Pulmonary embolisms occur as a wide spectrum ranging from clinically asymptomatic thrombi to massive thrombi that lead to cardiogenic shock. The purpose of this study was to determine the associations of thrombus localization with risk factors, accompanying disorders, D-dimer levels and the red blood cell distribution width in patients with pulmonary embolism.
MATERIAL AND METHODS:In 148 patients diagnosed with pulmonary embolism, the presence and anatomical localization of the thrombus were assessed via computed tomographic pulmonary angiography. The accompanying disorders, risk factors, serum D-dimer levels, and red blood cell distribution width of the patients were retrospectively evaluated. ClinicalTrials.gov: NCT02388841.
RESULTS:The mean age of the patients was 54±16.0 years, and 48 patients were ≥65 years of age. The most frequent accompanying disorders were chronic obstructive pulmonary disease (22%) and malignancy (10.1%), and the most frequent risk factors were recent operation (14.1%) and immobilization (18.2%). Thrombi were most frequently observed in the right pulmonary artery (37.8%). In 31% of the patients, the thrombus was localized to the main pulmonary arteries. Immobile patients exhibited a higher proportion of thrombi in the main pulmonary arteries than mobile patients. The mean D-dimer level and the mean red blood cell distribution width in the patients with thrombi in the main pulmonary arteries were higher than those in the patients with thrombi in more distal pulmonary arterial branches.
CONCLUSION:Significant associations of proximally localized thrombi with immobilization, the D-dimer levels, and the red blood cell distribution width were observed.
Pulmonary embolism (PE) is a serious cardiopulmonary disorder caused by the partial or complete obstruction of the pulmonary arterial bed by a thrombus formed in the systemic veins. PE is thought result from interactions between the patient and risk factors 1–3. In cases of suspected PE, clinical, laboratory, and radiological findings should be carefully studied. Because the clinical findings of PE are non-specific, objective diagnostic tests are required for its diagnosis 4. Computed tomographic pulmonary angiography (CTPA) is increasingly being used as the first investigation for suspected PE. The extent of a PE is commonly expressed by indicating the anatomical level of the most proximal vessel affected by a thrombus 5. For a definitive diagnosis of suspected PE, the D-dimer level is one factor that should be determined. Plasma D-dimer measurement provides information about fibrin degradation fragments following fibrinolysis. D-dimer assays have low specificity but high sensitivity and negative predictive value in most patients with suspected thromboemboli 6. The red cell distribution width (RDW) is a quantitative indicator of the variability in the size of red blood cells. This parameter, which can be easily obtained from a full blood count, is accepted as an indicator of ineffective red cell production 7. Some studies have suggested that the RDW may be associated with cardiovascular and pulmonary diseases, including PE 8–13.
The purpose of this study was to determine the associations of thrombus localization with risk factors, accompanying disorders, D-dimer levels and the RDW in patients with PE.
MATERIAL AND METHODSStudy designThe data from CTPA confirmed the presence of PE in 148 patients in the Clinic of Chest Diseases of the Medical School of Yüzüncü Yil University, Van, Turkey, between January 2012 and August 2014; these patients were retrospectively studied. The patients' accompanying disorders, risk factors, D-dimer dose administered on the same day as the CTPA exam and RDW were noted. Patients with a history of hospitalization for reasons other than surgery, such as pneumonia, sepsis, Brucellosis, and encephalitis, bedridden patients, such as those with hemiplegia, and patients who were immobilized long-term (>72 hours) after surgery were included in the immobilized group.
Patients who received a diagnosis of PE without a CTPA exam and 6 patients whose hemoglobin levels below 11 g/dL were not included in this study.
Computed tomographic pulmonary angiographyThe thoracic CT scans were performed using a 16-detector multi-sectional CT scanner (Somatom Emotion 16-slice; CT2012E-Siemens AG, Berlin and München, Germany) with intravenously injected contrast agent while the patients held their breath. Contrast-enhanced images were obtained 50–70 sec after the IV administration of 120 ml of the ionic iodinated contrast agent iodixanol (Visipaque 320 mg/100 ml, Opakim) using a power injector at a rate of 2 ml/sec.
The following parameters were used: 120–130 Kilovolt (kV), 80–120 (effective mA), 0.6 sec (rotation time), 16 mm×1.2 mm (acquisition), 1.2 mm (slice collimation), 5.0–3.0 (slice width), 0.80 (pitch factor), 5.0 mm (increment), and 512×512 (matrix).
D-dimer testThe blood specimens from the patients were evaluated in the Clinical Haematology Laboratory. The D-dimer levels were measured via a latex-enhanced photometric method (Sta Compact, Dade Behring, Marburg, Germany) using D-dimer kits.
Red blood cell distribution widthThe RDW was determined using whole blood specimens. The hematological analyses were performed using a Coulter LH 750 Complete Blood Count device (Beckman Coulter, Fullerton, CA, USA).
The study was planned according to the Declaration of Helsinki and the rules of the Hospital Ethics Committee.
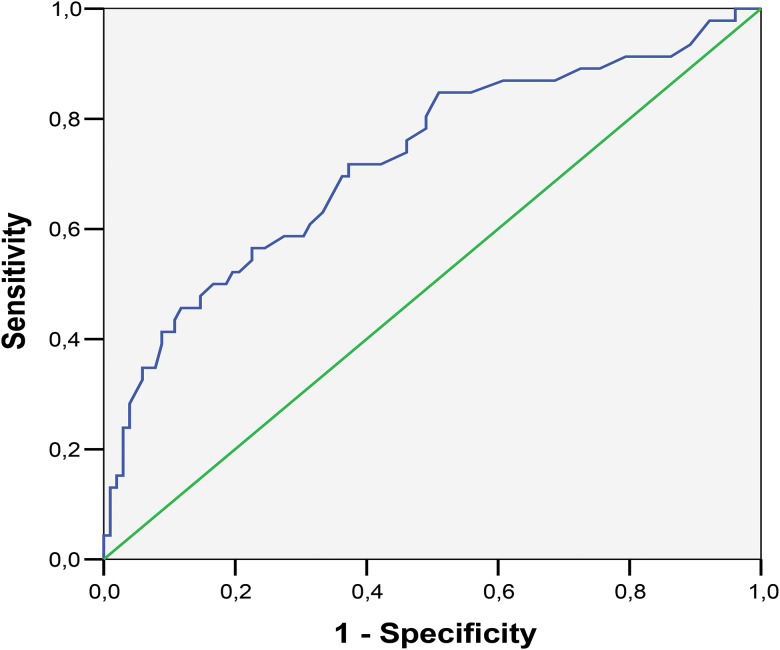
Statistical analysisDescriptive statistics are presented as frequencies and percentages for categorical data and as means and standard deviations for numerical data. Comparisons between two independent groups were conducted using Mann-Whitney U tests, and chi-square tests were used for non-normally distributed numerical and categorical variables. Pairwise Pearson correlations were utilized to estimate the linear relationships between the characteristics. Receiver operating characteristic (ROC) curve analysis was utilized to determine the optimum cutoff level for the association of RDW with a thrombus in the MPAs. All statistical calculations were performed using SAS version 9.3 (SAS, 2014). The results were considered to be statistically significant when the p-value was <0.05.
RESULTSThis study included 148 patients with PE as confirmed by CTPA. Of these patients, 83 (56%) were female, and 65 (43.9%) were male. The mean age of the patients was 54±16.8 years, and the age range was 18 to 81 years. Immobilization (18.2%) and recent operation (14.1%) were the most frequently identified risk factors. The most frequent comorbidity was chronic obstructive pulmonary disease (COPD). The thrombi were localized to the right pulmonary artery (PA) in 56 (37.8%) patients, in the left PA in 26 (17.5%) patients, and in the bilateral PAs in 66 (44.5%) patients (Table 1). When the anatomical level of the most proximal vessel affected by a thrombus was assessed by CTPA, a thrombus was observed in the main PAs (MPAs) in 46 (31%) patients and in the lobar, segmental, and/or subsegmental arteries in 102 (68.9%) patients. Among the patients with a thrombus in the MPAs and those with a distal thrombus, 34% and 30% were over 65 years of age, respectively (Table 2).
Distribution of the characteristics of pulmonary embolism patients according to thrombus localization.
| Right pulmonary arteries (n=56) | Left pulmonary arteries (n=26) | Bilateral pulmonary arteries (n=66) | p-value | |
|---|---|---|---|---|
| Mean age (years) | 50.9±18.3 | 53.3±17.0 | 56.561±15.3 | p>0.05 |
| Female/male | 36/20 | 15/11 | 32/34 | p<0.05 |
| Age over 65 years | 13 (%23) | 11 (%42) | 24 (%36) | p>0.05 |
| COPD | 10 (%17) | 8 (%30) | 15 (%22) | p>0.05 |
| Malignancy | 7 (%12) | 2 (%0.7) | 6 (%0.9) | p<0.05 |
| Immobilization | 9 (%16) | 5 (%19) | 13 (%19) | p>0.05 |
| Surgery | 6 (%10) | 2 (%0.7) | 13 (%19) | p<0.05 |
| D-dimer levels | 3.2±6.8 | 4.2±5.3 | 6.2±7.07 | p>0.05 |
| RDW | 15.5±3.05 | 15.5±2.8 | 15.8242±2.4 | p>0.05 |
Abbreviations: COPD: chronic obstructive pulmonary disease; RDW: red blood cell distribution width.
Distribution of the characteristics of pulmonary embolism patients according to the localization of the thrombi in the most proximal level of the main pulmonary artery and other arterial branches as confirmed by computed tomographic pulmonary angiography.
| Thrombus in main pulmonary arteries (n=46) | Thrombus in lobar, segmental and subsegmental arteries (n=102) | p-value | |
|---|---|---|---|
| Mean age (years) | 56.7±16.5 | 52.5±17.1 | p >0.05 |
| Female/male | 25/21 | 58/44 | p >0.05 |
| Age over 65 years | 16 (%34) | 32 (%30) | p >0.05 |
| COPD | 8 (%17) | 25 (%24) | p >0.05 |
| Malignancy | 5 (%10) | 10 (%9.8) | p >0.05 |
| Immobilization | 14 (%30) | 13 (%12) | p <0.05 |
| Surgery | 4 (%0.8) | 17 (%16.6) | p <0.05 |
| D-dimer levels | 8.6±8.4 | 3.0±0.55 | p <0.05 |
| RDW | 17.3±2.09 | 14.9±2.07 | p <0.05 |
Abbreviations: COPD: chronic obstructive pulmonary disease; RDW: red blood cell distribution width.
The percentage of thrombi in the MPAs was greater in immobilized patients (30% vs. 12%, p<0.05), and the percentage of thrombi in the lobar, segmental, and/or subsegmental arteries was higher in the patients with a history of recent operation (0.8% vs. 16.6%, p<0.05) (Table 2).
The mean D-dimer level was higher in the patients with thrombus in the MPAs (8.6±8.4) than in the patients with thrombus in the lobar, segmental, and/or subsegmental arteries (3.0±0.55) (p<0.05), and this level was higher in patients with bilateral thrombi than in patients with unilateral thrombi (p<0.05).
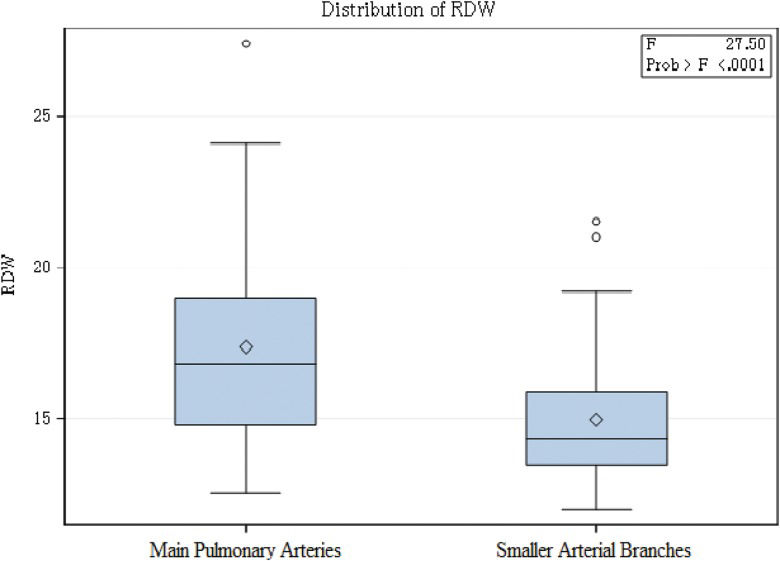
The RDW was significantly different between the group with thrombi in the MPAs and the group with thrombi in smaller arterial branches (p<0.001) (Table 2). The RDW of patients with MPA thrombi was greater than that of patients with thrombi in the smaller arterial branches (Figure 1).
The mean RDW was higher in the cases with thrombus in the MPAs (17.3±2.09) than in those with thrombus in smaller arterial branches (14.9±2.07) (p<0.05) (Table 2). ROC curve analysis revealed an area under the curve (AUC) of 0.72 with a 95% CI of 0.63–0.81. Thus, we identified an RDW cutoff value of 15.25% in the absence of MPA thrombi. This cutoff value displayed a sensitivity of 69.6% and a specificity of 62.7% (Figure 2).
DISCUSSIONPE is often caused by the partial or complete obstruction of blood flow in the pulmonary arterial bed by a thrombus formed in the systemic veins. When anatomically evaluated, PE occurs as a large spectrum ranging from non-massive asymptomatic thrombi 14 to massive thrombi that cause shock or cardiopulmonary arrest 15.
According to studies of the anatomical localizations of thrombi, thrombi are localized on the right, the left, and bilaterally in 36%, 18%, and 45% of cases, respectively 16,17. Regarding the numbers of thrombi, 65% of cases exhibit multiple 3–6 thrombi 17. Şimşek et al. 18 reported that thrombi were localized to the PAs of both lungs in 70.7% of their cases and in the PA of a single lung in 29.3% of their cases; he majority of the unilateral thrombi were localized to the right lung (60.5%). In our study, the thrombi were localized to the right PA in 37.8% of the cases and in the bilateral PAs in 44.5% of the cases.
Regarding the proximal localization of thrombi, in our study, the thrombus was localized in the MPAs in 46 (31%) and in the lobar, segmental, and/or subsegmental arteries in 102 (68.9%) of our patients. Gülcü et al. 19 examined 31 cases and confirmed via CTPA that the thrombi were localized to the MPAs in 30.8% of the patients. Şen et al. 20 detected an MPA-localized thrombus in 30% of their 172 cases. Perrier et al. 21 reported an MPA-localized thrombus in 32% of their series.
According to The International Cooperative Pulmonary Embolism Registry 22, the prognostic factors related to PE are age over 70 years, malignancy, congestive heart failure, and chronic respiratory insufficiency. In our study, the most frequently encountered accompanying disorders were COPD (22.2%) and malignancy (10.1%).
PE has been found to be associated with advanced age-related conditions that predispose patients to thrombosis, such as congestive heart failure, hip fractures, and stroke, increased coagulation potential, and limited mobility (23,24). In our study, 48 (32.4%) of the patients were 65 years old or older, but there was no association between age and thrombus localization (p>0.05). The mean age of the patients with a thrombus in the MPAs was higher, but this difference was not significant (p>0.05). Among the risk factors, long-term immobilization and recent operation were associated with markedly increased risk of PE. Regarding the risk factors for PE, Gülcü et al. 19 reported immobilization in 41.9% and recent surgery in 32.3% of their patients. In our study, we identified the risk factors of immobilization in 18.2% and recent surgery in 14.1% of our patients. A thrombus was more frequently localized to the MAPs in the immobile patients and was more frequently observed on the right side in the patients with a history of recent surgery. It has been reported that there is a strong association between the D-dimer levels and thrombus localization and that the D-dimer levels may differentiate patients with segmental and larger thrombi from those with subsegmental thrombi 25. Another study reported that the serum D-dimer level is higher in patients with proximally localized thrombi than in patients with distally localized thrombi, but this difference was not significant 26. Ghanima et al. 27 reported a significant association between the serum D-dimer level and the most proximal localization of the thrombus. In our study, we observed a significant correlation between thrombus localization and the serum D-dimer level. Furthermore, we determined that the mean D-dimer levels were higher in patients with MPA-localized thrombus than in patients with thrombus in other arterial branches.
Some studies have suggested that RDW may be associated with cardiovascular 8–11 and pulmonary diseases 12,13. Two studies have determined the RDW in patients with PE. Both of these studies found that a higher RDW, i.e., anisocytosis, is an independent predictor of early PE-related mortality 13,28. Recently, RDW has been associated with venous thromboembolism in two case–control studies 29,30. In our study, we found that the RDW was higher among the PE patients and that there was a significant association between the RDW and thrombus localization. The mean RDW was significantly higher in the patients with an MPA-localized thrombus. Our findings suggest that the RDW may differentiate patients with MPA-localized thrombi from those with thrombi in other arterial branches in clinical settings.
Our study contains some limitations. This was a retrospective study that was performed by screening the medical files of PE patients in our hospital computer system. The data for some patients were found to be insufficient, which caused us to study a limited number of patients. Another limiting factor was the selection of only CTPA-positive PE patients and the consequent exclusion of patients who were diagnosed with PE using methods other than CTPA.
In conclusion, we found a thrombus localized to the MPAs in 31% of our PE patients. Furthermore, we determined that a proximal thrombus localization was significantly associated with immobilization, and the D-dimer levels, and the RDW.
AUTHOR CONTRIBUTIONSSunnetcioglu A conceived the study; participated in its design, coordination, drafting, and revision; collected the data; and performed the literature search. Sertogullarindan B supervised the study, collected and analyzed the data; participated in the drafting of the manuscript; and performed the literature search. Ozbay B, Asker S and Ekin S collected and analyzed the data.
No potential conflict of interest was reported.