Paragangliomas or extra-adrenal pheochromocytomas are rare tumors derived from chromaffin cells. The organ of Zuckerkandl is the most frequent location. It is a group of paraganglia found below the diaphragm in the interaortocaval space, above the aortic bifurcation. Although patients present characteristic symptoms, such as difficult-to-manage secondary arterial hypertension, headache and palpitations, these symptoms are not very specific and may go unnoticed. The clinical diagnosis is usually made by exclusion, and this pathology should be considered in the differential diagnosis of abdominal pain. Malignancy is rare and defined by the presence of metastasis.1,2
The following is a case report of a patient with a paraganglioma of the organ of Zuckerkandl, accompanied by a review of the literature.
We present a 30-year-old male patient with a history of thoracic outlet syndrome, generic urticaria and appendectomy. During the study of non-specific abdominal pain that had been progressing for several years, an ultrasound study revealed a 4cm nodule compatible with interaortocaval lymphadenopathy. This tumor did not diminish in subsequent follow-up tests, so CT angiography (Fig. 1) and magnetic resonance angiography were ordered, which demonstrated inflammatory lymphadenopathy and could not rule out a neurogenic tumor. Ultrasound-guided FNA of the retroperitoneal mass provided a positive result for paraganglioma.
The tumor was assessed for possible functionality, observing the presence of arterial hypertension and elevated catecholamine levels: noradrenalin: 545mcg/24h (normal N<76mcg); adrenaline 5mcg/24h (N<18mcg); dopamine 910mcg/24h (N<390mcg) and vanillylmandelic acid 11.3mcg/24h (N<10mcg) in urine. Metaiodobenzylguanidine scintigraphy revealed a lesion with moderate uptake intensity in the posterior planes of the right paraumbilical abdominal region. Distant lesions were ruled out.
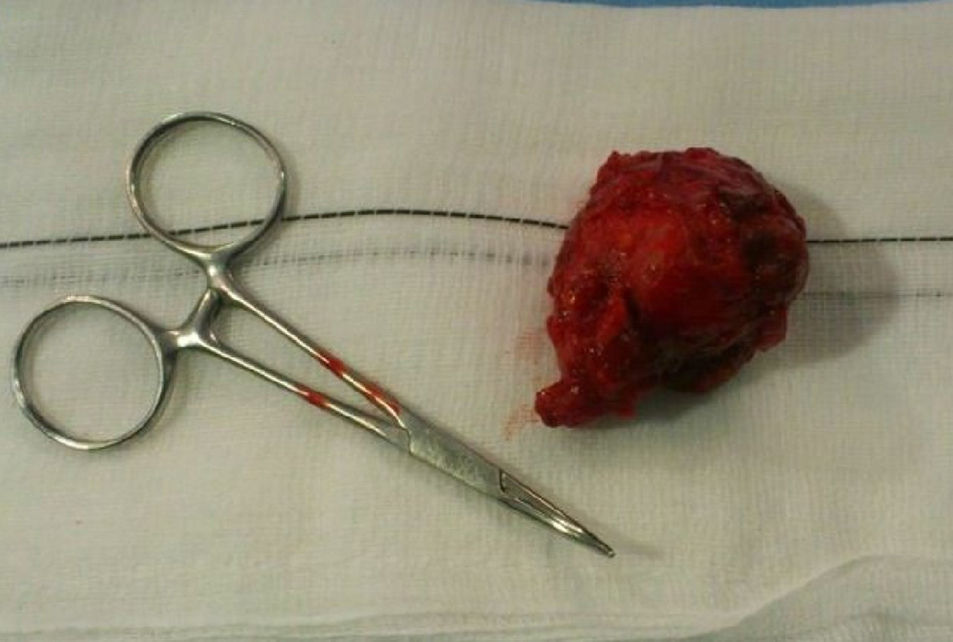
Once the arterial hypertension was under control with labetalol, the tumor was resected by means of a right anterior retroperitoneal surgical approach after dissection and control of the large blood vessels (Fig. 2). The pathology study confirmed the diagnosis of paraganglioma of the organ of Zuckerkandl. The postoperative period was uneventful, with no abdominal or local complications of infection. The patient was discharged after 7 days for later outpatient follow-up. The first ultrasound study was done 6 months later, followed by annual studies thereafter. The patient is currently asymptomatic.
Paragangliomas are an uncommon clinical problem with an incidence of 0.2–0.5 cases/100000 inhabitants/year.3 The incidence is similar between men and women, although some authors report a greater prevalence among men.4 Mean age at presentation is 42, and cases can be sporadic (10%) or familial (between 25 and 50%). Presentation can also be solitary or multiple. Their behavior differs according to cytological characteristics and the location of the tumor.5
Based on their topography, paragangliomas are classified as adrenal (pheochromocytomas) and extra-adrenal (supradiaphragmatic, branchiomeric and intravagal, aortosympathetic and autonomous-visceral). The location of 90% is adrenal, while 10% are extra-adrenal.4,6 The possibility to produce catecholamines is significant in extra-adrenal retroperitoneal locations.7 In the abdomen, the most frequent extra-adrenal location is the organ of Zuckerkandl.5,6 77% are functioning and cause hypertension, headache and palpitations.7–9 In 23% of non-functioning paragangliomas, the symptoms at presentation usually include abdominal pain (32%) or palpable mass (32%). It is important to establish the differential diagnosis with other abdominal masses, especially malignant tumors.
The treatment of choice for tumors in any location, without distant metastasis, as in our patient, is complete tumor resection using either laparoscopy or conventional surgery. The choice of treatment should be guided by proper patient selection and the experience of the surgical team. Some authors consider laparoscopy the method of choice due to its lower morbidity and mortality, relegating conventional surgery for large tumors or those adhered to neighboring structures.5 It is important to properly control perioperative arterial tension using combined β- and α-adrenergic blockers.
Surgery is associated with improved survival.3,8,10 Local radiotherapy is the alternative for non-resectable tumors, either for their size or location, and the use of coadjuvant chemotherapy is anecdotal.1
There are no established criteria to define malignancy of a paraganglioma. Nonetheless, it is believed that the invasion of adjacent tissues, capsular invasion, elevated mitotic rate, mass size larger than 5cm, weight over 80g and the recurrence or presence of distant metastatic disease indicate malignancy.5 Tumors that originate in the head and neck are generally non-functioning and have a very low probability for distant metastasis. Those that originate in the retroperitoneum can present metastasis at the time of diagnosis in approximately 10% of patients and reach 40% over the course of the natural progression of the pathology; the lungs, lymph nodes, bones and spleen are the most frequently affected organs. The possibility for producing catecholamines is significant in extra-adrenal retroperitoneal locations.2,6
Because recurrences or distant metastases can appear years after the initial diagnosis, long-term follow-up in patients with paragangliomas is fundamental.
Authorship/CollaboratorsElisa María Evangelista Sánchez: composition of the article and approval of the final version.
Esther Doiz Artázcoz: composition of the article, critical review and approval of the final version.
Manuel Rodríguez Piñero: study design and data collection.
Antonella Craven-Bartle Coll: data collection and analysis of the results.
Rosario Conejero Gómez: analysis of the results and critical review.
Conflict of InterestsNone of the authors have conflicts of interests.
Please cite this article as: Evangelista Sánchez EM, Doiz Artázcoz E, Rodríguez Piñero M, Craven-Bartle Coll A, Conejero Gómez R. Paraganglioma del órgano de Zuckerkandl. Cir Esp. 2016;94:483–484.