The pancreatic fistula is the most feared complication after a duodenopancreatectomy, and is the most common independent factor of post-surgical mortality. Peng et al. recently published a pancreaticojejunal anastomosis technique (binding anastomosis) which showed 0% pancreatic fistulas. The objective of this study is to evaluate and validate this new anastomosis technique compared with the conventional pancreaticoduodenectomy with end-to-side duct-to-mucosa anastomosis.
Material and methodA prospective, non-randomised study was conducted to evaluate and validate this new anastomosis technique compared with the conventional pancreaticojejunal terminolateral duct to mucosa anastomosis. The study included 63 patients who were subjected to a duodenopancreatectomy due to having a pancreatic or periampullary neoplasm.
A binding pancreaticojejunostomy according to the technique described by Peng et al. was performed on 30 patients (Group A), and a pancreaticoduodenectomy with end-to-side duct-to-mucosa anastomosis (conventional technique) was performed on 33 patients (Group B).
ResultsWhen the results of the 2 techniques were compared, 2/30 (6%) of patients had a pancreatic fistula with the Peng technique, and 4/33 (12%) with the conventional technique, but this was not statistically significant (P=.674). Nor were there any significant differences between the 2 groups on comparing, morbidity, hospital stay and mortality.
ConclusionThe results of this study show that the anastomosis method described by Peng is safe, but is not associated with a lower frequency of pancreatic fistula, general morbidity, or mortality. This leads to the uncertainty of whether it really has any advantages over other techniques.
La fístula pancreática es la complicación más temida luego de una duodenopancreatectomía, siendo el factor independiente de mortalidad postoperatoria más frecuente. Recientemente Peng et al. publicaron una técnica de anastomosis pancreato yeyunal «anastomosis por atadura» (binding anastomosis) que presentaba 0% de fístula pancreática. El objetivo de este estudio es evaluar y validar esta nueva técnica de anastomosis comparada con la anastomosis pancreato yeyunal termino-lateral ducto mucosa convencional (PYTL-C).
Material y metodoSe efectuó un estudio prospectivo no aleatorizado para evaluar y validar esta nueva técnica de anastomosis comparada con la anastomosis pancreato yeyunal termino-lateral convencional. Se incluyó a 63 pacientes a quienes se les realizó una duodenopancreatectomía por presentar una neoplasia pancreática o periampular, intervenidos por un mismo cirujano.
A 30 pacientes (Grupo A) se les realizó una anastomosis termino-terminal según la técnica descrita por Peng, y a 33 pacientes (Grupo B) se les realizó una anastomosis termino-lateral mucosa-mucosa (técnica convencional).
ResultadosCuando se compararon las 2 técnicas, la fístula pancreática se presentó en 2/30 pacientes (6,6%) con anastomosis de Peng y en 4/33 pacientes (12%) con anastomosis mucosa-mucosa, sin embargo esto no fue significativo (p=0,674). Además cuando se comparó la morbilidad, estancia hospitalaria y mortalidad tampoco existió diferencia significativa entre los 2 grupos.
ConclusiónLos resultados de este estudio muestran que la anastomosis descrita por Peng es un método seguro, pero que no está asociada a una menor frecuencia de fístula pancreática, morbilidad general, ni mortalidad, por lo cual se puede poner en duda si realmente presenta una ventaja sobre otras técnicas.
Pancreaticoduodenectomy (PD) is a surgical procedure in which postoperative mortality has decreased over the last decade. Factors that explain this reduced mortality include the high level of specialization in large hospitals, experienced surgeons with important annual surgical volumes and new support therapies in intensive care units, as well as the correct selection of candidates for PD.1
However, post-operative morbidity continues to be high, ranging from 12% to 45% of cases in some series. Pancreatic fistula is the most feared postsurgical complication, which is present in a percentage of cases that varies from 5% to 30%.1,2
Pancreatic fistulas are the most important independent cause of death, and they also contribute to prolonged hospital stays and number of reoperations. Many factors have been associated with the appearance of pancreatic fistulas, including surgeon experience, volume of intraoperative bleeding, characteristics of the pancreas (hard vs soft), type of anastomosis used, the patient's previous nutritional state, etc.
The pancreatic anastomosis is one of the crucial points of the pancreaticoduodenectomy procedure and is still the Achilles heel of this surgery.
In order to reduce the incidence of pancreatic fistulas, different types of pancreatic anastomoses have been developed along with various alternative methods like the use of fibrin and octreotide, which have not improved the morbidity rates.3–7
Until approximately eleven years ago, there was no single type of anastomosis that provided greater benefits over the other frequently used techniques.4,5 However, since Peng published his technique with initial results in 2002 and then in 2007 when he presented the results of a prospective study with 0% pancreatic fistulas with a new anastomosis, we now question whether there really is a superior technique.7–10
The objective of this study is to compare one of the most frequently used techniques for pancreatic anastomosis with this new technique and to determine the effectiveness and safety reported in the literature
Materials and MethodsDuring a period of 3 years between January 2007 and February 2010, we carried out a non-randomized prospective study in order to evaluate the efficacy of 2 types of pancreatic anastomoses during PD in patients with a diagnosis of periampullary and pancreatic neoplasms.
In this period, 123 PD were carried out, 63 of which were done by the same surgeon and included in the protocol after a diagnosis of periampullary neoplasia. The patients were divided into 2 groups according to the type of anastomosis performed. In 30 patients, Whipple procedures were performed with Peng-type end-to-end pancreaticojejunal anastomoses, while in 33 cases termino-lateral mucosa-to-mucosa anastomoses were used (standard technique).
Excluded from the study were those patients who presented findings of unresectability during surgery, such as carcinomatosis, tumor infiltration of the mesenteric vessels, or portal and other metastases that were not detected in the preoperative tests. We also excluded patients who underwent pancreaticoduodenectomy for diagnoses other than periampullary neoplasia, those who had been operated on by another surgeon or those who required another type of pancreatic anastomosis.
The decision to perform one technique or the other was done sequentially, first starting with the patients undergoing mucosa-to-mucosa anastomosis and later performing the Peng anastomoses.
We evaluated age, sex, comorbidities, body mass index (BMI), operative time, bleeding and intraoperative transfusions, and consistency of the pancreas, reoperations, complications, start of oral intake, post-surgical hospital stay and mortality.
The Peng pancreatic anastomoses were performed in accordance with the original technique described by the author,7,9–11 while the mucosa-to-mucosa anastomoses were done in accordance with the standard technique described by several authors.12,13
We defined pancreatic fistula as drainage of more than 50 cc with an amylase level 3 times greater than normal serum levels after the tenth post-operative day.1,14,15
Operative mortality was defined as any death occurring during hospitalization after surgery or within the first 30 days post-surgery in patients who were discharged.
StatisticsTo compare the quantitative variables, the Student's t test was used; to compare the qualitative variables, either the chi-squared test or Fisher's exact test was used, depending on the case. The results are expressed by means and standard deviation. Differences were considered statistically significant when the result of a test produced a P<.05.
ResultsGeneral CharacteristicsOf the 63 patients included, 27 (43%) were men and 36 (57%) were women, with an average age of 67 (42–88 years), an average BMI of 25 (17–39) and an average tumor size of 3.5 (range 8–2cm).
The most frequent histologic diagnosis was adenocarcinoma of the ampulla of Vater in 32% of cases, followed by pancreatic ductal adenocarcinoma in 24%, pancreatic cystic tumors in 24%, cholangiocarcinoma in 9%, duodenal cancer in 6% and neuroendocrine tumors in 5%.
Overall morbidity was 36%, with a mortality of 1.5%.
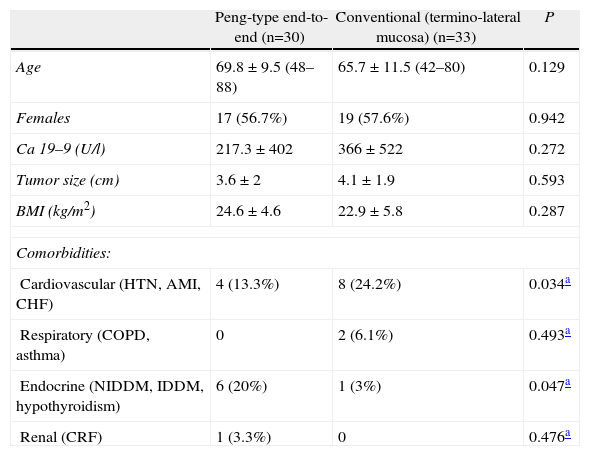
Evaluation by GroupsWhen we compared age, sex, preoperative diagnosis, history, Ca 19-9, tumor size and BMI, no significant differences were seen in the 2 study groups, and therefore both groups were considered comparable (Table 1).
Demographic Data.
| Peng-type end-to-end (n=30) | Conventional (termino-lateral mucosa) (n=33) | P | |
| Age | 69.8±9.5 (48–88) | 65.7±11.5 (42–80) | 0.129 |
| Females | 17 (56.7%) | 19 (57.6%) | 0.942 |
| Ca 19–9 (U/l) | 217.3±402 | 366±522 | 0.272 |
| Tumor size (cm) | 3.6±2 | 4.1±1.9 | 0.593 |
| BMI (kg/m2) | 24.6±4.6 | 22.9±5.8 | 0.287 |
| Comorbidities: | |||
| Cardiovascular (HTN, AMI, CHF) | 4 (13.3%) | 8 (24.2%) | 0.034a |
| Respiratory (COPD, asthma) | 0 | 2 (6.1%) | 0.493a |
| Endocrine (NIDDM, IDDM, hypothyroidism) | 6 (20%) | 1 (3%) | 0.047a |
| Renal (CRF) | 1 (3.3%) | 0 | 0.476a |
IDDM: insulin-dependent diabetes mellitus; NIDDM: non-insulin-dependent diabetes mellitus; COPD: chronic obstructive pulmonary disease; HTN: arterial hypertension; CHF: congestive heart failure; AMI: acute myocardial infarction; CRF: chronic renal failure.
Level of significance P<.05.
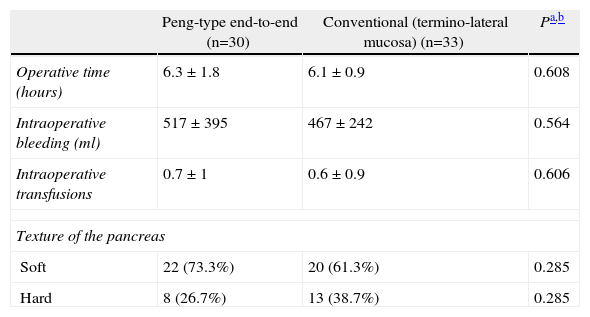
As for the intraoperative variables such as operative time, bleeding and transfusions, as well as the pancreas texture, we found no significant differences in the 2 groups (Table 2).
Intraoperative Data.
| Peng-type end-to-end (n=30) | Conventional (termino-lateral mucosa) (n=33) | Pa,b | |
| Operative time (hours) | 6.3±1.8 | 6.1±0.9 | 0.608 |
| Intraoperative bleeding (ml) | 517±395 | 467±242 | 0.564 |
| Intraoperative transfusions | 0.7±1 | 0.6±0.9 | 0.606 |
| Texture of the pancreas | |||
| Soft | 22 (73.3%) | 20 (61.3%) | 0.285 |
| Hard | 8 (26.7%) | 13 (38.7%) | 0.285 |
Level of significance for values P<.05.
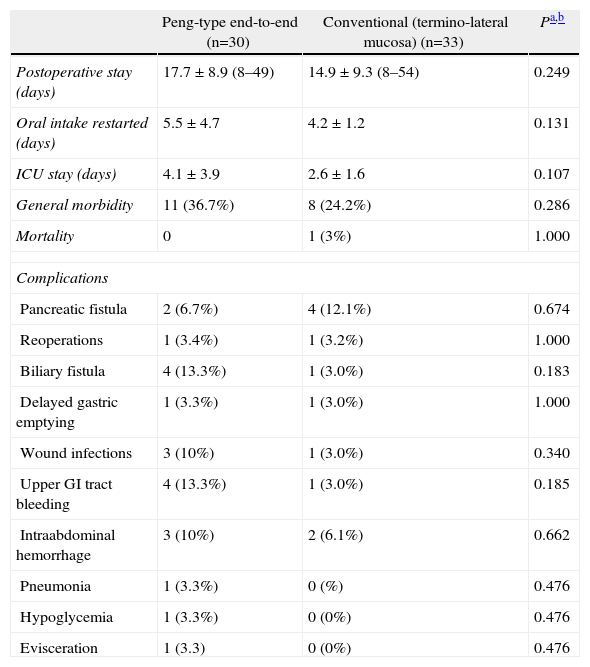
When results were compared for general morbidity, we observed that the group of patients with Peng anastomosis had more morbidity than the group with mucosa-to-mucosa anastomosis; however, this difference was not statistically significant. When we evaluated the frequency of intra-abdominal hemorrhage, this was present in the Peng group in 10% of the cases, while in the mucosa-to-mucosa group it occurred in 3%. Likewise, digestive hemorrhage was more frequent in the group with Peng anastomosis (3% vs 16%). However, when we compared the different complications individually, we could observe that there was no significant difference in the 2 series (Table 3).
Postoperative Data and Complications.
| Peng-type end-to-end (n=30) | Conventional (termino-lateral mucosa) (n=33) | Pa,b | |
| Postoperative stay (days) | 17.7±8.9 (8–49) | 14.9±9.3 (8–54) | 0.249 |
| Oral intake restarted (days) | 5.5±4.7 | 4.2±1.2 | 0.131 |
| ICU stay (days) | 4.1±3.9 | 2.6±1.6 | 0.107 |
| General morbidity | 11 (36.7%) | 8 (24.2%) | 0.286 |
| Mortality | 0 | 1 (3%) | 1.000 |
| Complications | |||
| Pancreatic fistula | 2 (6.7%) | 4 (12.1%) | 0.674 |
| Reoperations | 1 (3.4%) | 1 (3.2%) | 1.000 |
| Biliary fistula | 4 (13.3%) | 1 (3.0%) | 0.183 |
| Delayed gastric emptying | 1 (3.3%) | 1 (3.0%) | 1.000 |
| Wound infections | 3 (10%) | 1 (3.0%) | 0.340 |
| Upper GI tract bleeding | 4 (13.3%) | 1 (3.0%) | 0.185 |
| Intraabdominal hemorrhage | 3 (10%) | 2 (6.1%) | 0.662 |
| Pneumonia | 1 (3.3%) | 0 (%) | 0.476 |
| Hypoglycemia | 1 (3.3%) | 0 (0%) | 0.476 |
| Evisceration | 1 (3.3) | 0 (0%) | 0.476 |
Level of significance for values P<.05.
Pancreatic fistulas presented in 9.5% of cases in the entire series. When the two techniques were compared, fistulas occurred in 7% of patients with Peng anastomosis and in 12% of patients with mucosa-to-mucosa anastomosis, although the difference was not significant (P=.67).
When we compared the incidence of pancreatic fistulas according to the consistency of the pancreas, we were able to observe that in the hard pancreas there were no cases of fistula in the group with Peng anastomosis, while in the mucosa-to-mucosa group there were fistulas in 4.5%. As for the soft pancreas, fistulas occurred in 9% of the Peng group and rose to 25% in the mucosa-to-mucosa group; there were, however, no significant differences in the 2 groups (P>.05) (Table 3).
As for the post-operative course, data are shown in Table 3. There were no significant differences in morbidity of the group with Peng anastomosis (11/30) and the mucosa-to-mucosa technique group (8/33), with a P=.29; the same was found when we compared hospital stay, reinstitution of oral intake, reoperations, intensive care stay or mortality.
DiscussionThe frequency of pancreatic fistulas depends on many factors, such as anatomy, characteristics of the gland and skill of the surgeon in performing pancreatic anastomosis; thus, the most important step to avoid pancreatic fistulas is prevention.16–18 In addition, it is very important to be able to distinguish the characteristics of the pancreas, such as consistency and the size of the Wirsung duct because these are factors of vital importance for predicting which patients have a greater probability of presenting pancreatic fistulas.19,20
It is essential to have a refined technique and to choose a safe pancreatic anastomosis. The problem lies in that fact that there are many types of techniques for creating pancreatic anastomoses, and until now no technique has been described as “superior”.
From 2002 until 2004, Peng published a series of cases describing a new pancreatic anastomosis with truly surprising results. In these series, there is no single report of any pancreatic fistulas in more than 100 operated patients; there is, however, a reported morbidity of 35%.10,11
Published in 2007, Peng's last study concludes that this technique drastically reduces the risk of pancreatic fistula, complications and hospital stay.
According to the author, this new pancreatic anastomosis presents a tremendous advantage over other techniques described since there are no reported pancreatic fistulas, and this is one of the most feared complications after pancreaticoduodenectomy.
For this reason, several studies have been performed to evaluate the pancreatic anastomosis described by Peng in order to validate the results and to know whether we actually have a technique that is superior to others.
In a study published by Buc in 45 patients who underwent Peng anastomosis on a soft pancreas, the results presented by Peng were not reproduced and 8.9% of the patients presented a pancreatic fistula.
Furthermore, Maggiori concluded that this technique is not associated with a lower incidence of post-surgical pancreatic fistulas but is instead associated with a greater incidence of post-pancreatectomy hemorrhages.14,21
When the two techniques were compared in our study, there were no differences in the frequency of pancreatic fistula, nor were there differences in morbidity or mortality. Thus, once again, the results obtained by Peng could not be replicated.
In addition, it is important to highlight that in the series of cases by Peng, although there is not one single case of pancreatic fistula, neither morbidity nor mortality are any lower than when the conventional technique is done.13
In our study, we have found the same association as Maggiori regarding the presentation of post-pancreatectomy intraabdominal hemorrhage; this complication in the Peng anastomosis group was 3% vs 10% in the mucosa-to-mucosa group; the difference was that in our series this was not significant.
Furthermore, when hospital stay was compared between the 2 groups, there was no significant difference between the 2 techniques, showing no advantage when the Peng technique was used.
We should point out that in this study all the patients were operated on by the same surgeon, who performs a high volume of pancreaticoduodenectomies annually. This could positively influence our results in general, but, at the same time, it tests the feasibility of reproducing Peng's technique, without having shown any benefit over a classical pancreatic anastomosis technique.
The problem presented is that none of these 3 studies could reproduce the results obtained by Peng because there were incidences of pancreatic fistulas in all the studies.
ConclusionPeng's anastomosis technique is a safe and reliable method for performing pancreatic anastomosis after pancreaticoduodenectomy. Nonetheless, it is not associated with a lower frequency of pancreatic fistula complications, hospital stay or mortality than the standard technique.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Targarona J, et al. ¿Es la anastomosis pancreato yeyunal de Peng más efectiva que la anastomosis muco-mucosa en la duodenopancreatectomía por neoplasias de páncreas y periampulares? Cir Esp. 2013;91:163–8.