Familial adenomatous polyposis (FAP) is a genetic disease caused by a mutation of the APC gene (chromosome 5q21) that inactivates tumour suppressor genes (for example, p53 or DCC) and stimulates certain proto-oncogenes (for example, K-ras).1 Inheritance is autosomal dominant in 80% of patients, but 20% are due to spontaneous mutations. This pathology involves the development of hundreds of polyps in the large bowel and colorectal carcinoma in 100% of those affected, especially during the 3rd decade of life. Meanwhile, polyps appear with malignant degeneration in locations other than the colon: mainly the duodenum (3%–5%, the most frequent), thyroid (2%), pancreas (2%) and stomach (0.6%).1,2
Gardner Syndrome (GS) is defined by the association of FAP with desmoid tumours, osteomas of the skull, dental alterations, congenital hypertrophy of the retinal pigment epithelium or skin lesions (sebaceous cysts, lipomas, epidermoid cysts and fibromas).1–3 Its prevalence is 1/1000000 individuals.
We present the case of a 55-year-old male, whose brother who had undergone surgery for intestinal polyposis. At the age of 42, the patient started having episodes of self-limiting diarrhoea and rectal bleeding. After complete radiologic, endoscopic and genetic studies, and given the findings of intestinal, gastric, and duodenal polyposis, the presence of 2 osteomas (frontal bone and mandible) and sebaceous cysts, the patient was diagnosed with GS at another hospital.
The patient underwent total colectomy and ileorectal anastomosis with a J-pouch. The histopathologic study revealed multiple adenomatous polyps, moderately differentiated adenocarcinoma in a rectal polyp and metastasis in a neighbouring lymph node (pT1N1M0). The patient received adjuvant chemotherapy.
At the age of 52, the study of a biopsied residual polyp in the rectal mucosa was positive for adenocarcinoma. We performed an abdominoperineal resection with total mesorectal excision at our hospital (pT1N0M0).
At the age of 55, gastroscopy showed evidence of 2 polyps in the gastric antrum with histology for carcinoma in situ. In the duodenum, there were 3 tubular adenomas measuring 3–4mm, with moderate grade dysplasia (Spigelman stage II).
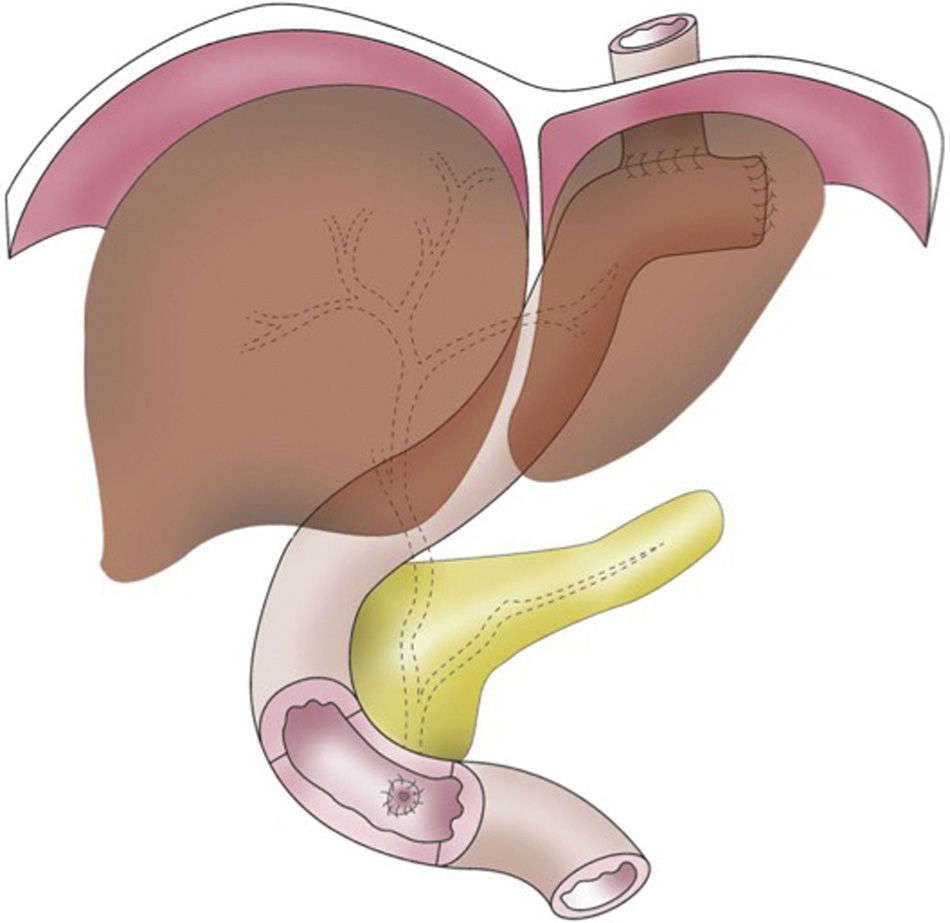
Total gastroduodenectomy with pancreatic preservation was carried out. After an extensive Kocher manoeuvre, the stomach was freed by dissecting the gastric vessels. Afterwards, the oesophagogastric junction and first jejunal loop were dissected. The duodenum was completely mobilised, while preserving the gastroduodenal artery, the entire pancreas and a minimal patch of mucosa (0.5cm) of the second portion of the duodenum, where the papilla was located. This had been previously identified by duodenostomy, and sphincterotomy was completed. After removing the stomach and duodenum en bloc, the jejunal loop was pulled up, and the digestive tract was reconstructed by means of mechanical end-to-side oesophagojejunal anastomosis. Then, an anastomosis was used to attach the minimal peripapillary duodenal remnant to the jejunum, in an end-to-side position 60cm from the oesophagojejunal anastomosis (Fig. 1). A Kehr drain tube was placed in the common bile duct.
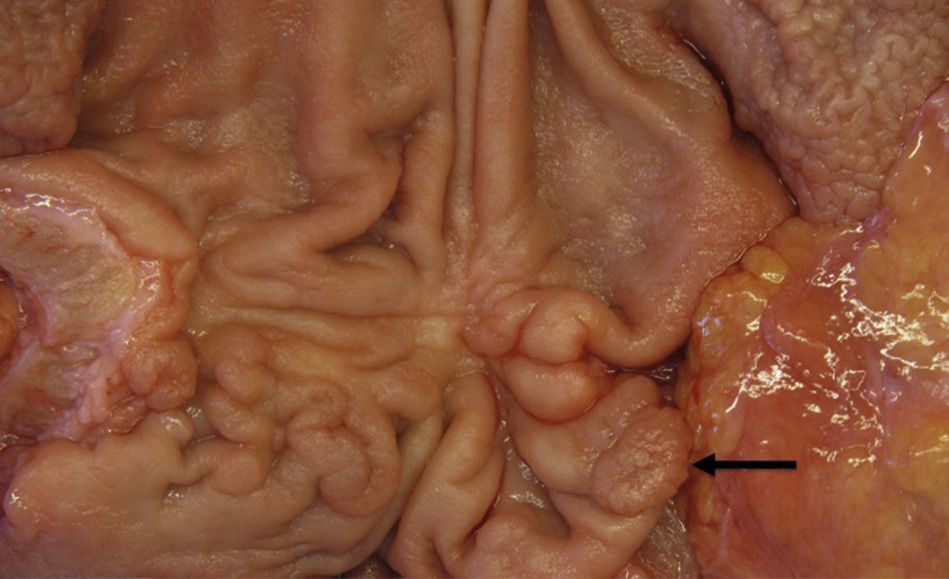
The pathology study revealed a pyloric tubular adenoma (0.8cm) with high grade dysplasia (pTisN0M0) (Fig. 2) and 3 tubular adenomas with moderate grade dysplasia in the first and second portions of the duodenum.
On the 14th day postop, the discharge from the abdominal drain was bilious, and an emergency computed tomography (CT scan) showed evidence of an intraperitoneal collection (22×10cm). The patient was re-operated on, and a partial dehiscence of the anastomosis between the papilla and the jejunum was identified. The dehiscence was sutured and drains were inserted. Subsequently, the patient's progress was uneventful, and he was discharged on the 53rd day post-op.
Gastric involvement in GS is frequent (18%), but malignant degeneration is rare (0.6%).4 Traditionally, duodenal polyposis with high grade dysplasia was treated by means of pancreaticoduodenectomy. Afterwards, with the advent of pancreas-preserving total duodenectomy (PPTD), the endocrine and exocrine pancreatic functions were able to be preserved. In addition, this technique reduces operative time, requires 2 anastomoses instead of 3, and avoids hepaticojejunostomy in an undilated bile tract and a pancreaticojejunal anastomosis in a soft pancreas with a thin Wirsung duct. It is also associated with less intraoperative bleeding and provides for better endoscopic follow-up of the remaining proximal intestine.5–8
In order to stage and make therapeutic decisions in duodenal polyposis, the Spigelman classification is used.5,8 This endoscopic-histological scale involves a scoring system with 4 items (number, size, histology and dysplasia of the polyps) that classifies duodenal involvement into 5 stages.1 It is currently accepted that Spigelman grades IV and III with high-grade dysplasia require duodenal resection. Grades I, II and III without high-grade dysplasia are treated by endoscopy.5 The duodenal involvement of our patient corresponded with a Spigelman grade II.According to this classification, it could have been treated endoscopically, while preserving the duodenum. The gastric involvement could also be treated endoscopically, but the malignant degeneration of a gastric polyp in the context of a patient with this preneoplastic disease led us to the decision to perform gastrectomy. After gastrectomy and reconstruction of the tract with a Roux-en-Y anastomosis, the duodenal stump was excluded, which meant that posterior endoscopic monitoring of the duodenal polyps would not be possible, and duodenal resection was therefore justified. In a review of the literature, we found no similar cases.
In conclusion, total gastroduodenectomy with pancreatic preservation is a complex technique that could be considered an alternative to pancreaticoduodenectomy in cases of gastric polyposis, malignant degeneration and concomitant duodenal polyposis in GS, as it provides for endoscopic control of the proximal portion of the remaining small bowel.
FundingNo funding was received for this publication.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Artiles Armas M, Marchena Gómez J, Kanouzi Masuh G, Ramírez Felipe JA. Gastroduodenectomía total con preservación pancreática para el tratamiento del síndrome de Gardner con poliposis gastroduodenal y degeneración maligna. Cir Esp. 2016;94:196–198.