Infected aneurysms are associated with a high mortality rate (approximately 44%)1 and require early surgical treatment due to their rapid growth and possibility of systemic sepsis.2
Staphylococcus, Streptococcus or Salmonella are classically involved, although there are more and more reports of cases with atypical microorganisms, like Campylobacter fetus1 (C. fetus). Potentially susceptible patients are those with underlying diseases, such as diabetes, cardiovascular disease or some type of immunodeficiency.3 The first case was reported in 1971 by Dolev, and the first successful repair was done in 1983 by Marty.1
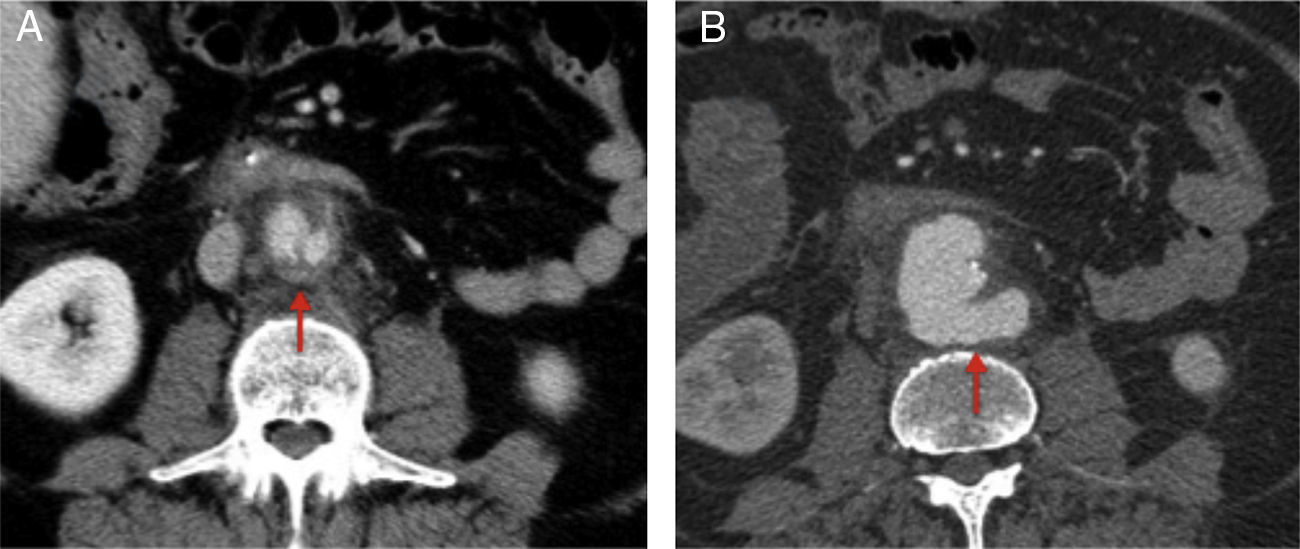
We present the case of a 62-year-old male with a history of arterial hypertension, diabetes mellitus, ischemic cardiopathy, hepatic steatosis, splenectomy for Hodgkin's lymphoma and transurethral resection due to bladder cancer. He came to the Emergency Department with pain in the mesogastrium, accompanied by liquid stools during the previous 3 days, but no fever or systemic involvement. Lab work-up was nonspecific, and the patient was diagnosed with viral gastroenteritis. Seven days later, he once again came to the ER with intense abdominal pain. Abdominal-pelvic CT scan revealed a saccular infrarenal aortic aneurysm measuring 3.5cm adjacent to the third portion of the duodenum, as well as a diffuse increase in periaortic retroperitoneal fat density compatible with mycotic aneurysm, actinic aortitis or aortic ulcer (Fig. 1). The patient continued to be stable and had no fever; abdominal examination was normal, with no guarding or signs of peritonitis. Lab work-up showed slight leukocytosis (11.8×109/l) and elevated transaminases (FA: 771IU/L; GGT: 815IU/L; GOT: 50IU/L; GPT: 56IU/L).
The patient was admitted to the vascular surgery ward for observation and further studies. Due to the hepatic pattern, abdominal ultrasound, upper gastrointestinal endoscopy and colonoscopy were done but provided no significant findings. On the 5th day, the patient had an abrupt episode of abdominal pain radiating to the left lumbar region, with no hemodynamic instability. Emergency abdominal CT scan showed rapid growth (1.7cm) of the aneurysm (largest diameter: 5.2cm) versus contained rupture (Fig. 1).
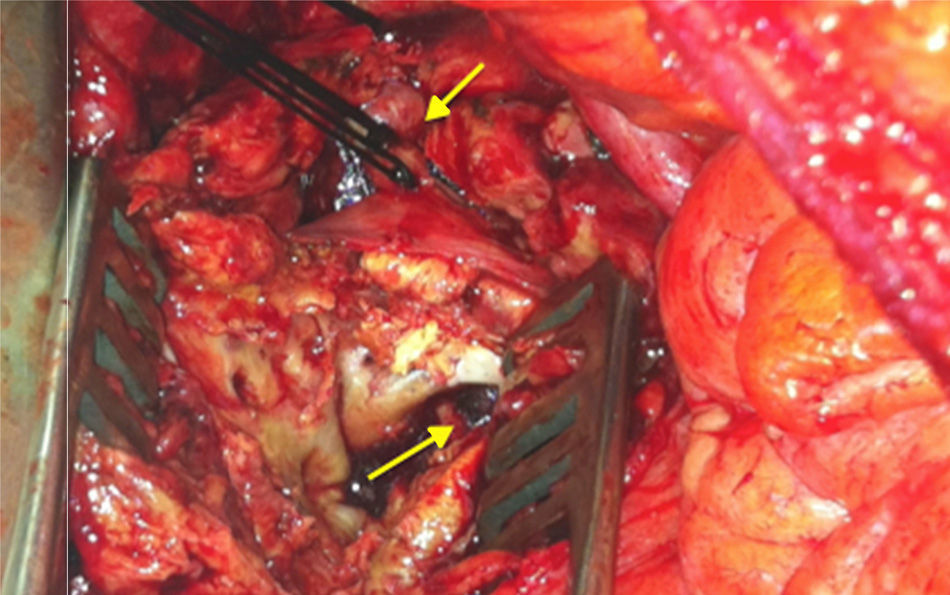
Midline laparotomy was performed urgently with a transperitoneal approach and infrarenal clamping. A saccular infrarenal aortic aneurysm was observed with a large amount of fibrosis that made dissection difficult, along with a contained rupture at the posterior side and visualization of the prevertebral ligaments (Fig. 2). It was not possible to perform a bypass in situ, so we ligated the aortic stump, resected the aneurysm and collected samples. The lower extremities were revascularized by right axillofemoral bypass (Dacron silver 8×8mm), and the patient left the operating room in stable condition with positive peripheral pulses. Cultures were positive for C. fetus, and treatment was initiated with imipenem and ciprofloxacin.
On the 10th day, the patient presented melenas and hematemesis due to an ulcer in the second part of the duodenum, which was resolved with hemostatic clips. Beforehand, abdominal CT scan had ruled out aortoenteric fistula. Four days later, the patient's general condition worsened, and bilious secretions were observed through the abdominal drain orifice. With the suspicion of choleperitoneum, an exploratory laparotomy was done, although the bile duct could not be accessed due to dense adhesions. Treatment with somatostatin was begun, and the patients’ progress was favorable. He was discharged 54 days after the aortic surgery, during which time he had completed 6 weeks of specific antibiotic therapy.
The incidence of infected aneurysms is below 3%; around 50% are abdominal aortic aneurysms.4 Their management is complex because of the greater morbidity and mortality as a result of the high risk for rupture (50%–85%).1,2C. fetus may be one of the most frequent atypical microorganisms observed in these cases due to the higher sensitivity of current diagnostic tests5 and because it is a Gram-negative bacillus that is microaerophilic and has a predilection for the vascular endothelium.3 It is associated with severe systemic diseases, such as meningitis, endocarditis, pneumonia or, in some cases, mycotic aneurysms.6 Unlike C. jejuni, the presentation of diarrhea is uncommon.3 Our case started with colicky abdominal pain and 3 days of diarrhea.
The diagnosis of infected aneurysm is a challenge as the classic triad of fever, pain and a pulsating mass is seen in less than 50% of cases and in only 29% of case reports with C. fetus.1 Our patient had no fever, no mass was palpated and leukocytosis was nonspecific.
The diagnostic test of choice is abdominal-pelvic CT scan. It may not be conclusive in some cases, and the possibility of other diseases should be considered.7 Most mycotic aneurysms are saccular and have poly-lobulated edges.8 An important finding is the increased density in periaortic fat (representing the retroperitoneal inflammatory response).1 Other less frequent findings include: edema or periaortic gas, multiple aneurysms or vertebral abnormalities.7,8 There are no characteristic tomographic signs for C. fetus infection; nevertheless, the majority of the cases reported show evidence of a retroperitoneal fibrous reaction.6 CT angiography at admission of our patient showed increased periaortic fat density, and the second demonstrated an important retroperitoneal fibrotic reaction.
The surgical approach is controversial. The classical option of extracorporeal membrane oxygenation with aortic ligation is not free of complications, such as rupture of the stump or long-term low permeability of the bypass. Aneurysmatic resection and reconstruction using in situ bypass is the preferred procedure for stable patients with localized infection and low risk for systemic infection, accompanied by extensive debridement and prolonged antibiotic therapy.9 Chun-Hui described similar long-term survival rates between extracorporeal repair and in situ bypass, although with greater postoperative complications.2 Currently, endovascular treatment is attractive as a “bridge” procedure in unstable patients, given the elevated morbidity and mortality of open surgery.4 Regardless of the technique, wide-spectrum antibiotic therapy is a constant and should be initiated empirically for a minimum of 4–6 weeks. In the case of C. fetus, imipenem is the antibiotic of choice.2,3
In conclusion, aneurysms infected by C. fetus are uncommon. They should be suspected in immunocompromised patients in whom surgery should not be delayed due to their rapid growth and high rate of rupture.
Please cite this article as: Peralta Moscoso MT, García López M, Vilariño Rico J. Aneurisma micótico de aorta abdominal por Campylobacter fetus. Cir Esp. 2015;93:413–415.