Churg-Strauss syndrome (CSS), also known as allergic granulomatous angiitis, is a systemic necrotizing vasculitis of the small and medium vessels. It typically occurs in conjunction with a history of asthma, eosinophilia, pulmonary infiltrates, and vasculitis, but cases without asthma have also been reported (1-2). CSS has rarely been reported in pediatric patients. Here, we report a nine-year-old boy with a possible diagnosis of CSS who presented with prominent pulmonary involvement accompanied by eosinophilia, rash, abdominal pain, and hepatomegaly but without anti-neutrophil cytoplasmic antibody (ANCA). The present case indicates that physicians should consider CSS when eosinophilia is noted in bronchoalveolar lavage, serum, or a tissue specimen. The clinical features and treatment for childhood CSS are reviewed.
CASE DESCRIPTIONA nine-year-old boy presented to our clinic with a one-week history of a productive cough, blood-streaked sputum and increased wheezing and a five-day history of fever. He complained of a one-year history of asthma, which had previously been treated with inhaled corticosteroids with the addition of montelukast. A BCG scar confirmed previous immunization against tuberculosis. He had no history of travel to helminth endemic areas and showed no weight loss. The boy was admitted because of the exacerbation of his symptoms and a chest radiograph revealing infiltration in both lungs in April 2011 (Figure 1A). The possibility of pneumonia was considered. After taking a five-day course of antibiotics, which included ceftriaxone for five days and azithromycin for three days, his respiratory symptoms and physical condition improved. However, several days later, his condition worsened, with cough, severe dyspnea, perioral cyanosis, urticaria-like lesions and vesicular rashes on the skin of both lower extremities, and purpura on the hands. Additionally, he began to experience lower back pain, whole body fatigue, pyknocardia, hepatomegaly, mild splenomegaly, hyperpyrexia, bilateral swelling of the parotid gland, submaxillary gland enlargement, discrete cervical lymphadenectasis, acute abdominal pain, chest pain, polyarthralgia, myalgia, and muscle weakness. His chest X-ray demonstrated worsening of the pulmonary infiltration (Figure 1B).
The initial laboratory examination at the time of admission showed a peripheral white blood cell (WBC) count of 14.9×109/L (normal: 4-10×109/L) with 30.7% eosinophils (normal: 0%–5%), 41.4% neutrophils, 21.6% lymphocytes, and a hemoglobin level of 138 g/L. Notably, 11 days later, his eosinophil count increased to 72.2% with an absolute eosinophil count of 27.9×109/ L and a WBC count of 38.6×109/L. The patient's erythrocyte sedimentation rate was 77 mm/hour, and immunoglobulin E (IgE) was elevated to 1258 KU/L (reference range: 0–100 KU/L). Tests for cytoplasmic (classical) antineutrophil cytoplasmic antibodies (c-ANCA) and peri-nuclear (protoplasmic-staining) antineutrophil cytoplasmic antibodies (p-ANCA) were negative. The levels of proteinase 3 (PR3) and myeloperoxidase (MPO) were normal. Computed tomography of the chest demonstrated interstitial infiltration. Cultures and/or stains of blood and sputum for viruses, fungi, acid-fast bacilli and bacteria were all negative. His parents declined bone marrow aspiration. A peripheral blood smear analysis produced normal results. His lactate dehydrogenase level was 235 U/L (normal, 120-300 U/L). Peripheral blood lymphocyte immunophenotyping indicated that his T-cell subsets were normal. All tumor markers and antinuclear antibodies were negative. Stool cultures for parasites and the results of serum analyses for anti-Schistosoma and anti-Sparganum species antibodies were all negative, and serum samples were negative for HIV and hepatitis B and C. No other significant laboratory abnormalities were found, including blood gas levels, hepatic, renal and myocardial function, coagulation function, antistreptolysin o, complement levels, 1-3-β-D glucosan (G test) and galactomannan (GM test). Cardiac evaluations, including electrocardiography and echocardiography, revealed no abnormalities.
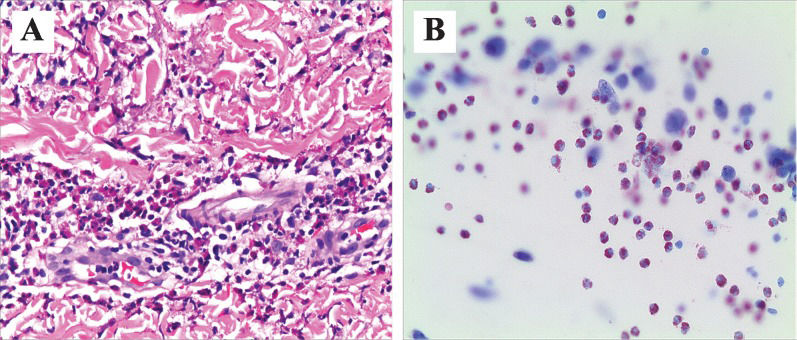
A skin biopsy specimen obtained from a rash on the patient's left lower extremity revealed a dermal infiltration with a considerable quantity of eosinophils (Figure 2A). Flexible bronchoscopy revealed moderate secretions. Bronchoalveolar lavage cytology revealed a predominance of in flammatory cells with 93% eosinophils, 2% macrophages (Figure 2B), and no microorganisms. A diagnosis of Churg-Strauss syndrome (CSS) was suggested. Corticosteroid therapy (intravenous methylprednisolone) was initiated at a dose of 80 mg daily (2.7 mg/kg/day), which improved the symptoms. Five days later corticosteroid (methylprednisolone tablets) was tapered at 48 mg daily (1.7 mg/kg/day). After two weeks of corticosteroids treatment, his condition stabilized and a peripheral eosinophil count decreased to 1.3%, WBC count decreased to 8.07×109/L, and the sedimentation rate decreased from 77 to 16 mm/hour. Chest computed tomography (Figure 1C) and x-ray (Figure 1D) revealed an improvement in pulmonary infiltration. Ten months later, the last flexible fiberoptic examination showed a clear airway, and the bronchoalveolar lavage cytology assay was normal. The corticosteroids were tapered without any systemic vasculitis over the following 11 months. At the latest follow up in late February 2012, the child was started on methylprednisolone tablets at a dose of 8 mg daily (0.3 mg/Kg/day) for two months.
DISCUSSIONChurg-Strauss syndrome was first described by Churg and Strauss in 1951 (3). The annual incidence of CSS in adults ranges between 0.5 and 3.1 cases per million. In children, the incidence of CSS is unknown but is thought to be very low. To our knowledge, only 44 pediatric patients with CSS have been reported, including our present case. The reported patients' ages ranged from 2 to 18 years (20 males and 24 females), with clinical manifestations rarely appearing before one year of age.
The rarity of CSS in childhood makes the diagnosis much more difficult. In 1990, the American College of Rheumatology (ACR) developed specific clinical criteria for the classification of CSS, which comprised a history of asthma, eosinophilia >10%, mononeuropathy/polyneuropathy, nonfixed pulmonary infiltrates, paranasal sinus abnormality, and extravascular eosinophils revealed by biopsy. The presence of at least four criteria yields a sensitivity of 85% and a specificity of 99.7% (4). Our patient met four of the six ACR criteria, namely, a history of asthma, eosinophilia >10%, pulmonary infiltrates, and a skin biopsy revealing extravascular eosinophils. However, although commonly used to diagnose CSS, the ACR criteria were not meant as diagnostic criteria and were instead meant to distinguish one form of vasculitis from another. Unfortunately, there have been no new diagnostic criteria for CSS. The differential diagnosis of CSS depends on the predominant clinical manifestations of each patient. For example, hypereosinophilic syndrome (HES) is difficult to distinguish from CSS because HES patients may have hypereosinophilia and end-organ damage, but characteristics such as asthma, atopic history and lung infiltrates support a diagnosis of CSS. Concomitant eosinophilia, asthma, and lung infiltrates may resemble certain parasitic infections, but stool cultures for parasites and serum analyses for antibodies were negative, and our patient had no history of travel to helminth endemic areas. Moreover, neoplastic disorders, particularly lymphomas, typically progress by the 11-month follow-up examination, but our patient's prompt response to treatment and persistent remission did not support the diagnosis of neoplastic disease. Nevertheless, a definite diagnosis was a challenge, and we still follow up with the patient in the event that evidence of a malignant disorder is discovered. The accurate diagnosis of CSS requires the presence of a constellation of findings that may have presented and evolved over a period of years rather than any individual pathological finding at one time point (5-7).
After reviewing the 43 cases of pediatric CSS in the literature, we outlined the clinical features of CSS in children and compared them with those in adults. The mortality rate of CSS is approximately 5% in adults (8) and is significantly worse in children, at 15.9% (7/44). In the past four years, 2 of the 11 pediatric CSS patients died due to pulmonary abscess and sepsis despite treatment with immunosuppressive drugs and intravenous immunoglobulin (1,9). The other predominant causes of death include heart failure, renal failure, cerebral failure, and gastrointestinal perforation/hemorrhage.
In our review, a history of asthma was found in 39 (88.6%) of the 44 children with CSS. Almost all CSS patients show a marked peripheral blood eosinophilia. The highest absolute eosinophilic count reported in all ages was 51.6×109/L and leukocytosis in leukemic ranges (65.8×109/L) (10). In our patient, the highest level of leukocytosis was 38.6×109/L with an absolute eosinophil count of 27.9×109/L (72.2%). Of the 44 pediatric CSS patients, 23 had high IgE levels and only 2 had normal IgE levels; the 19 remaining cases lacked relevant data. Our patient was negative for ANCAs, which is consistent with the literature demonstrating that only 5 of 23 patients were positive for ANCAs. However, the frequency of ANCA positivity is uncertain because the ANCA status was not available for the other 21 children. Two recent independent studies on large cohorts have found that ANCAs are present in only approximately 40% of adult CSS patients (11,12). It has been postulated (11,12) that CSS might encompass two clinical subsets or phenotypes: one is an ANCA-associated process that primarily has the features of small-vessel vasculitis (such as glomerulonephritis, mononeuritis multiplex, and purpura), and the other is ANCA-negative and more related to eosinophilic tissue infiltration that leads predominantly to pulmonary involvement and cardiopulmonary manifestations.
The clinical presentation of CSS is variable, and virtually any organ can be affected by the disease. In our review, pneumonia was the most common disorder (37/44 cases; 84.1%) followed by cutaneous manifestations (29/44, 65.9%). Skin manifestations were a common early presentation of CSS in children, which ranged from discrete to diffuse patchy, petechial or purpuric lesions and can be itchy, edematous, or tender. Paranasal sinus abnormalities were also common early presentations (24/37; 64.9%). Neurologic involvement, especially multiple mononeuropathy, was described in 40.5% (17/42) of children with CSS and has been reported in 36% of adult patients with CSS (8). Heart involvement was reported in 38.6% (17/44) of the children, gastrointestinal tract involvement in 34.1% (15/44) and kidney involvement in 13.6% (6/43). A number of reports reveal more subtle presentations of CSS, including swelling of the legs and feet, oral aphthae, hepatomegaly, hepatic venous outflow obstruction, respiratory distress, polyarthralgia, myalgia, polyneuropathies presenting as dysesthesia, muscle weakness, gait disturbances, venous thrombosis and pulmonary embolism, hemichorea, sudden painless loss of vision, retinal artery occlusions, discrete cervical lymphadenopathy, testicular pain, hypertension, seizures and necrosis of the toe tips.
Although the diagnosis of CSS is established mainly based on clinical observations, a tissue biopsy should be performed whenever possible (5,13). In addition to skin biopsies, the diagnosis of CSS is increasingly aided by transbronchial lung biopsy, open or thoracoscopic lung biopsy and, less frequently, by sinus biopsy, nasal mucosa biopsy or liver biopsy. A controlled study for the optimal treatment of CSS is not yet available because of the limited number of patients. The cornerstone of treatment for CSS remains corticosteroid therapy, but the response is variable. In patients with severe organ involvement or uncontrolled vasculitis symptoms, additional therapy with cyclophosphamide and/or azathioprine chlorambucil and methotrexate is required. The use of these various immuno-suppressive medications was effective in treating refractory CSS and in minimizing relapses. Plasma exchange was also used as an alternative to cytotoxic therapy, but prospective studies have not shown any difference in mortality or outcome (5). Moreover, intravenous immunoglobulin is a treatment option in patients with CSS with neuropathy (14). Rituximab, in fliximab, MMF (mycophenolate mofetil), and α-interferon are other therapeutic options used to treat CSS (15).
In conclusion, our present case emphasizes the importance of considering the diagnosis of CSS in children with uncontrolled pneumonia, hypereosinophilia, skin lesions, neuropathy, cardiomyopathy or hepatomegaly in conjunction with a previous history of asthma and sinusitis. Delayed diagnosis and severe organ involvement may worsen the prognosis and even lead to a fatal outcome. If started early, treatment with corticosteroids is often successful.
This study was partially supported by grants from the National Natural Science Foundation of China (Nos. 30872798, 81070004 and 81000765).
No potential conflict of interest was reported.
Jinling L wrote and revised the manuscript, collected data, performed the follow up, and served as an attending physician of the patient. Yingchun X served as an attending physician of the patient and participated in the data collection and writing. Zhimin C, the corresponding author, was responsible for the structure of the manuscript and the design of the treatment and follow up. Xuefeng X participated in writing the manuscript and constructed the figures. Meiping L co-designed the patient's treatment scheme and served as an attending physician of the patient. Yingshuo W participated in data collection and writing. Yunlian Z participated in data collection and follow up. Weizhong G analyzed the skin biopsy specimens and bronchoalveolar lavage fluid.