not negligible, affecting one in 3 patients. They are severe in one out of 5 and, in one of every 10 patients graft loss occurs. Therefore, there are still a significant percentage of surgical complications in this type of activity, as shown in our country.
El fracaso técnico en el trasplante de páncreas ha sido el principal responsable de la pérdida de los injertos. Desde hace unos años, el número de complicaciones se han reducido, y por tanto, la proporción de este problema.
ObjetivosEl Grupo Español del Trasplante de Páncreas se plantea como objetivo de este estudio analizar la situación actual con relación a las complicaciones quirúrgicas y su gravedad.
Material y métodosSe ha realizado un estudio retrospectivo y multicéntrico con 10 centros participantes, con un total de 410 pacientes trasplantados de páncreas entre enero de 2008 y diciembre de 2013.
ResultadosUn total de 316 trasplantes fueron simultáneos con riñón, 66 después de riñón, 10 solo de páncreas, 7 multiviscerales y 11 retrasplantes. El porcentaje de complicaciones quirúrgicas fue del 39% (161 pacientes). Un 7% de trombosis vasculares, 13% de hemorragias, 6% de pancreatitis del injerto, 12% de infecciones quirúrgicas y otras en menor proporción. Las reintervenciones alcanzaron el 25%. La gravedad de las complicaciones fueron del tipo iiib (13%), del tipo ii (12%) y del tipo iva (8,5%). La pérdida del injerto fue del 8%. La mortalidad precoz del 0,5%. Las operaciones por complicaciones tardías fueron el 17%.
ConclusionesEl número de complicaciones quirúrgicas tras el trasplante no es desdeñable: afectan a uno de cada 3 pacientes, son graves en uno de cada 5 y con pérdida del injerto en uno de cada 10 pacientes. Por tanto, sigue existiendo un porcentaje significativo de complicaciones quirúrgicas en este tipo de actividad, como se demuestra en nuestro país.
Pancreas transplantation (PT) is the only method able to restore normoglycemia in patients with diabetes mellitus.
In February 1983 at the Hospital Clínic in Barcelona, the first simultaneous pancreas-kidney transplantation was performed in Spain. From then and until 2013, a total of 1454 PT have been performed in our country.1 Since December 2010, more than 35000 PT have been registered in the International Pancreas Transplant Registry (IPTR).2
In recent decades, advances made in immunosuppressant treatment have gone hand-in-hand with a decrease in postoperative complications, improved surgical technique and, ultimately, better graft and patient survival.
Nonetheless, technical failure (TF), which has always been the most critical factor in PT, still plays an important role in the results and reveals the inherent problems of this type of surgery. TF is defined as early graft loss due to factors that are not related with immunological problems, and it is responsible for the loss of most transplanted organs during the first year.3 But, as reported by Humar et al., it seems that the number of surgical complications has decreased in recent years and, therefore, so has TF.4
ObjectivesThe main objective of this study by the Spanish Pancreas Transplant Group is to analyze the current situation of abdominal surgical complications, their severity and the proportion of TF.
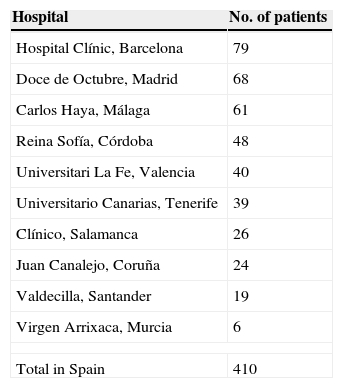
Materials and MethodsWe carried out a nation-wide retrospective, multicenter study with 10 participating hospitals (Table 1), including a total of 410 patients who were treated by PT between January 2008 and December 2013.
Spanish Hospitals With Pancreas Transplant Programs That Have Collaborated With this Study.
| Hospital | No. of patients |
|---|---|
| Hospital Clínic, Barcelona | 79 |
| Doce de Octubre, Madrid | 68 |
| Carlos Haya, Málaga | 61 |
| Reina Sofía, Córdoba | 48 |
| Universitari La Fe, Valencia | 40 |
| Universitario Canarias, Tenerife | 39 |
| Clínico, Salamanca | 26 |
| Juan Canalejo, Coruña | 24 |
| Valdecilla, Santander | 19 |
| Virgen Arrixaca, Murcia | 6 |
| Total in Spain | 410 |
The following data were compiled in a database (SPSS, version 11.0 for Windows) for further study: number of patients, age, sex, types of PT, early complications (≤30 days) and their severity, reinterventions, graft transplantectomies, early mortality (≤30 days), and late onset complications.
The surgical technique was not completely uniform, which is logical due to the number of transplant units at different centers. Along general lines, it entailed the following:
- 1.
80% of the pancreatic grafts were obtained simultaneously along with the liver by the same team. In 60% of cases, Celsior® solution was used as a preservation fluid.
- 2.
During graft preparation, most groups advocate a duodenal length of 5 to 10cm in order to obtain a well vascularized bowel. Likewise, in 80% of cases, duodenal dissection was performed with an autosuture device, and the staple line was reinforced with invaginating sutures to avoidleaks.
- 3.
The approach used to implant the pancreas in the recipient was supra- and infraumbilical midline laparotomy in all cases except for 2 groups in which an independent approach was used for the kidney. Last of all, the graft was implanted with the duodenum in the proximal position, and the tail of the pancreas was distal.
- 4.
Venous drainage to the inferior vena cava was the standard technique used.
- 5.
With the exception of one group, all the transplant units used the iliac artery grafts from the donor for the arterial vascular reconstruction.
- 6.
Enteric bypass of pancreatic exocrine secretions was done universally.
- 7.
Complete anticoagulation with heparin after graft reperfusion was used in only 3 transplant groups.
- 8.
All groups maintained at least one drain after surgery.
The descriptive statistical study of the frequencies included: central tendency with the determination of sums, means (if normal distribution), and medians; and dispersion with standard deviation with maximum and minimum values. Likewise, the percentages of the different manifestations were calculated, along with their degrees of severity.
ResultsA total of 316 PT were done simultaneously in conjunction with the kidney, 66 after the kidney, 10 pancreas-only, 7 multi-organ, and 11 retransplantation. Mean age was 38 (23–59) and the patients were predominantly male (68.7%).
161 surgical complications (39.2%) were diagnosed and categorized as follows:
- -
Vascular thrombosis: present in 29 patients (7%), 62% of which were venous and 27.6% arterial. In 3 patients (10.4%), the type could not be determined due to massive graft necrosis.
- -
Hemorrhage: present in 52 patients (12.7%). In 30 cases, bleeding was intraabdominal (57.7%), and 20 of these cases were early (≤30 days). Nine cases were gastrointestinal (17.3%), and in 13 patients the location was not specified (25%).
- -
Graft pancreatitis due to ischemia-reperfusion affected 25 patients (6%). When classified in accordance with the 2012 Atlanta classification,5 11 were mild, 10 moderate-severe and 4 acute.
- -
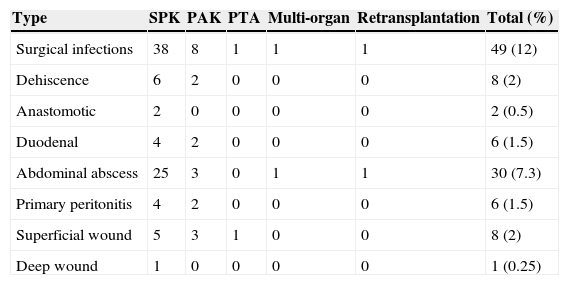
Intra-abdominal surgical infections (Table 2) were present in 49 patients (12%). In 8 cases (2%), they were caused by suture dehiscence (6 at the duodenal closure, and 2 at the intestinal duodenal anastomosis). A total of 30 patients presented intraabdominal abscess (7.3%), with no relation with previous fistulas. Primary peritonitis was seen in 6 cases (1.5%) and wound infections in 9 (2.2%).
Table 2.Infectious Complications After the Abdominal Surgery for Different Pancreas Transplant Types.
Type SPK PAK PTA Multi-organ Retransplantation Total (%) Surgical infections 38 8 1 1 1 49 (12) Dehiscence 6 2 0 0 0 8 (2) Anastomotic 2 0 0 0 0 2 (0.5) Duodenal 4 2 0 0 0 6 (1.5) Abdominal abscess 25 3 0 1 1 30 (7.3) Primary peritonitis 4 2 0 0 0 6 (1.5) Superficial wound 5 3 1 0 0 8 (2) Deep wound 1 0 0 0 0 1 (0.25) PAK: pancreas-after-kidney transplantation; PTA: pancreas transplant alone; SPK: simultaneous pancreas-kidney transplantation.
- -
Pancreatic fistula was observed in 7 recipients (1.7%): type A (n=1), type B (n=3), and type C (n=3).6
- -
Other complications were also observed, including: surgical wound dehiscence in 7 cases (1.7%), intestinal obstruction due to adhesions in 6 patients, one case of arterial graft pseudoaneurysm, and one lymphocele.
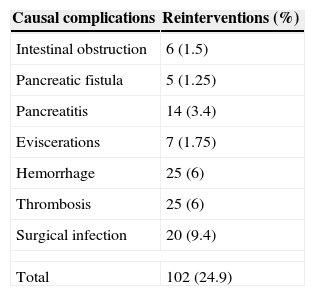
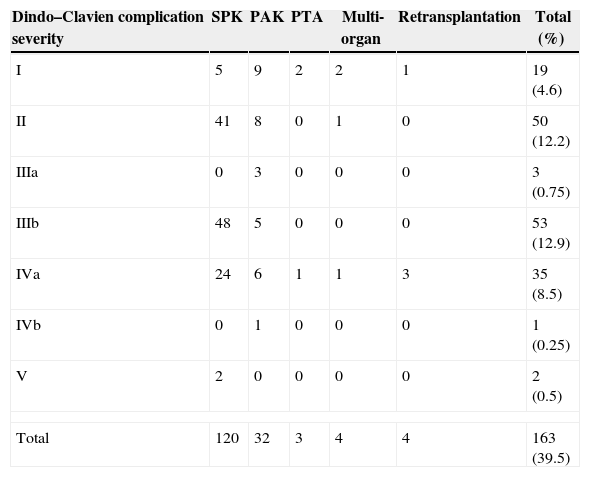
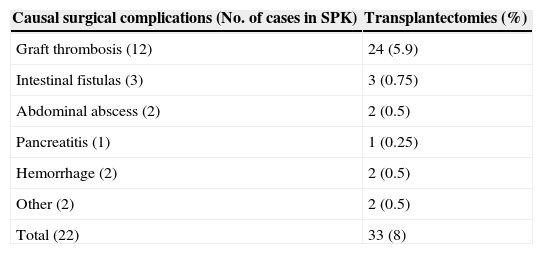
Reoperations were required in 102 patients (24.9%) (Table 3). The severity of the complications was classified according to Dindo–Clavien,7 with 53 patients who were type IIIb (12.9%), 50 patients type II (12.2%) and 35 patients type IVa (8.5%) (Table 4). Surgical complications led to the loss of the graft in 33 patients (8%) (Table 5).
Severity of Surgical Complications According to the Dindo–Clavien Classification.
| Dindo–Clavien complication severity | SPK | PAK | PTA | Multi-organ | Retransplantation | Total (%) |
|---|---|---|---|---|---|---|
| I | 5 | 9 | 2 | 2 | 1 | 19 (4.6) |
| II | 41 | 8 | 0 | 1 | 0 | 50 (12.2) |
| IIIa | 0 | 3 | 0 | 0 | 0 | 3 (0.75) |
| IIIb | 48 | 5 | 0 | 0 | 0 | 53 (12.9) |
| IVa | 24 | 6 | 1 | 1 | 3 | 35 (8.5) |
| IVb | 0 | 1 | 0 | 0 | 0 | 1 (0.25) |
| V | 2 | 0 | 0 | 0 | 0 | 2 (0.5) |
| Total | 120 | 32 | 3 | 4 | 4 | 163 (39.5) |
PAK: pancreas-after-kidney transplantation; PTA: pancreas transplant alone; SPK: simultaneous pancreas-kidney transplantation.
Source: Dindo–Clavien.7
Causes of Graft Loss.
| Causal surgical complications (No. of cases in SPK) | Transplantectomies (%) |
|---|---|
| Graft thrombosis (12) | 24 (5.9) |
| Intestinal fistulas (3) | 3 (0.75) |
| Abdominal abscess (2) | 2 (0.5) |
| Pancreatitis (1) | 1 (0.25) |
| Hemorrhage (2) | 2 (0.5) |
| Other (2) | 2 (0.5) |
| Total (22) | 33 (8) |
SPK: simultaneous pancreas-kidney transplantation.
Two patients (0.5%) died prematurely: one as a result of sepsis secondary to pneumonia at 29 days post-op, and one intraoperative asystole of unknown cause.
We have also been able to analyze late complications (>30 days post-PT) in 302 transplants performed at 7 hospitals (excluding deaths and lost data). The causes of late surgical reoperations were: intraabdominal hemorrhage (n=10), collections or abscesses (n=9), graft pancreatitis (n=3), acute cholecystitis (n=1), incisional hernias (n=7) and intestinal obstruction (n=12). In total, the late reoperation rate was 17%.
DiscussionProper evaluation of the pancreas viability at the time of extraction from the donor is one of the basic pillars for obtaining good results in the recipient. It should invariably be accompanied by a correct surgical technique during organ extraction and implantation. In this regard, after having evaluated the different transplant groups, the surgical technique used was rather uniform in both donors as well as recipients.
As stated by Troppmann,8 during the 1980s PT complications resulted in a 25% loss of pancreatic grafts. In the following decades, however, we have witnessed a clear decrease in the percentage of these complications. In a PT analysis done in the United States between 2004 and 2008, a decrease in TF was observed, ranging from 7% to 9%.9 Nonetheless, these results have not been corroborated by other contemporary publications, which report relaparotomy rates from 24% to 35% and graft losses due to complications in up to 75%.9–12
In Spain, there has been a high rate of surgical complications (nearly 40%), but only 8% of TF, which are excellent results and similar to the review by Troppmann.9
The most frequent and severe surgical complications include:
Graft thrombosisThrombosis is still the most serious and frequent complication,13,14 affecting between 7% (in our experience) and 13% of PT. It usually appears in the first week,15 represents 70% of TF8 and is the main reason for relaparotomy and graft removal.3
Its etiology is multifactorial, although problems with the anastomosis are clearly a well-known cause.16 Other causes include: stasis of the splenic vessels, endothelial damage due to ischemia/reperfusion injuries and hypercoagulability.17 There are also donor-related factors: age over 50 or younger than 10, hemodynamic instability and cardiovascular death.18,19 Factors related with extraction include: mechanical aggression, excessive preservation fluid and pressure, and inadequate blood drainage.19 Factors related with the recipient include: single-organ transplants, peritoneal dialysis, enteric drainage,19,20 cellular rejection,21 graft pancreatitis,22 and thrombophilia syndromes.23,24
Transplantectomy is the standard treatment in cases of massive graft thrombosis, as has occurred in 6% of our Spanish series. Other less aggressive therapies have had limited success in some cases.20,25 What is interesting is early retransplantation in these cases, and if there is no infection, the results are excellent,26 as in our series.
Most Spanish transplant groups use prophylaxis with low molecular weight heparin (40mg/day). Only 3 groups use complete anticoagulation (1mg/kg of weight) with sodium heparin. Some international groups do not use these medications, with excellent results.12,17,27 Aspirin is also frequently used as a platelet antiaggregant12 in our setting.
Intra-Abdominal Surgical InfectionsThese infections are the most frequent cause of mortality within the first year.12,28 Anastomotic leaks affect between 9% and 14% of published cases,29 but the grafts are removed in only 0.5%.9 Abscesses or localized collections affect 14% of patients29; 30% are associated with suture dehiscence,8,30 and 80% are resolved with interventional radiology.
Wound infection is frequent (14%),16 although it is generally superficial and simple to resolve. Deep infections, however, must be treated seriously and with extensive debridement as they can lead to severe problems, such as graft loss and even patient death (as in one of our cases).
These processes have been related with older donors and recipients, retransplantation, peritoneal dialysis, cold ischemia time, graft pancreatitis, long waiting-list periods, more severe disease, and immunosuppression type.9,13,31
Graft PancreatitisWithin this entity, there is a physiological type29 that appears in 100% of PT as an acute inflammatory response during the first 72h. It is related with ischemia/reperfusion injuries and is usually silent in most cases.32 Protein C levels are elevated and the frequency of hyperamylasemia in this period reaches up to 35% of cases. A condition that we call “peripancreatitis” often arises, which causes fluid around the graft that is rich in amylase and lipase. In some cases, this can be associated with small leaks from the pancreatic parenchyma caused during surgery. It may resolve itself spontaneously or with the help of a surgical drain.16,22
Early graft pancreatitis within the first 3 months is observed in 35%–38% of cases.32 The severity of the process is equally difficult to standardize, although we believe that we should adopt the new Atlanta classification5 to standardize concepts. When severity is acute, the outcome is loss of the graft in some 78%–91% of cases,32 although the prognosis is relatively benign. Donor risk factors9 include: age, obesity, prolonged resuscitation, large inotrope requirements, ischemia/reperfusion syndrome, and prolonged periods of warm ischemia.33 Recipient risk factors9 are: improper graft management, accelerated/high pressure revascularization, poor papillary drainage, etc.
From a physiological standpoint, graft pancreatitis can be divided into 2 types32: one is related with infectious or immunological processes; the other is associated with the surgical process, such as graft thrombosis, which is responsible for 60%–70% of graft pancreatitis.21
Management should be conservative, as was applied in our series.
Pancreatic FistulasPancreatic fistulas are infrequent (5%).8 They are related with technical problems, fundamentally with duodenal perforations or suture deshiscence. As mentioned in the previous section, what is most frequent are small leaks from the pancreatic parenchyma caused by organ handling.16
HemorrhagesThis is the most frequent complication in the abdominal area that results in a higher number of relaparotomies. On the other hand, after surgical resolution, bleeding is a relatively benign process as less than 0.3% of grafts are lost.9
When the hemorrhage is gastrointestinal, it can originate at the duodenal sutures or the enteric anastomosis and it is usually self-limiting. Hemorrhages that are infectious in origin (such as cytomegalovirus), ischemic, or due to vascular-enteric fistulas are later and in many cases lead to the removal of the graft.9
Severity of the Complications (Dindo–Clavien)7This assessment is fundamental to determine the risk of the process and its implications. Most published articles refer to the complications that appear, but they do not clearly define their importance, except for TF. One-fifth of the complications observed in the study are resolved with medical treatment. Three cases required percutaneous radiological resolution of intraabdominal abscesses. In the group of reoperated patients, there was TF in less than 10%. Two patients died prematurely, which represents a low mortality rate.
Late ComplicationsLate complications result in a reoperation rate of 17%, including a high rate of intestinal obstructions that affected more than one-third of the population, as well as intraabdominal collections and incisional hernias, which were observed in 1 out of 5 patients.
The limitation of this study is that it is only focused on abdominal surgical complications and, therefore, we have not assessed the late graft function or long-term follow-up of the patients.
ConclusionsThe national percentage of surgical complications after pancreas transplantation is far from negligible: they affect 1 out of every 3 patients, are severe in 1 out of every 5, and lead to graft loss in 1 out of every 10 patients.
Therefore, contrary to what some international authors report,4,9 there is still a significant percentage of surgical complications in PT activity, as demonstrated in Spain.
Transplantation DataWe have followed the guidelines established by our respective healthcare centers to access the data from patient medical files for the completion of this publication and in order to disclose this information to the scientific community.
The authors have participated in the data acquisition and collection as well as the critical review and approval of the final version.
Conflict of InterestsThe authors explicitly declare having no conflict of interests.
Please cite this article as: Moya-Herraiz A, Muñoz-Bellvis L, Ferrer-Fábrega J, Manrique Municio A, Pérez-Daga JA, Muñoz-Casares C, et al. Estudio cooperativo del Grupo Español de Trasplante de Páncreas (GETP): complicaciones quirúrgicas. Cir Esp. 2015;93:300–306.
Information from this article was presented at the 3rd Meeting of the Spanish Pancreas Transplant Group, under the title “National experience with immediate complications after pancreas transplantation”, which was held on May 15–16, 2014 in Valencia.