To present a case series of 26 patients with postpartum hemorrhages treated with vascular ligations and analyze its efficiency for hemorrhagic control.
Material and methodsThis case series included patients with postpartum hemorrhages hospitalized in a high risk pregnancy unit in Sofia Feldman Hospital, Brazil, between January 2014 and May 2017, who were treated with vascular ligation techniques. The data were collected from patient medical records.
ResultsThe success rate in hemorrhagic control was 96.2% and hemorrhagic control of the single case in which vascular ligation failed was obtained with total hysterectomy. Hypovolemic shock occurred in 19.2% of the patients and blood transfusion was required in 26.9%. No patient required intensive care unit treatment. Hypertensive syndrome was the most prevalent comorbidity (46.2%). The main etiology was uterine atony (65.4%). Uterine and/or pelvic adhesions and uterine lacerations associated with fetal extraction occurred in 19.3% and 15.4% of cases, respectively.
ConclusionVascular ligations are efficient strategies for hemorrhagic control during cesarean sections and should be an integral part of the set of techniques that allow uterus preservation in the treatment of postpartum hemorrhage.
Presentar una serie de casos de 26 pacientes con hemorragias posparto tratadas con ligaduras vasculares y analizar su eficacia para el control hemorrágico.
Material y métodosEsta serie de casos incluyó a pacientes con hemorragias posparto hospitalizadas en la Unidad de Embarazo de Alto Riesgo del Hospital Sofia Feldman, Brasil, entre enero de 2014 y mayo de 2017, que fueron tratadas con técnicas de ligaduras vasculares. Los datos se obtuvieron de los registros médicos de las pacientes.
ResultadosLa tasa de éxito en el control hemorrágico fue del 96,2% y el control hemorrágico del caso único en el que falló la ligadura vascular, se obtuvo con histerectomía total. El choque hipovolémico ocurrió en el 19,2% de los pacientes y se requirió transfusión de sangre en el 26,9%. Ningún paciente requirió tratamiento en la Unidad de Cuidados Intensivos. El síndrome hipertensivo fue la comorbilidad con mayor prevalencia (46,2%). La principal etiología fue la atonía uterina (65,4%). Las adherencias uterinas y/o pélvicas y las laceraciones uterinas asociadas con la extracción fetal ocurrieron en el 19,3% y el 15,4% de los casos, respectivamente.
ConclusiónLas ligaduras vasculares son estrategias eficaces para el control hemorrágico durante la cesárea y deben integrar el conjunto de técnicas que permiten la preservación del útero en el tratamiento de la hemorragia posparto.
Postpartum hemorrhage (PPH) is defined as cumulative blood loss of 1000 milliliters (ml) or more, followed by signs or symptoms of hypovolemia, within 24h of birth.1 Currently, it is the most common serious complication at birth and the most frequent cause of severe maternal morbidity and preventable maternal mortality.2 When severe and resistant to conservative medical treatment, PPH is the largest worldwide cause of peripartum hysterectomy, even among young women with a desire for future fertility.3
In case of suspected PPH, the team, in a uniform manner, must act immediately. It is necessary to immediately inform the attending physician, provide two large peripheral venous accesses, quantifying blood loss, keep the patient warm and monitored. Collect blood typing, cross-testing, coagulogram, blood count and fibrinogen and after starting an immediate infusion of 20IU oxytocin, one gram of tranexamic acid, while performing a uterine compression maneuver. If bleeding persists, infuse heated crystalloids, not exceeding 2000ml, while revising the birth canal, intramuscular administration 0.2mg of methylergometrine (if not contraindicated) and reevaluating the condition. If bleeding is still active, introduce 600–800mcg of misoprostol sublingually, evaluate the second dose of tranexamic acid and methylergometrine. If active bleeding persists, collect blood gas and lactate and request blood transfusion. If bleeding still persists, invasive measures should be taken, such as intrauterine balloon tamponade, vascular ligations (VL), arterial embolization and hysterectomy.4
Several techniques for uterine conservation have already been developed, mainly VL, uterine compression sutures, intrauterine balloons, arterial embolization and intravascular balloons.5
O’Leary J.L. and O’Leary J.A. (1966) described the technique of bilateral ligation of the ascending branches of the uterine arteries in an article entitled “Uterine artery ligation in the control of intractable PPH”.6 Ever since, other techniques have been developed that also include the interruption of the vascular supply from other pelvic arteries that irrigate the uterus (cervical, ovarian, round ligament and internal iliac arteries), expanding the surgical strategies through VL in the treatment of PPH.7–10
This article aims to present a retrospective cohort study including cases of PPH treated with VL techniques and analyze its efficiency for hemorrhagic control. Success rates in uterus preservation and secondary outcomes are also evaluated.
Material and methodsA retrospective cohort study was conducted including cases of HPP seen at the High Risk Pregnancy Unit of Sofia Feldman Hospital between January 3, 2014 and May 22, 2017 that were treated with VL techniques. The project was previously approved by the Research Ethics Committee. The data were collected from patient medical records.
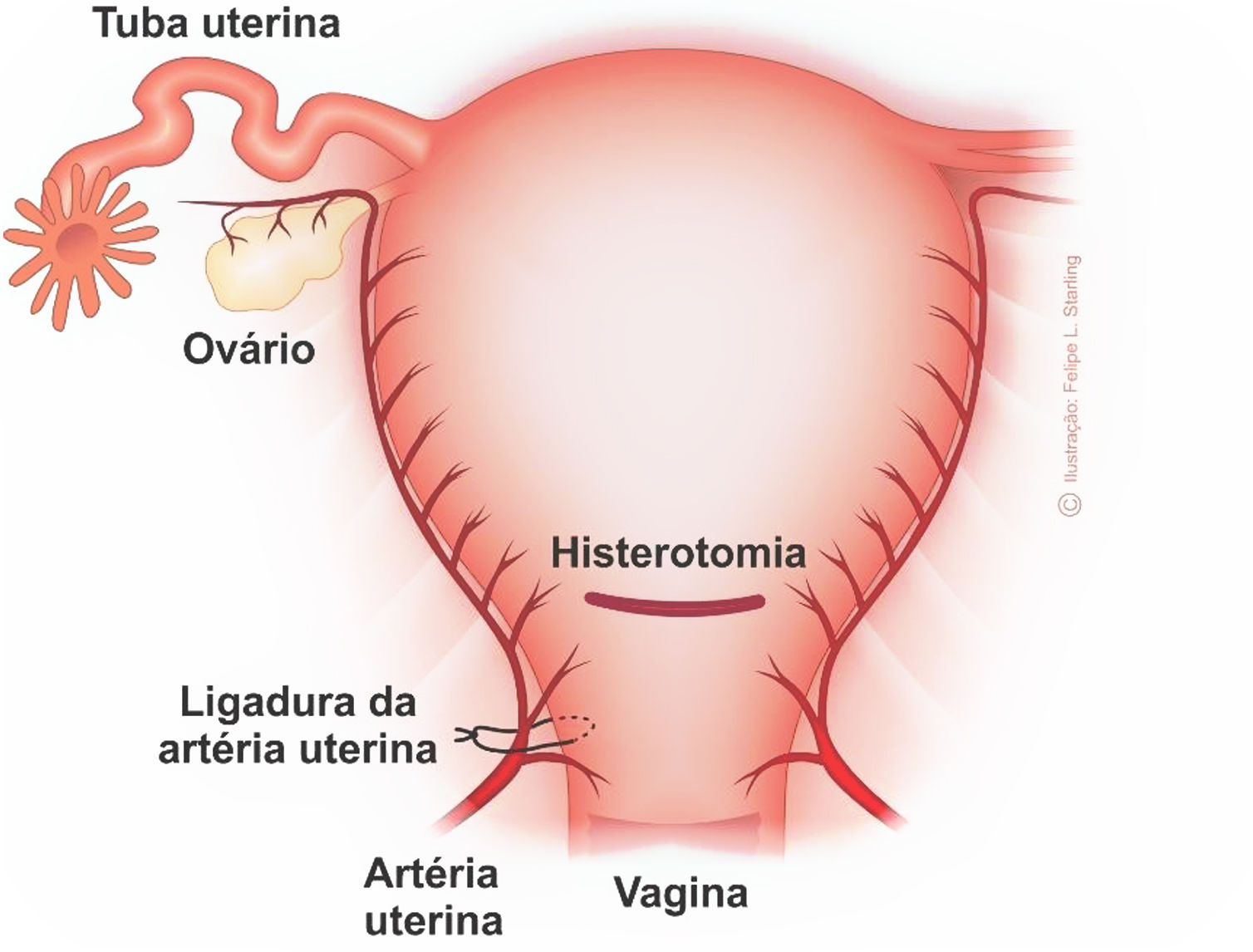
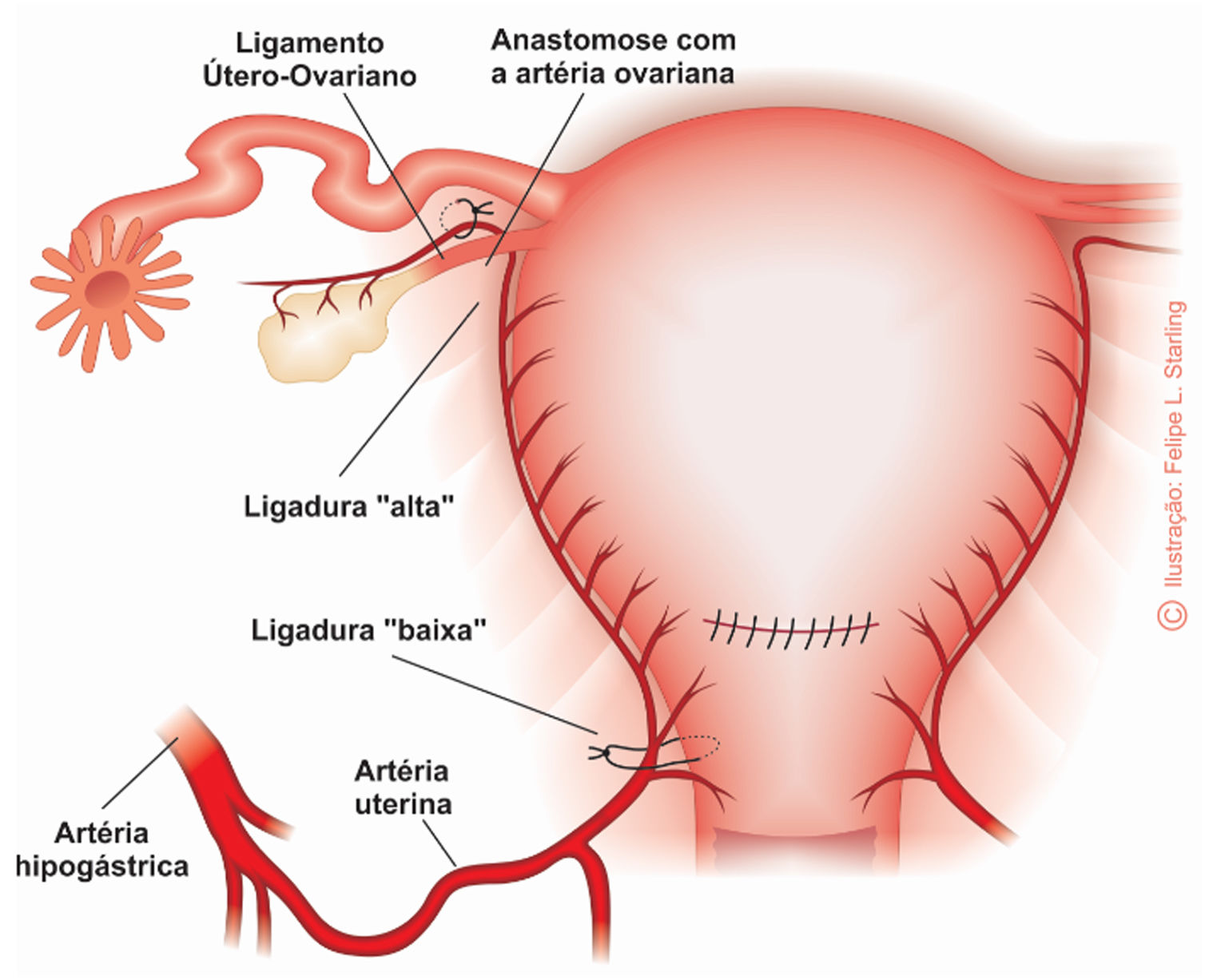
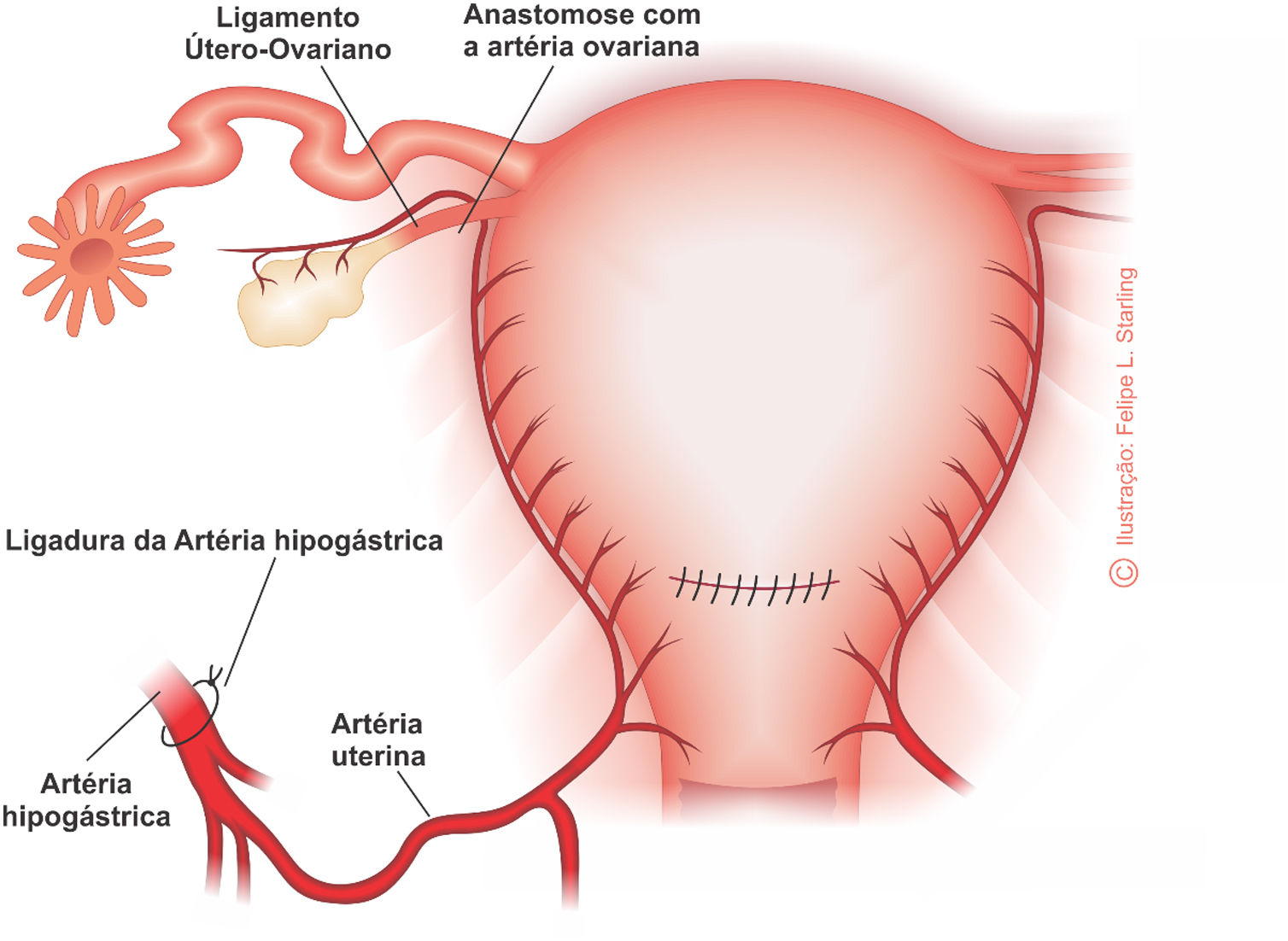
The VL techniques included bilateral ligation of the uterine artery ascending branches (O’Leary's technique – Fig. 1), bilateral ligation of the uterine arteries and the uterine-ovarian connections (Fig. 2) and bilateral ligation of the internal iliac arteries (Fig. 3).
Demographic and clinical variables included were maternal age estimated by ultrasound, risk factors for PPH and associated morbidities, use and time of use (in hours) of misoprostol or oxytocin before or during delivery, etiology of PPH, estimated blood loss (in ml), adjuvant therapies, shock index immediately, 12 and 24h after start of bleeding, blood transfusion, VL success rate and complications. Outcomes were also identified, and the proportions of patients who had hemorrhagic control were calculated according to the VL technique adopted and those who required hysterectomy.
All variables were inserted into the Epi-Info/Center for Disease Control and Prevention program for statistical analysis. Categorical variables had their absolute and relative frequencies calculated. Quantitative variables were studied by calculating their central tendency and dispersion measures.
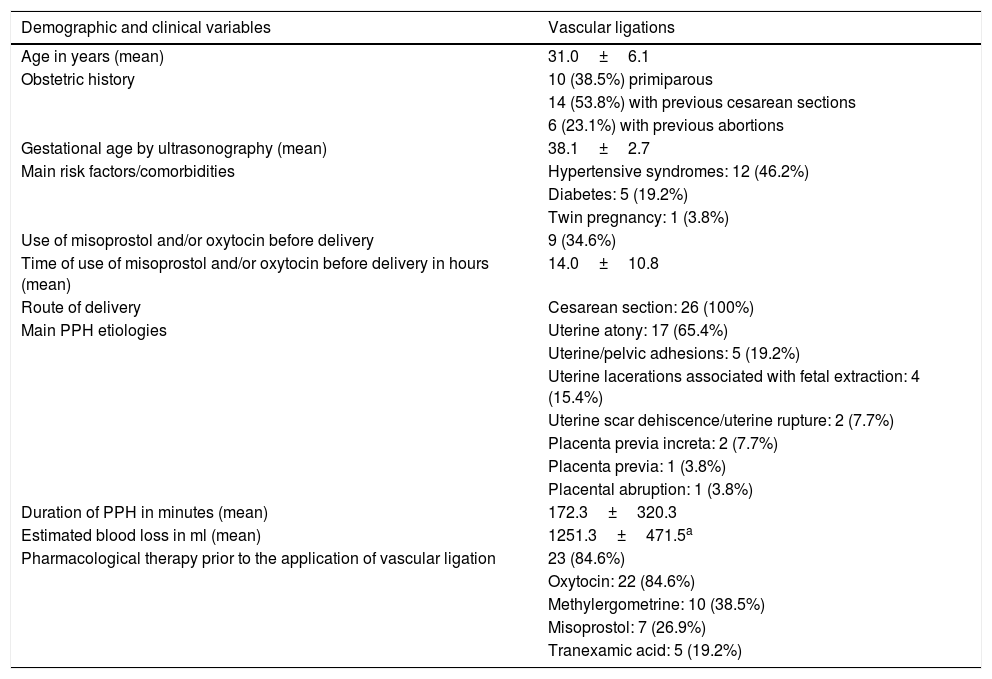
ResultsDuring this period, 38,107 births occurred in our center, 24.9 percent of which were cesarean sections, of which 484 patients evolved to PPH. Of the 484 cases of PPH, 354 (73,1%) showed good response to pharmacological treatment; 130 (26.9%) needed surgical treatment, of these 116 (89.2%) were treated with conservative surgical treatment and 14 (10.8%) needed hysterectomy. In the conservative surgical treatment group, 38 (32.7%) responded satisfactorily with intrauterine balloons; 26 (22.4%) responded satisfactorily to VL; 10 (8.6%) required B-Lynch compressive suture; 41 (35.3%) were treated with uterine VL associated with Hayman compressive suture; and one (0.9%) case were subjected to segmental myometrial excision.
The VL success rate was 96.2%. Of 26 patients, 10 (38.5%) were primiparous. Among the 16 (61.5%) who had given birth, the majority had previous cesarean section (14 patients – 53.8%) and only five (19.2%) had vaginal delivery. Twenty four (92.3%) patients had one or more risk factors/comorbidities, with hypertensive syndromes (12 patients – 46.2%) and diabetes (five patients – 19.2%) as the most frequent. Misoprostol and/or oxytocin were used in nine (34.6%) patients before or during labor and the mean time of use was 14.0±10.8h. All (100%) patients underwent cesarean section. The VL were performed during cesarean section in 24 (92.3%) patients and after completed cesarean section in two (7.7%), both with surgical reopening within six hours of birth. Some patients had more than one hemorrhagic etiology.
The most frequent PPH etiology was uterine atony (17 patients – 65.4%) followed by uterine/pelvic adhesions (five patients – 19.2%), uterine lacerations associated with fetal extraction (four patients – 15.4%), uterine rupture (two patients – 7.7%) and placenta previa increta (two patients – 7.7%).
One patient (3.8%) also presented placenta previa, but not accreta. In another patient (3.8%), atony was secondary to placental abruption. The mean duration of PPH was 172.3±320.3min. Blood loss was estimated in six patients and averaged 1251.3±471.5ml.
Bilateral ligation of the scending branches of the uterine arteries (O’Leary technique) was used in 22 (84.6%) patients. Among these 22 patients, one (3.8%) was also submitted to bilateral ligation of the internal iliac arteries. One patient (3.8%) underwent bilateral ligation of the uterine arteries and the uterine-ovarian connections. The three (11.5%) other patients underwent unilateral ligation of the uterine artery.
Five (19.2%) patients developed hypovolemic shock and seven (26.9%) needed blood transfusion. None required intensive care. In the only patient which there was no success of VL, hemorrhagic control was obtained by total hysterectomy.
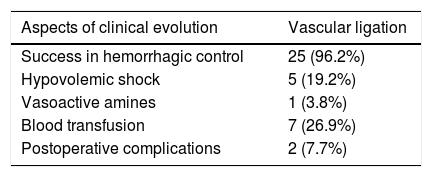
Two (7.7%) patients developed postoperative complications, one with headache after spinal anesthesia and another with abdominal wall abscess. Table 1 shows the main demographic and clinical variables and Table 2 details the clinical evolution of patients treated with VL.
Demographic and clinical variables of patients undergoing vascular ligation in the treatment of postpartum hemorrhage.
| Demographic and clinical variables | Vascular ligations |
|---|---|
| Age in years (mean) | 31.0±6.1 |
| Obstetric history | 10 (38.5%) primiparous |
| 14 (53.8%) with previous cesarean sections | |
| 6 (23.1%) with previous abortions | |
| Gestational age by ultrasonography (mean) | 38.1±2.7 |
| Main risk factors/comorbidities | Hypertensive syndromes: 12 (46.2%) |
| Diabetes: 5 (19.2%) | |
| Twin pregnancy: 1 (3.8%) | |
| Use of misoprostol and/or oxytocin before delivery | 9 (34.6%) |
| Time of use of misoprostol and/or oxytocin before delivery in hours (mean) | 14.0±10.8 |
| Route of delivery | Cesarean section: 26 (100%) |
| Main PPH etiologies | Uterine atony: 17 (65.4%) |
| Uterine/pelvic adhesions: 5 (19.2%) | |
| Uterine lacerations associated with fetal extraction: 4 (15.4%) | |
| Uterine scar dehiscence/uterine rupture: 2 (7.7%) | |
| Placenta previa increta: 2 (7.7%) | |
| Placenta previa: 1 (3.8%) | |
| Placental abruption: 1 (3.8%) | |
| Duration of PPH in minutes (mean) | 172.3±320.3 |
| Estimated blood loss in ml (mean) | 1251.3±471.5a |
| Pharmacological therapy prior to the application of vascular ligation | 23 (84.6%) |
| Oxytocin: 22 (84.6%) | |
| Methylergometrine: 10 (38.5%) | |
| Misoprostol: 7 (26.9%) | |
| Tranexamic acid: 5 (19.2%) |
Main aspects of the clinical evolution of patients submitted to vascular ligation in the treatment of postpartum hemorrhage.
| Aspects of clinical evolution | Vascular ligation |
|---|---|
| Success in hemorrhagic control | 25 (96.2%) |
| Hypovolemic shock | 5 (19.2%) |
| Vasoactive amines | 1 (3.8%) |
| Blood transfusion | 7 (26.9%) |
| Postoperative complications | 2 (7.7%) |
The main indications for VL in the treatment of PPH are hemorrhagic persistence after pharmacological therapy during cesarean section and failure or unavailability of radiological intervention after completed cesarean section or vaginal delivery.10
The vascularization of the uterus is complex, formed by anastomoses that come from both the upper part of the pelvis, irrigated by the internal iliac itself and the lower ones that ascend from the vaginal plexuses. Three main pedicles integrate the lower uterine blood supply. The superior is constituted by the uterine artery, one medial formed by the cervical artery and one inferior formed by the vaginal arteries. Different types of anastomoses occur between the upper, middle and lower pedicles, exhibit similar features and may be interconnected along the isthmus-vaginal edges or as a network of intramural anastomoses. A transmedial intern uterine anastomosis with caliber equivalent to the uterine artery may also be present. This anastomotic system between the uterine and vaginal arteries explains the failures, complications and hemodynamic changes related to the procedures of devascularization.11 Also, the irrigation in invasive low placentas usually originates from the upper vaginal vessels, mainly from the vaginal and internal pudendal arteries. These vessels are as calibrous as the uterine artery and markedly increase their volumes in cases of low placental invasion. These anatomical aspects explain the high failure rate of uterine artery ligation and/or embolization in anterior placenta percreta cases.12
In the original series of 90 cases of PPH, published by O’Leary J.L. and O’Leary J.A. (1974), the success rate of bilateral ligation of uterine artery ascending branches was 93.4%. Since hemorrhagic etiologies included uterine atony, placental abruption, Couvelaire uterus, afibrinogenemia, incisional bleeding, uterine lacerations, placenta previa, placenta accreta and bleeding at the placental site, they concluded that the simple bilateral ligation of these branches is a satisfactory technique for the control of PPH. The effect of uterine artery ligation is quickly visible. The uterus becomes pale and the bleeding reduces simultaneously. The uterus can often remain hypotonic, but hemorrhagic control is achieved. Recanalization of the vessel will occur, so the subsequent blood flow will be normal. Collateral circulation is enough to prevent tissue necrosis. In summary, the technique produces an effect similar to subtotal hysterectomy. Even in a Couvelaire uterus, the myometrium will contract and the bleeding will stop.13 This series of 26 cases goes in the line of these results because, despite the lower sample number, it included a significant diversity of hemorrhagic etiologies and obtained a similar success rate. The only case of failure was of a patient with two previous cesareans whose etiology were multiple adhesions in the uterus and pelvis. Hemorrhagic control was obtained with total hysterectomy and there were no postoperative complications.
In addition to the ligation of uterine arteries, bilateral stitches may be added to the mesosalpinx at the level of the uterine insertion of the utero-ovarian ligaments, in order to occlude the blood supply from the utero-ovarian connections.7 In our study, one of the cases was successfully treated using this technique. The patient had chronic hypertension associated with preeclampsia, two previous cesarean sections and one segmental placenta increta. The fetus was extracted by a transverse body hysterotomy, the vascular ligation of the ascending branch of the uterine artery and the uterine-ovarian connections was made, and then the placenta was removed and the uterus was preserved.
Other VL techniques include Tsirulnikov's triple ligation, AbdRabbo's step by step sequential ligation, the stepwise/step by step vascular ligation of Morel et al. and bilateral ligation of the internal iliac arteries. Tsirulnikov's triple ligation includes bilateral ligations of the ascending branches of the uterine arteries, the utero-ovarian connections and the arteries of the round ligament.8 In AbdRabbo's step-by-step sequential ligation, bilateral occlusion points include the ascending branch of the uterine artery, the cervicovaginal pedicle, and the infundibulopelvic ligament (ovarian pedicle). Despite the potential risk of surgical ovarian failure, the original series of 103 patients reported no complications.9 In the technique of Morel et al. (2011), the progressive sequence includes bilateral ligations of ascending branches of the uterine arteries, ligation and section of the round ligaments, ligation of the uterine-ovarian connections, ligation of the cervical-uterine arteries and, as a final step, ligation of the internal iliac arteries. The section of the round ligaments promotes extensive exposure, facilitating the execution of ligations.10 In this series of cases none of these techniques were applied.
The final method of surgical control through interruption of vascular supply is bilateral ligation of the internal iliac arteries. It should be reserved for hemodynamically stable patients, without coagulopathy, with low parity and with intense desire for new gestation, as a final effort to avoid hysterectomy. Indications include failure of other techniques that preserve the uterus or hemorrhages from the lower genital tract. Their success rates vary between 42 and 93%. Failure is associated with revascularization of the uterine artery, which is possible by anastomoses before the ligation points.7,10 Among the 26 patients studied, only one was submitted to ligation of the internal iliac arteries performed after ligation of the ascending branches of the uterine arteries. The etiology of PPH was prolongation of hysterotomy and injury of the uterine artery.
When evaluating the efficacy of Tsirulnikov's triple artery ligation, completed or not with Cho's uterine compression sutures, in 56 patients with PPH associated with cesarean section, Blanc et al. (2012) identified that placenta accreta was an independent factor and had a significant impact on the risk of failure.14 In our study, three patients had placenta previa. In one patient the placenta was marginal but not accreta. The other two patients had placenta increta, one with marginal and the other with central implantation. Bilateral ligation of the uterine arteries provided hemorrhagic control in these three patients and all of them progressed without postoperative complications. In the patient presenting marginal placenta increta, bilateral ligations of the utero-ovarian connections were also added.
Most patients studied had uterine atony as an isolated etiology of PPH. Two patients had uterine scar dehiscence with partial rupture of the uterus, one with a previous cesarean section and other with three. Four patients had PPH due to uterine trauma during fetal extraction and five due to uterine and pelvic adhesions. This may be explained by to the high percentage of patients with previous cesarean section and the exclusivity of this delivery route in the sample studied. Besides the fact that all study patients were treated with VL associated with cesarean sections, 87.5% of those who had already given birth had this type of delivery.
The estimation of blood loss is an important action in the treatment of PPH, and can be performed through visual estimation, weighing laparotomy pads or using collectors.4 However, this procedure was performed in only six of the 26 patients, which is a limitation of our study. The thread to be used in VL techniques must be absorbable. In our study, polyglactin was used in the 26 patients and the most used technique was the bilateral ligation of the ascending branch of the uterine arteries.10
Rapidity in treatment seems to be the factor that influences the most the efficacy of surgical management of PPH through VL. The choice of technique is usually more related to the experience of the obstetrician. The general recommendation is to start with bilateral ligation of the ascending branch of the uterine arteries (O’Leary technique), once this strategy will be effective in most cases.10
ConclusionsThis study provided an evaluation of the efficacy of VL in the control of PPH in its several etiologies. The results stand out for the high success rate and goes in the line of the studies of the first series of PPH cases treated with these techniques.
These facts indicate the importance to value the promotion and the evolution of surgical procedures that preserve the uterus in the treatment of PPH and to reflect on the knowledge and applicability of VL among care teams. VL are efficient surgical procedures for hemorrhagic control during cesarean sections and should integrate the set of techniques that preserve the uterus in the treatment of PPH when the conservative treatment options (pharmacological procedures, uterine balloon tamponade, uterine artery embolization) have failed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe authors declare that they have not financing for this article.
Conflicts of interestThe authors declare that they have not conflicts of interest for this article.