Pyogenic liver abscesses usually have a biliary origin or are secondary to a septic focus that reaches the liver by either the portal or arterial route.1 Despite advances made in imaging studies and treatment, they are still a therapeutic challenge.2 There has been a recent increase in the incidence of liver abscesses caused by perforations of the gastrointestinal tract after the ingestion of foreign bodies. The first case was reported by Lambert in 1989, and since then about 60 cases have been published in the literature.2–4
This entity is a diagnostic challenge because accidental ingestions are often forgotten, and the non-specific symptoms can lead to a misdiagnosis of cryptogenic abscesses.5,6 Likewise, this etiology must be taken into account in the differential diagnosis of recurrent pyogenic liver abscesses.2
We present two clinical cases of liver abscesses secondary to perforation of the gastrointestinal tract by a fishbone.
Case 1. A 74-year-old woman with a history of arterial hypertension, diabetes mellitus and cholecystectomy presented with pain in the right renal fossa that radiated toward the right hypochondrium and a week-long fever. Percussion of the kidneys was positive, and lab work showed no alterations. On abdominal ultrasound, a heterogeneous lesion with multiple septa was observed in liver segment V, which was confirmed by computed tomography (CT) scan as a space-occupying lesion suggestive of a multi-walled abscess, measuring 10cm in diameter.
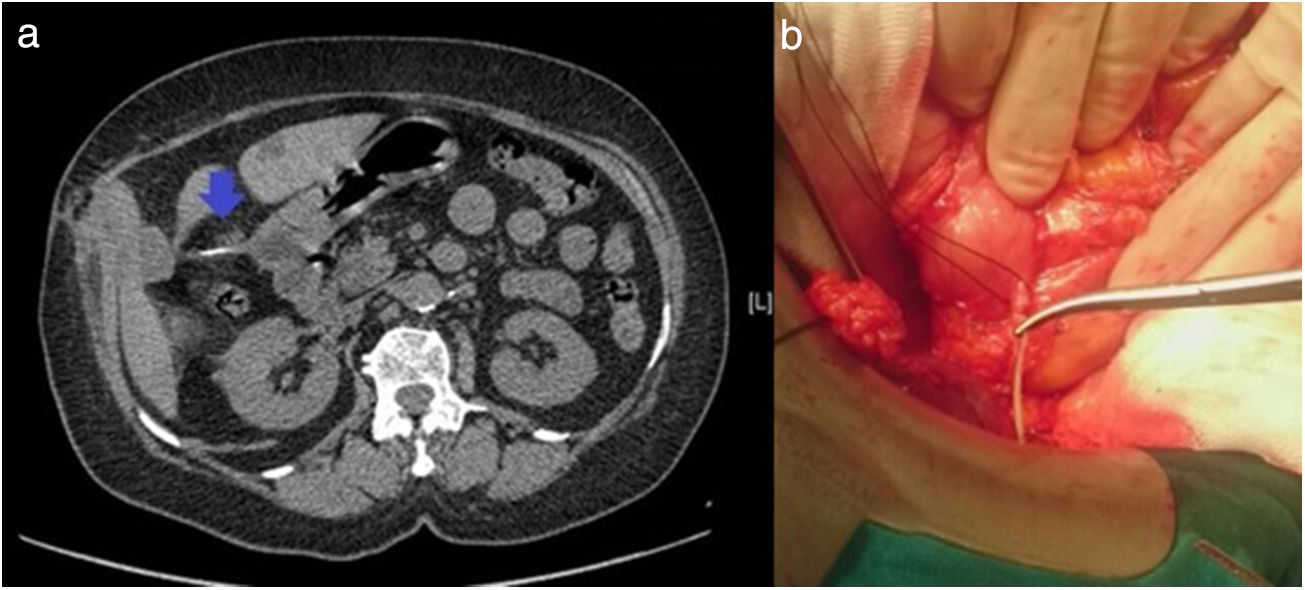
After empirical antibiotic therapy and percutaneous drainage, the lesion persisted and urgent surgical intervention was therefore indicated. By means of subcostal laparotomy, surgical drainage was performed twice, one week apart. However, there was no clinical or radiological improvement, and the etiology of the abscess was not determined. On the seventh postoperative day, the patient was discharged to ambulatory follow-up, remaining asymptomatic and afebrile. On the follow-up CT scan, the lesion was visualized again accompanied by a linear image of bone density measuring 3cm in connection with the gastric antrum and in intimate contact with the abscess (Fig. 1), which was not clearly visualized in the previous imaging tests.
A surgical intervention was scheduled for re-laparotomy and debridement of the inflammatory tissue encompassing the gastric antrum, hepatic flexure of the colon and liver segments V and VI, with a 4-cm fishbone that was perforating the lateral side of the lesser curvature of the stomach and piercing the liver. The fistula tract was resected and closed, the foreign body extracted and the abscessed liver area resected (Fig. 1b). The patient was discharged on the eighth day and has currently had no recurrence of the disease.
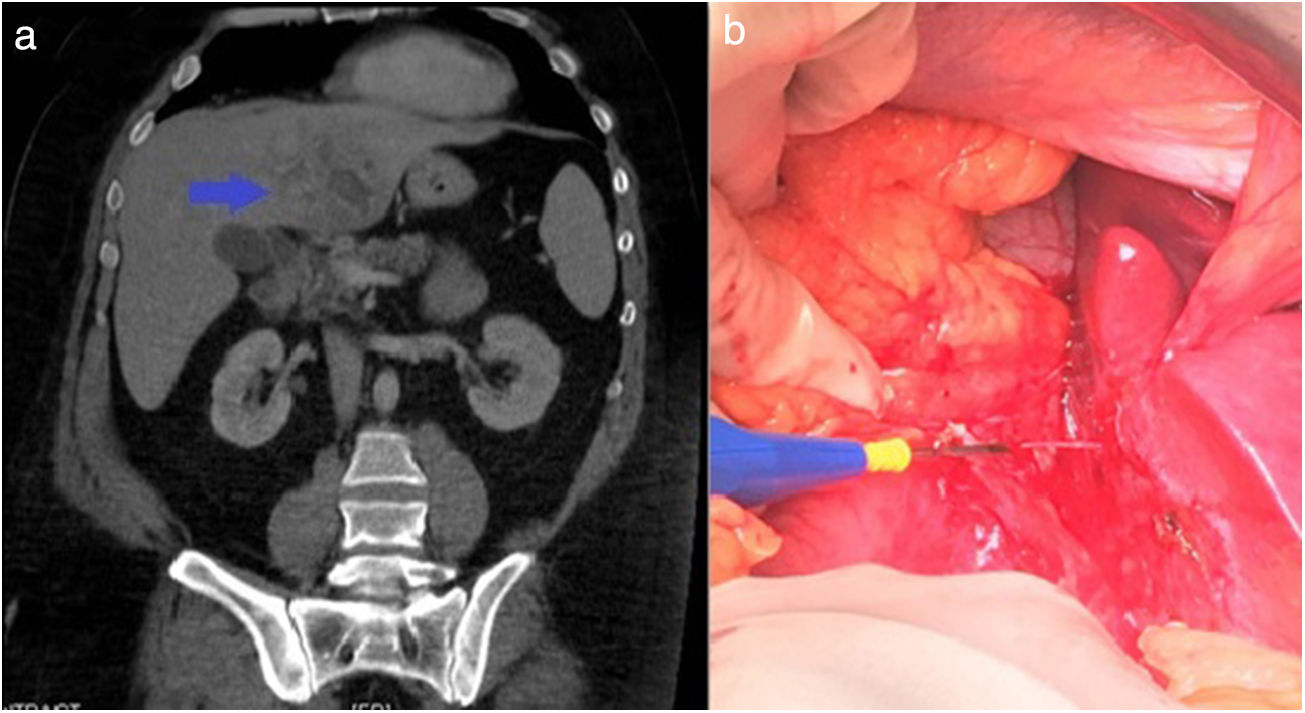
Case 2. A 44-year-old male with diffuse abdominal pain for one month, who consulted for worsening pain and leukocytosis (18500/mm3). CT scan revealed a linear foreign body with calcium density measuring 4cm in the left lobe of the liver, adjacent to an intraparenchymal collection measuring 5cm at its largest diameter, suggestive of liver abscess (Fig. 2); edema was also seen around the second part of the duodenum, with a possible area of perforation. Conservative treatment was initiated with empirical antibiotic therapy; the patient presented proper evolution and was discharged on the eighth day.
Elective surgery was subsequently conducted; after bilateral subcostal laparotomy, an inflammatory mass was found at the lesser curvature of the stomach. The abscess was drained, the gastric antrum perforation closed and the fishbone removed (Fig. 2b). The patient was discharged on the fifth day, with no complications or subsequent recurrence.
In general, accidentally-ingested foreign bodies pass through the gastrointestinal tract without complications in about one week.1,7 In certain cases (<1%), they cause intestinal perforation, migrate and reach the hepatic parenchyma, causing a liver abscess. The most frequent locations of perforation are the pylorus and the duodenum, and the migration zone is frequently the left hepatic lobe, due to proximity.2
These abscesses secondary to foreign bodies are usually related to sharp and pointed elements (toothpicks, chicken bones, needles or fishbones).3,5 Symptoms are non-specific (abdominal pain, fever, jaundice, weight loss and/or fatigue), and most patients do not remember having ingested the foreign body.1,8 Lab work usually shows elevated inflammatory parameters as well as increased liver enzyme levels. CT scan is the diagnostic test of choice due to its high resolution and diagnostic accuracy.6
Recent studies advocate initial conservative management with empirical antibiotic therapy, sometimes associated with percutaneous drainage, and subsequent removal of the foreign body either endoscopically or surgically.2,5 Endoscopic management may be indicated in cases diagnosed early and before perforation/migration of the foreign body has occurred.7 Despite this, surgery with removal of the foreign body, closure of the perforation, drainage and debridement of the abscess continues to be the treatment of choice to prevent recurrence.5,9
This etiology should be included in the differential diagnosis of a single, recurrent abscess, or with indirect evidence of adhesion or inflammation between the gastrointestinal tract and the liver observed on imaging tests, suggestive of the migration of a foreign body.2 Due to the imprecise diagnosis, multidisciplinary management is important, and surgery is the basic pillar for a definitive resolution.7,8
Please cite this article as: Jaén Torrejimeno I, Galeano Díaz F, López Guerra D, Blanco Fernández G. Absceso hepático por espina de pescado, un hallazgo inusual. Cir Esp. 2019;97:598–600.