Laparoscopic appendectomy is probably the technique of choice in acute appendicitis. Single port laparoscopic surgery (SILS) has been proposed as an alternative technique. The objective of this study is to compare the safety and efficacy of SILS against conventional laparoscopic appendectomy (LA).
Material and methodsFrom January 2011 to September 2012, 120 patients with acute appendicitis were prospectively randomized; 60 for SILS and 60 for LA. Patients between 15 and 65 years were selected, with onset of symptoms less than 48h. We compared BMI, surgery time, start of oral intake, hospital stay, postoperative pain, pathology, and costs.
ResultsThe median age, BMI, sex, and time of onset of symptoms to diagnosis were similar. There were no statistically significant differences in the operative time, start of oral intake, or hospital stay. There was a significant difference in postoperative pain being higher in SILS (4±1.3) than in LA (3.3±0.5) with a P=.004. Flemonous appendicitis predominated in both groups in a similar percentage. A total of 3 cases with intra-abdominal abscess (SILS 2, LA 1) required readmission and resolved spontaneously with intravenous antibiotic treatment. One case of SILS required assistance by a 5mm trocar in the RLC for drainage placement. The cost was higher in SILS due the single port device.
ConclusionSILS appendectomy is safe, effective, and has similar results to LA in selected patients, and although the cost is greater, the long term results will determine the future of this technique.
La apendicectomía laparoscópica es probablemente en la actualidad la técnica de elección en las apendicitis agudas. La cirugía laparoscópica por puerto único (PU) ha intentado instalarse como técnica alternativa. El objetivo de este estudio es comparar la seguridad y eficacia del PU frente a la apendicectomía laparoscópica convencional (LC).
Material y métodosDe enero del 2011 a septiembre del 2012 se aleatorizó prospectivamente a 120 pacientes con apendicitis aguda (PU 60, LC 60). Se seleccionó a pacientes entre 15 y 65 años con inicio de síntomas<48h comparándose el IMC, tiempo operatorio, inicio de ingesta, estancia hospitalaria, dolor postoperatorio, anatomía patológica y costes.
ResultadosLa edad media, IMC, sexo y tiempo de inicio de síntomas hasta el diagnóstico fueron similares. No se encontraron diferencias del tiempo operatorio, inicio de ingesta ni estancia hospitalaria. Se evidenciaron diferencias en el dolor postoperatorio siendo mayor en el PU (4±1,3) que en la LC (3,3±0,5) con una p=0,004. La apendicitis flemonosa predominó para ambos grupos. Hubo 3 reingresos por absceso intraabdominal (PU 2, LC 1) que requirieron tratamiento antibiótico intravenoso. Un caso del PU requirió asistencia intraoperatoria de un trocar de 5mm en FID por necesidad de drenaje. El coste fue mayor en el PU debido al dispositivo empleado.
ConclusiónLa apendicectomía por PU es segura, eficaz con resultados similares a la LC en pacientes seleccionados y, aunque el coste es mayor, serán los resultados obtenidos a largo plazo los que determinen el futuro de esta técnica.
Laparoscopic appendectomy is probably the current technique of choice for acute complicated or uncomplicated appendicitis. Since Semm performed the first laparoscopic appendectomy in 1983, a large variety of papers have been published, noting the advantages of this technique compared to open appendectomy.1–3 However, in an effort to “minimize” the incision in the abdominal wall, laparoscopic surgery through a single port is now being used, commonly known as SILS (Single-Incision Laparoscopic Surgery). This relatively new concept started over 15 years ago in pediatric surgery,4–8 evolving to the present day with the development of devices and medical graspers that have helped the surgeon to extend its application to other diseases.9 SILS-based appendectomy tries to position itself as an alternative technique compared to conventional laparoscopy (CL), with emphasis on the publication of studies with better cosmetic results,10,11 considering that it is usually performed through the umbilicus and the scar is almost invisible.
This is a prospective randomized study comparing CL-based appendectomies to SILS-based appendectomies. Parameters are analyzed such as surgery time, start of oral intake, hospital stay, post-surgery pain, post-surgery complications, pathology, and costs.
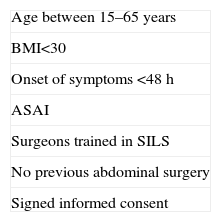
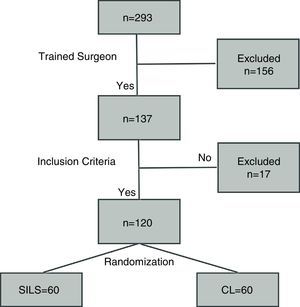
Materials and methodsIn January 2011, a prospective randomized study was initiated, aiming to compare SILS to CL. The study included 60 patients for each technique, with the following inclusion criteria: patients aged between 15 and 65 years, with BMI<30, onset of symptoms less than 48h, absence of previous abdominal surgery, ASA anesthesia risk I, presence of a surgeon trained in both techniques and signed informed consent (Table 1). The age range of patients was based on that of the economically active population, given that it is a well-defined population sector and relevant to the statistical study. Another factor for inclusion was non-obese patients, i.e. with a BMI<30, because a higher value would increase the possibility of complications.12,13 Appendicitis cases with a time of onset of symptoms of less than 48h were selected, predictably uncomplicated (no perforation, no diffuse or localized peritonitis). Pain was assessed with a visual analog scale (VAS) on discharge. Another important factor to note was the motivation of the surgeon to perform this type of technique; therefore, 3 surgeons were considered who were interested in learning and developing it. These surgeons had no previous experience with SILS-based appendectomies, but did with CL, which made it easier on their learning curve.14 All the patients included were informed and accepted the randomized study; none of them had previous abdominal surgery. Informed consent was signed by all patients who accepted both techniques.
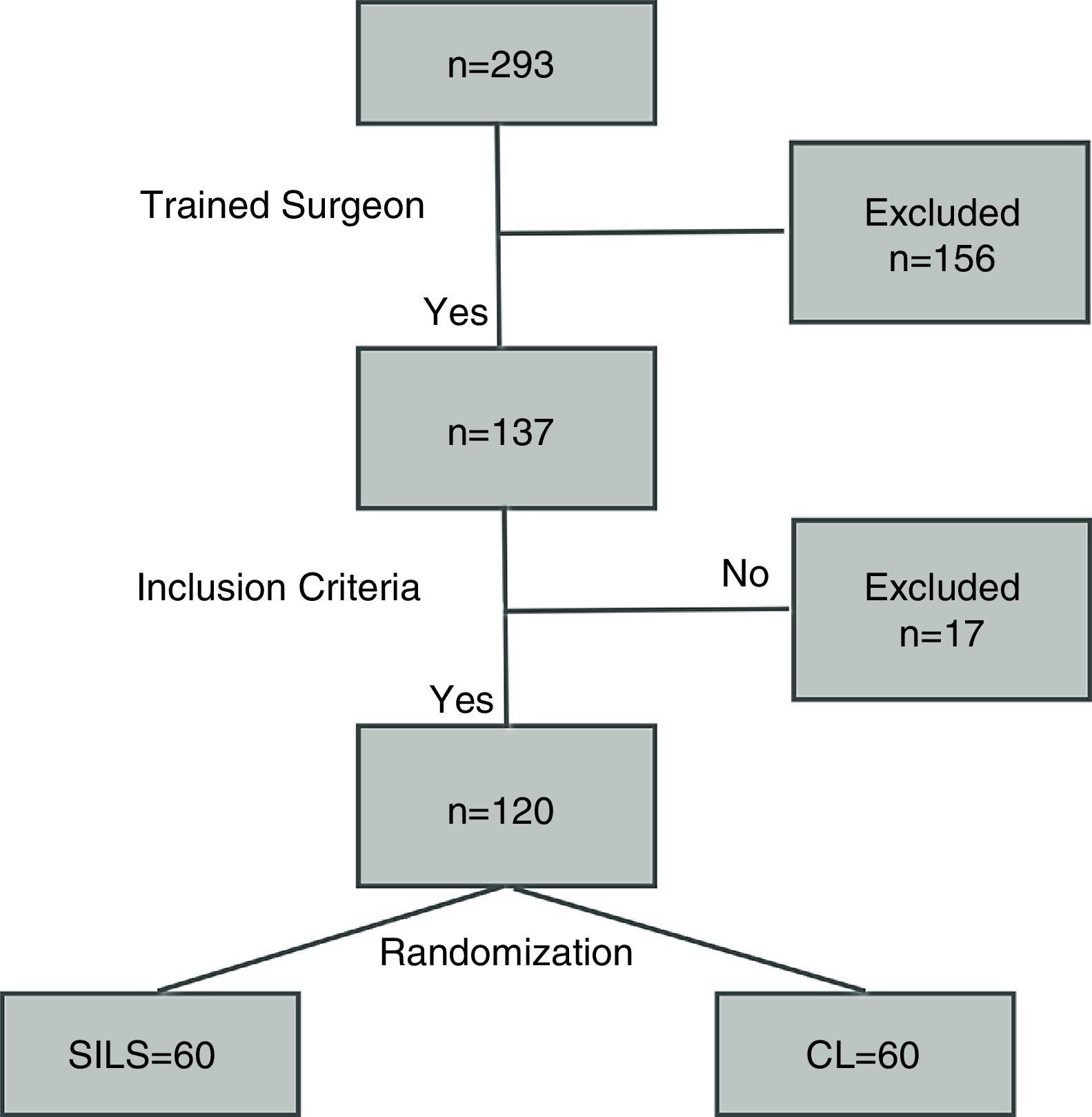
A performance algorithm was developed as shown in Fig. 1. Randomization was performed by closed envelope in a box where 60 envelopes were placed for each technique.
The CL material used was a Hasson trocar, one of 11mm, and another one of 5mm. 30° 10mm optics, graspers (2), scissors, hook, endoloops (2), endoclip. For SILS, the single port device (Covidien SILS port) was used®, 5mm and 30° optics, articulated grasper (Covidien Roticulator Endo Grasp®), scissors, endoloops (2), endoclip and in some cases, for the two techniques, Covidien Ligasure® and endostapler (Covidien Endo-GIA®).
Conventional laparoscopic appendectomy was performed with a 1cm approximately periumbilical incision to place the Hasson and where the optics were inserted, another 5mm incision in FII and 11mm approx. in the suprapubic region. All appendices were bagged and removed through the umbilical incision under direct vision with 11mm trocar-inserted optics. The aponeuroses of the umbilical and suprapubic incisions were closed with 0 long-duration absorbable suture (Ethicon PDS®) and staples for skin.
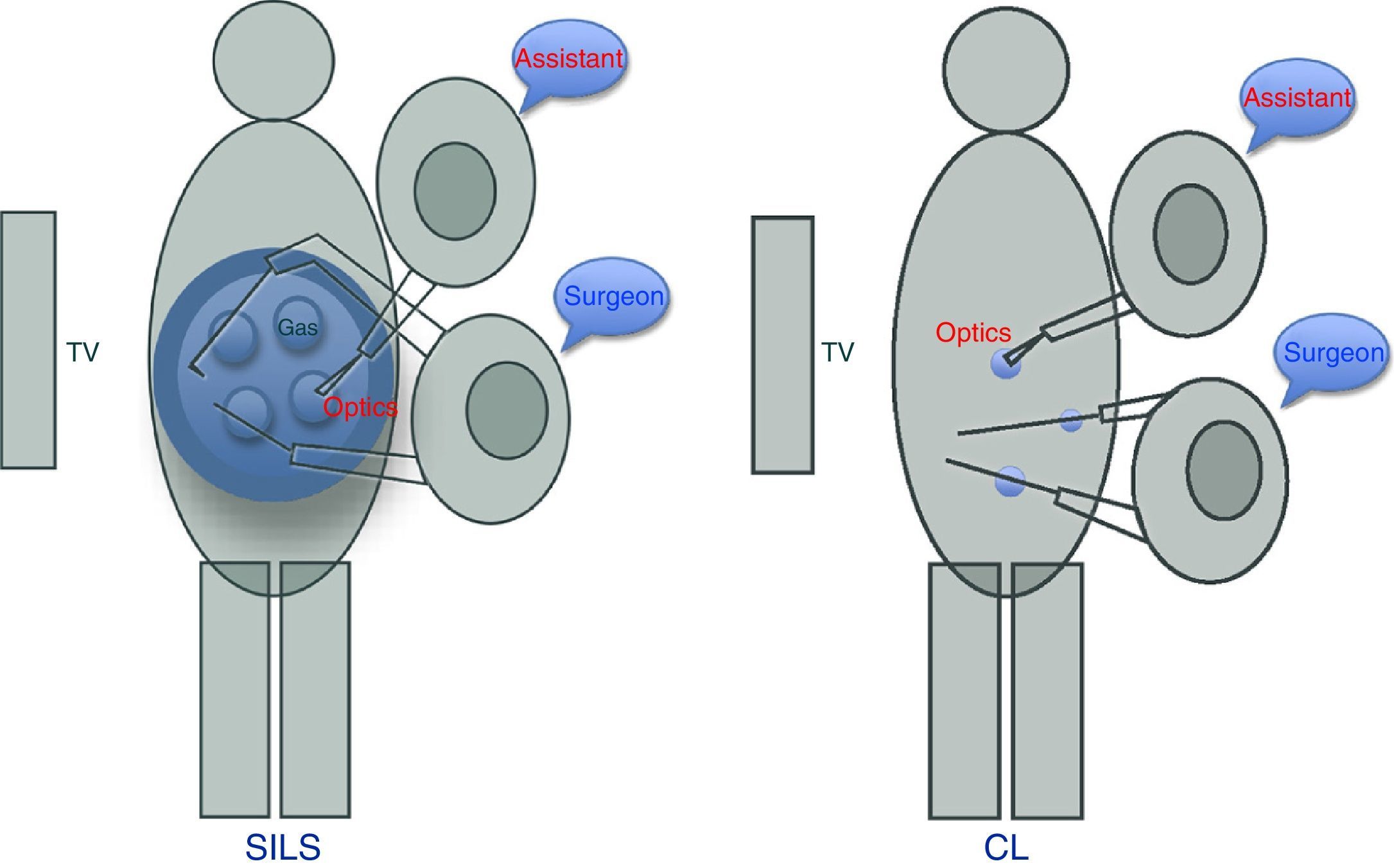
SILS-based appendectomy was performed via an approximately 2.5–3cm transumbilical incision where the SILS port was inserted®. This device has 4 orifices, one for inserting the gas, another for optics, and the other 2 for surgeon's manipulations. It is important to place the optics in the orifice closest to the surgeon, allowing better vision and to avoid interfering with the assistant (Fig. 2). In 39 cases (No.=60), there was no need to use the articulated grasper. To bag the appendix, a collection bag was used, after the placing the 12mm trocar in the orifice most distal to the surgeon. The aponeurosis was closed with 0 long-duration absorbable suture (Ethicon PDS®), with interrupted sutures, followed by one 3–0 fast-absorbing intradermal suture (Ethicon Vicryl Rapid®).
Neither of the techniques used anesthetic infiltration to avoid errors in measuring post-surgery pain. Surgeries were performed with the patient in slight Trendelenburg, inclined to the left, which facilitated the procedure. For our hospital protocol (for easier Douglas viewing, and to avoid bladder injury) only patients undergoing CL-based appendectomy received a urinary catheter, which was removed at the end of the surgery.
The results were entered into a database and analyzed using the SPSS application®. For quantitative variables, the Student t test was used, and the chi square test for non-quantitative variables. P<.05 was accepted as the level of statistical significance.
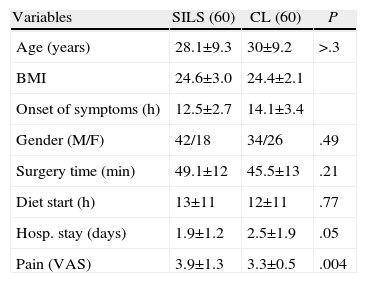
ResultsBetween January 2011 and September 2012, surgery was conducted on 293 acute appendicitis patients overall, of which 120 met the study inclusion criteria (Table 2). No significant differences were observed for all these parameters between the two groups. In addition, surgery time was similar for the two groups, as well as the start of fluid intake and hospital stay. Post-surgery pain was measured using the VAS scale (0–10), with higher readings for SILS with a statistically significant difference (P=.004; SILS 4±1.3; CL 3.3±0.5). The pathological study revealed the following groups: unaltered appendix, acute catarrhal, phlegmonous or suppurative, and gangrenous appendicitis. The findings were similar for each group, predominantly for phlegmonous appendicitis; SILS (73%) and CL (77%) did not show significant differences (P=.21).
Variables According to Surgery Technique.
| Variables | SILS (60) | CL (60) | P |
| Age (years) | 28.1±9.3 | 30±9.2 | >.3 |
| BMI | 24.6±3.0 | 24.4±2.1 | |
| Onset of symptoms (h) | 12.5±2.7 | 14.1±3.4 | |
| Gender (M/F) | 42/18 | 34/26 | .49 |
| Surgery time (min) | 49.1±12 | 45.5±13 | .21 |
| Diet start (h) | 13±11 | 12±11 | .77 |
| Hosp. stay (days) | 1.9±1.2 | 2.5±1.9 | .05 |
| Pain (VAS) | 3.9±1.3 | 3.3±0.5 | .004 |
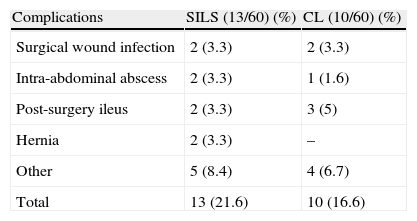
There were 13 post-surgery complications with SILS (22%), and 12 with CL (20%), with a P=.78. Notably, for SILS, there were 2 intra-abdominal abscess cases requiring hospitalization for IV antibiotics, and only one case for CL. In the two groups, the collections were located in the right iliac fossa, without the need for additional surgery or puncture-drainage, due to good response to antibiotic treatment. Intrasurgery lavage data were collected as well (SILS 16 and CL 19; P=.49), anticipating that its excess could be a condition for having an intra-abdominal abscess.15 Other complications such as post-surgery ileus or surgical wound infection, among others, showed no significant differences (Table 3).
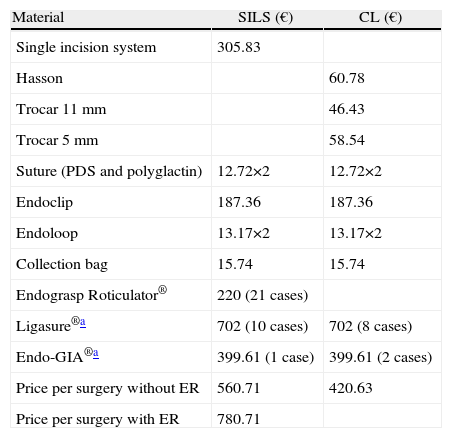
The cost, depending on the type of technique used, was adjusted to the prices provided by the purchasing department of our hospital (Table 4), listing specified additional material used in some cases, depending on intra-operational circumstances.
Costs According to Technique.
| Material | SILS (€) | CL (€) |
| Single incision system | 305.83 | |
| Hasson | 60.78 | |
| Trocar 11mm | 46.43 | |
| Trocar 5mm | 58.54 | |
| Suture (PDS and polyglactin) | 12.72×2 | 12.72×2 |
| Endoclip | 187.36 | 187.36 |
| Endoloop | 13.17×2 | 13.17×2 |
| Collection bag | 15.74 | 15.74 |
| Endograsp Roticulator® | 220 (21 cases) | |
| Ligasure®a | 702 (10 cases) | 702 (8 cases) |
| Endo-GIA®a | 399.61 (1 case) | 399.61 (2 cases) |
| Price per surgery without ER | 560.71 | 420.63 |
| Price per surgery with ER | 780.71 |
ER: endograsp roticulator.
Post-surgery follow-up was performed between 6 and 24 months; there were 2 hernia cases for SILS, and none for CL. Only one case was correlated to surgical wound infection.
DiscussionSILS-based laparoscopic appendectomy arises in a context in which CL-based appendectomy was becoming the technique of choice compared to open appendectomy. Despite the latter being the gold standard for appendicitis treatment in recent years, new randomized prospective papers have been published in addition to practice guidelines clearly showing benefits from laparoscopic surgery,16–18 progressively leading to the change of option by most surgeons. Technological development, the urge to be less aggressive in the incisions and to improve esthetic results, along with the inherent concern of most surgeons, have boosted the development of SILS-based appendectomy. This technique may have some benefits over CL due to the smaller incision, resulting in an almost imperceptible scar for the patient. SILS as a novel technique has been the focus of all kinds of criticism, especially due to how complicated and expensive it is; this situation is similar to that which occurred with laparoscopic surgery when it emerged in the late 1980s.19 However, the latter is currently the gold standard technique in multiple surgeries. Our study included only patients without factors altering the implementation of the technique, such as obesity, complicated acute appendicitis or patients with previous abdominal surgery. From the results obtained, the patient population was found to be homogeneous for both groups.
Although the SILS-based appendectomy surgery time turned out to be greater than that for CL, no statistically significant differences were detected (P=.21), showing that this minimal difference was due to the increased time spent placing the single port, and during closure of the incision. Furthermore, the added difficulty of triangulation in the SILS technique that could prolong surgery was not as significant as almost 2/3 of the patients who underwent the SILS-based surgery (39) with straight forceps. This is due to the topographic characteristics of the appendix and its mesentery, which often have a plane perpendicular to the forceps, allowing work in parallel. Covidien roticulator grasping forceps were used when this appendix-mesentery plane was different®. Based on selection criteria, our study did not include complicated appendicitis. In some patients, we had difficulty with dissection, which can explain our complication rate. Some studies20 do not find statistically significant differences in complicated appendicitis with regard to surgery time. Other studies19,21 do find differences, however, not between uncomplicated appendicitis and appendicitis with normal characteristics. Our study showed a difference of about 5min between the two techniques; in clinical practice, this would have no impact on patient outcomes.
There was no difference in hospital stay; the two groups started oral intake at 5h after surgery and early mobilization between 6 and 8h after surgery. Although some series show greater post-surgery satisfaction with SILS-based surgery,16 post-surgery pain was significantly higher in this group (P=.004), coinciding with other authors.22–25 Pain was assessed using the VAS nursing record and the surgeon's assessment at discharge time, with the patient's postural movements, cough or Valsalva maneuver.
Although the sum of all wounds caused by trocars cannot be related to pain, it is important to take into account that the tissue injury of the abdominal wall in either of these 2 techniques would be virtually the same with regard to the extent or sum of lengths. The length of the incision with SILS is 2.5–3cm, and for CL with 3 trocars is approximately 2.6cm. Likewise, keep in mind that with SILS, only the aponeurosis is incised, while with CL muscles are traversed, incurring an increased risk of vascular damage, such as the epigastric arteries.26 The use of bladeless trocars could further reduce the rate of post-surgery pain in the CL group.
Higher complication rates in patients with complicated appendicitis have been described. In our study, the major complications are derived from gangrenous appendicitis or more operating time due to difficulty in dissection. The surgical wound infection rate, strictly following the diagnostic criteria established by CDC (erythema, wound pain or turbid serous or purulent content excretion), was 3.3%, and although high, it is similar to some studies described in the literature.16,27 Of the 4 cases observed (2 for SILS and 2 for CL), incidence was lower than that reported by other authors,28 and did not correlate with longer surgery time, difficulties in surgical procedure or contamination when removing the surgical specimen. It is known that the incidence of intra-abdominal abscess is higher in obese patients or those with complicated appendicitis; the study does not include this criteria. However, despite being uncomplicated appendicitis, we had 3 cases (2 for SILS and 1 for CL) that were associated with longer surgery time, difficulty with dissection, and greater manipulation of the surgical specimen.29 For the 3 cases observed, 2 corresponded to suppurative appendicitis and one gangrenous case; abundant intra-abdominal lavage was performed without leaving a drain. Thus, uncontrolled intra-abdominal lavage in the context of a difficult appendectomy (loosening of adhesions, thickened meso appendix, suppurating or gangrenous appendix, retrocecal or retroileal appendix) may predispose to a higher incidence of intra-abdominal abscesses.15
There were 2 cases of hernia, one due to surgical wound infection and the other one probably due to technical or intrinsic factors related to the patient; nevertheless, there were no statistically significant differences (P>.05).
Costs were significantly higher (P<.001) for SILS, due to the use of the Covidien SILS Port®, whose price was almost twice the cost of all 3 trocars used for CL, plus the Covidien roticulator endograsping forceps®.
In conclusion, SILS-based appendectomy is an effective, feasible, and safe procedure in selected patients with uncomplicated acute appendicitis. Post-surgery pain was higher than that in CL, though probably more objective measurement criteria are required. Long-term studies will be needed to demonstrate whether there are differences in the incidence of hernias between SILS and CL. Finally, SILS-based appendectomy is currently more expensive than CL, and long-term results will determine the future of this technique.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Villalobos Mori R, Escoll Rufino J, Herrerías González F, Mias Carballal MC, Escartin Arias A, Olsina Kissler JJ. Estudio comparativo prospectivo aleatorizado entre apendicectomía laparoscópica por puerto único y apendicectomía laparoscópica convencional. Cir Esp. 2014;472–477.
Part of this manuscript was presented at the 6th International Notes Wider (Barcelona, December 3-4, 2012): Natural orifice transluminal endoscopic surgery.